Abstract
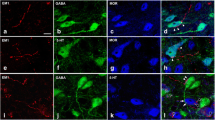
Opioids are often first-line analgesics in pain therapy. However, prolonged use of opioids causes paradoxical pain, termed “opioid-induced hyperalgesia (OIH).” The infralimbic medial prefrontal cortex (IL-mPFC) has been suggested to be critical in inflammatory and neuropathic pain processing through its dynamic output from layer V pyramidal neurons. Whether OIH condition induces excitability changes of these output neurons and what mechanisms underlie these changes remains elusive. Here, with combination of patch-clamp recording, immunohistochemistry, as well as optogenetics, we revealed that IL-mPFC layer V pyramidal neurons exhibited hyperexcitability together with higher input resistance. In line with this, optogenetic and chemogenetic activation of these neurons aggravates behavioral hyperalgesia in male OIH rats. Inhibition of these neurons alleviates hyperalgesia in male OIH rats but exerts an opposite effect in male control rats. Electrophysiological analysis of hyperpolarization-activated cation current (Ih) demonstrated that decreased Ih is a prerequisite for the hyperexcitability of IL-mPFC output neurons. This decreased Ih was accompanied by a decrease in HCN1, but not HCN2, immunolabeling, in these neurons. In contrast, the application of HCN channel blocker increased the hyperalgesia threshold of male OIH rats. Consequently, we identified an HCN-channel-dependent hyperexcitability of IL-mPFC output neurons, which governs the development and maintenance of OIH in male rats.











Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this published article.
References
Higgins C, Smith BH, Matthews K (2019) Evidence of opioid-induced hyperalgesia in clinical populations after chronic opioid exposure: a systematic review and meta-analysis. Br J Anaesth 122:e114–e126. https://doi.org/10.1016/j.bja.2018.09.019
Compton P, Canamar CP, Hillhouse M, Ling W (2012) Hyperalgesia in heroin dependent patients and the effects of opioid substitution therapy. J Pain 13:401–409. https://doi.org/10.1016/j.jpain.2012.01.001
Compton P, Charuvastra VC, Ling W (2001) Pain intolerance in opioid-maintained former opiate addicts: effect of long-acting maintenance agent. Drug Alcohol Depend 63:139–146. https://doi.org/10.1016/S0376-8716(00)00200-3
Lauber E, Filice F, Schwaller B (2016) Prenatal valproate exposure differentially affects parvalbumin-expressing neurons and related circuits in the cortex and striatum of mice. Front Mol Neurosci 9:150. https://doi.org/10.3389/fnmol.2016.00150
Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L (2011) A comprehensive review of opioid-induced hyperalgesia. Pain Physician 14:145–161
Mauermann E, Filitz J, Dolder P, Rentsch KM, Bandschapp O, Ruppen W (2016) Does fentanyl lead to opioid-induced hyperalgesia in healthy volunteers?: a double-blind, randomized, crossover trial. Anesthesiology 124:453–463. https://doi.org/10.1097/ALN.0000000000000976
Mercadante S, Arcuri E, Santoni A (2019) Opioid-induced tolerance and hyperalgesia. CNS Drugs 33:943–955. https://doi.org/10.1007/s40263-019-00660-0
Zhang P, Perez OC, Southey BR, Sweedler JV, Pradhan AA, Rodriguez-Zas SL (2021) Alternative splicing mechanisms underlying opioid-induced hyperalgesia. Genes (Basel) 12:1570. https://doi.org/10.3390/genes12101570
Wilson SH, Hellman KM, James D, Adler AC, Chandrakantan A (2021) Mechanisms, diagnosis, prevention and management of perioperative opioid-induced hyperalgesia. Pain Manag 11:405–417. https://doi.org/10.2217/pmt-2020-0105
Bourne S, Machado AG, Nagel SJ (2014) Basic anatomy and physiology of pain pathway. Neurosurg Clin N Am 25:629–638. https://doi.org/10.1016/j.nec.2014.06.001
Roeckel LA, Le Coz GM, Gavériaux-Ruff C, Simonin F (2016) Opioid-induced hyperalgesia: cellular and molecular mechanisms. Neuroscience 338:160–182. https://doi.org/10.1016/j.neuroscience.2016.06.029
Neugebauer V (2015) Amygdala pain mechanisms. Handb Exp Pharmacol 227:261–284. https://doi.org/10.1007/978-3-662-46450-2
Datta U, Kelley LK, Middleton JW, Gilpin NW (2020) Positive allosteric modulation of the cannabinoid type-1 receptor (CB1R) in periaqueductal gray (PAG) antagonizes anti-nociceptive and cellular effects of a mu-opioid receptor agonist in morphine-withdrawn rats. Psychopharmacology 237:3729–3739. https://doi.org/10.1007/s00213-020-05650-5
Hamlin AS, McNally GP, Osborne PB (2007) Induction of c-Fos and zif268 in the nociceptive amygdala parallel abstinence hyperalgesia in rats briefly exposed to morphine. Neuropharmacology 53:330–343. https://doi.org/10.1016/j.neuropharm.2007.05.017c
Li Z, Li C, Yin P, Wang ZJ, Luo F (2016) Inhibition of CaMKIIalpha in the central nucleus of amygdala attenuates fentanyl-induced hyperalgesia in rats. J Pharmacol Exp Ther 359:82–89. https://doi.org/10.1124/jpet.116.233817
Li Z, Yin P, Chen J, Jin S, Liu J, Luo F (2017) CaMKIIα may modulate fentanyl-induced hyperalgesia via a CeLC-PAG-RVM-spinal cord descending facilitative pain pathway in rats. PLoS One 12:e0177412. https://doi.org/10.1371/journal.pone.0177412
Mecca CM, Chao D, Yu G, Feng Y, Segel L, Zhang Z, Rodriguez-Garcia DM, Pawela CP, Hillard CJ, Hogan QH, Pan B (2021) Dynamic change of endocannabinoid signaling in the medial prefrontal cortex controls the development of depression after neuropathic pain. J Neurosci 41:7492–7508. https://doi.org/10.1523/JNEUROSCI.3135-20.2021
Yue L, Ma LY, Cui S, Liu FY, Yi M, Wan Y (2017) Brain-derived neurotrophic factor in the infralimbic cortex alleviates inflammatory pain. Neurosci Lett 655:7–13. https://doi.org/10.1016/j.neulet.2017.06.028
Kummer KK, Mitrić M, Kalpachidou T, Kress M (2020) The medial prefrontal cortex as a central hub for mental comorbidities associated with chronic pain. Int J Mol Sci 21:3440. https://doi.org/10.3390/ijms21103440
Radzicki D, Pollema-Mays SL, Sanz-Clemente A, Martina M (2017) Loss of M1 receptor dependent cholinergic excitation contributes to mPFC deactivation in neuropathic pain. J Neurosci 37:2292–2304. https://doi.org/10.1523/JNEUROSCI.1553-16.2017
Wu XB, Liang B, Gao YJ (2016) The increase of intrinsic excitability of layer V pyramidal cells in the prelimbic medial prefrontal cortex of adult mice after peripheral inflammation. Neurosci Lett 611:40–45. https://doi.org/10.1016/j.neulet.2015.11.030
Kiritoshi T, Neugebauer V (2018) Pathway-specific alterations of cortico-amygdala transmission in an arthritis pain model. ACS Chem Neurosci 9:2252–2261. https://doi.org/10.1021/acschemneuro.8b00022
Rose JE, Woolsey CN (1948) The orbitofrontal cortex and its connections with the mediodorsal nucleus in rabbit, sheep and cat. Res Publ Assoc Res Nerv Ment Dis 27:210–232
Preuss TM (1995) Do rats have prefrontal cortex? The rose-woolsey-akert program reconsidered. J Cogn Neurosci 7:1–24. https://doi.org/10.1162/jocn.1995.7.1.1
Notomi T, Shigemoto R (2004) Immunohistochemical localization of Ih channel subunits, HCN1-4, in the rat brain. J Comp Neurol 471:241–276. https://doi.org/10.1002/cne.11039
Van De Werd HJ, Rajkowska G, Evers P, Uylings HBM (2010) Cytoarchitectonic and chemoarchitectonic characterization of the prefrontal cortical areas in the mouse. Brain Struct Funct 214:339–353. https://doi.org/10.1007/s00429-010-0247-z
Cheriyan J, Kaushik MK, Ferreira AN, Sheets PL (2016) Specific targeting of the basolateral amygdala to projectionally defined pyramidal neurons in prelimbic and infralimbic cortex. eNeuro 3:ENEURO.0002-16. https://doi.org/10.1523/ENEURO.0002-16
Ferreira AN, Yousuf H, Dalton S, Sheets PL (2015) Highly differentiated cellular and circuit properties of infralimbic pyramidal neurons projecting to the periaqueductal gray and amygdala. Front Cell Neurosci 9:161. https://doi.org/10.3389/fncel.2015.00161
Ding W, You Z, Shen S, Yang J, Lim G, Doheny JT, Zhu S, Zhang Y et al (2018) Increased HCN channel activity in the gasserian ganglion contributes to trigeminal neuropathic pain. J Pain 19:626–634. https://doi.org/10.1016/j.jpain.2018.01.003
He JT, Li XY, Zhao X, Liu X (2019) Hyperpolarization-activated and cyclic nucleotide-gated channel proteins as emerging new targets in neuropathic pain. Rev Neurosci 30:639–649. https://doi.org/10.1515/revneuro-2018-0094
Grzelka K, Kurowski P, Gawlak M, Szulczyk P (2017) Noradrenaline modulates the membrane potential and holding current of medial prefrontal cortex pyramidal neurons via β 1-adrenergic receptors and HCN channels. Front Cell Neurosci 11:341. https://doi.org/10.3389/fncel.2017.00341
Cordeiro Matos S, Zamfir M, Longo G, Ribeiro-da-Silva A, Seguela P (2018) Noradrenergic fiber sprouting and altered transduction in neuropathic prefrontal cortex. Brain Struct Funct 223:1149–1164. https://doi.org/10.1007/s00429-017-1543-7
Cordeiro Matos S, Zhang Z, Séguéla P (2015) Peripheral neuropathy induces HCN channel dysfunction in pyramidal neurons of the medial prefrontal cortex. J Neurosci 35:13244–13256. https://doi.org/10.1523/JNEUROSCI.0799-15.2015
McDevitt DS, McKendrick G, Graziane NM (2021) Anterior cingulate cortex is necessary for spontaneous opioid withdrawal and withdrawal-induced hyperalgesia in male mice. Neuropsychopharmacology 46:1990–1999. https://doi.org/10.1038/s41386-021-01118-y
Chaplan SR, Guo HQ, Lee DH, Luo L, Liu C, Kuei C, Velumian AA, Butler MP et al (2003) Neuronal hyperpolarization activated pacemaker channels drive neuropathic pain. J Neurosci 23:1169–1178. https://doi.org/10.1523/JNEUROSCI.23-04-01169.2003
Cook DC, Goldstein PA (2021) Non-canonical molecular targets for novel analgesics: intracellular calcium and HCN channels. Curr Neuropharmacol 19:1937–1951. https://doi.org/10.2174/1570159X19666210119153047
Dini L, Lungo MD, Resta F, Melchiorre M, Spinelli V, Mannelli LDC, Ghelardini C, Laurino A et al (2018) Selective blockade of HCN1/HCN2 Channels as a potential pharmacological strategy against pain. Front Pharmacol 9:1252. https://doi.org/10.3389/fphar.2018.01252
Jiang YQ, Xing GG, Wang SL, Tu HY, Chi YN, Li J, Liu FY, Han JS et al (2008) Axonal accumulation of hyperpolarization-activated cyclic nucleotide-gated cation channels contributes to mechanical allodynia after peripheral nerve injury in rat. Pain 137:495–506. https://doi.org/10.1016/j.pain.2007.10.011
Resta F, Micheli L, Laurino A, Spinelli V, Mello T, Sartiani L, Mannelli LDC, Cerbai E et al (2018) Selective HCN1 block as a strategy to control oxaliplatin-induced neuropathy. Neuropharmacology 131:403–413. https://doi.org/10.1016/j.neuropharm.2018.01.014
Cho HJ, Staikopoulos V, Furness JB, Jennings EA (2009) Inflammation-induced increase in hyperpolarization-activated, cyclic nucleotide-gated channel protein in trigeminal ganglion neurons and the effect of buprenorphine. Neuroscience 162:453–461. https://doi.org/10.1016/j.neuroscience.2009.04.063
Célèrier E, Rivat C, Jun Y, Laulin JP, Larcher A, Reynier P, Simonnet G (2000) Long-lasting hyperalgesia induced by fentanyl in rats: preventive effect of ketamine. Anesthesiology 92:465–472. https://doi.org/10.1097/00000542-200002000-00029
Zissen MH, Zhang G, McKelvy A, Propst JT, Kendig JJ, Sweitzer SM (2007) Tolerance, opioid-induced allodynia and withdrawal associated allodynia in infant and young rats. Neuroscience 144:247–262. https://doi.org/10.1016/j.neuroscience.2006.08.078
Wang XX, Cui LL, Gan SF, Zhang ZR, Xiao J, Li CH, Luo F (2022) Inhibition of oligodendrocyte apoptosis in the prelimbic medial prefrontal cortex prevents fentanyl-induced hyperalgesia in rats. J Pain S1526–5900:00003–00007. https://doi.org/10.1016/j.jpain.2021.12.012
Cheriyan J, Sheets PL (2018) Altered excitability and local connectivity of mPFC-PAG neurons in a mouse model of neuropathic pain. J Neurosci 38:4829–4839. https://doi.org/10.1523/JNEUROSCI.2731-17.2018
Reiner DJ, Fredriksson I, Lofaro OM, Bossert JM, Shaham Y (2019) Relapse to opioid seeking in rat models: behavior, pharmacology and circuits. Neuropsychopharmacology 44:465–477. https://doi.org/10.1038/s41386-018-0234-2
Rogers JL, Ghee S, See RE (2008) The neural circuitry underlying reinstatement of heroin-seeking behavior in an animal model of relapse. Neuroscience 151:579–588. https://doi.org/10.1016/j.neuroscience.2007.10.012
Moorman DE, James MH, McGlinchey EM, Aston-Jones G (2015) Differential roles of medial prefrontal subregions in the regulation of drug seeking. Brain Res 1628:130–146. https://doi.org/10.1016/j.brainres.2014.12.024
Koppensteiner P, Galvin C, Ninan I (2019) Lack of experience-dependent intrinsic plasticity in the adolescent infralimbic medial prefrontal cortex. Synapse 73:e22090. https://doi.org/10.1002/syn.22090
Pena-Bravo JI, Reichel CM, Lavin A (2017) Abstinence from cocaine-induced conditioned place preference produces discrete changes in glutamatergic synapses onto deep layer 5/6 neurons from prelimbic and infralimbic cortices. eNeuro 4:ENEURO.0308-17. https://doi.org/10.1523/ENEURO.0308-17.2017
Peters J, Kalivas PW, Quirk GJ (2009) Extinction circuits for fear and addiction overlap in prefrontal cortex. Learn Mem 16:279–288. https://doi.org/10.1101/lm.1041309
David-Pereira A, Puga S, Gonçalves S, Amorim D, Silva C, Pertovaara A, Almeida A, Pinto-Ribeiro F (2016) Metabotropic glutamate 5 receptor in the infralimbic cortex contributes to descending pain facilitation in healthy and arthritic animals. Neuroscience 312:108–119. https://doi.org/10.1016/j.neuroscience.2015.10.060
Ji G, Neugebauer V (2011) Pain-related deactivation of medial prefrontal cortical neurons involves mGluR1 and GABA(A) receptors. J Neurophysiol 106:2642–2652. https://doi.org/10.1152/jn.00461.2011
Ji G, Neugebauer V (2014) CB1 augments mGluR5 function in medial prefrontal cortical neurons to inhibit amygdala hyperactivity in an arthritis pain model. Eur J Neurosci 39:455–466. https://doi.org/10.1111/ejn.12432
Shiers S, Pradhan G, Mwirigi J, Mejia G, Ahmad A, Kroener S, Price T (2018) Neuropathic pain creates an enduring prefrontal cortex dysfunction corrected by the type II diabetic drug metformin but not by gabapentin. J Neurosci 38:7337–7350. https://doi.org/10.1523/JNEUROSCI.0713-18.2018
McCormick DA, Shu Y, Hasenstaub A, Sanchez-Vives M, Badoual M, Bal T (2003) Persistent cortical activity: mechanisms of generation and effects on neuronal excitability. Cereb Cortex 13:1219–1231. https://doi.org/10.1093/cercor/bhg104
Yang L, Liu X, Yao K, Sun Y, Jiang F, Yan H, Mao P, Fan S et al (2019) HCN channel antagonist ZD7288 ameliorates neuropathic pain and associated depression. Brain Res 1717:204–213. https://doi.org/10.1016/j.brainres.2019.03.036
Ma Y, Chen J, Yu D, Wei B, Jin H, Zeng J, Liu X (2021) cAMP-PKA signaling is involved in regulation of spinal HCN channels function in diabetic neuropathic pain. Neurosci Lett 750:135763. https://doi.org/10.1016/j.neulet.2021.135763
Ramírez D, Zúñiga R, Concha G, Zúñiga L (2018) HCN channels: new therapeutic targets for pain treatment. Molecules 23:2094. https://doi.org/10.3390/molecules23092094
Lancon K, Qu C, Navratilova E, Porreca F, Seguela P (2021) Decreased dopaminergic inhibition of pyramidal neurons in anterior cingulate cortex maintains chronic neuropathic pain. Cell reports 37:109933. https://doi.org/10.1016/j.celrep.2021.109933
Ku SM, Han MH (2017) HCN Channel targets for novel antidepressant treatment. Neurotherapeutics 14:698–715. https://doi.org/10.1007/s13311-017-0538-7
Brennan GP, Baram TZ, Poolos NP (2016) Hyperpolarization-activated cyclic nucleotide-gated (HCN) channels in epilepsy. Cold Spring Harb Perspect Med 6:a022384. https://doi.org/10.1101/cshperspect.a022384
Shah MM (2014) Cortical HCN channels: function, trafficking and plasticity. J Physiol 592:2711–2719. https://doi.org/10.1113/jphysiol.2013.270058
Wang M, Ramos BP, Paspalas CD, Shu Y, Simen A, Duque A, Vijayraghavan S, Brennan A et al (2007) Alpha2A-adrenoceptors strengthen working memory networks by inhibiting cAMP-HCN channel signaling in prefrontal cortex. Cell 129:397–410. https://doi.org/10.1016/j.cell.2007.03.015
Shin KS, Rothberg BS, Yellen G (2001) Blocker state dependence and trapping in hyperpolarization-activated cation channels: evidence for an intracellular activation gate. J Gen Physiol 117:91–101. https://doi.org/10.1085/jgp.117.2.91
Zhang Z, Cordeiro Matos S, Jego S, Adamantidis A, Seguela P (2013) Norepinephrine drives persistent activity in prefrontal cortex via synergistic alpha1 and alpha2 adrenoceptors. PLoS One 8:e66122. https://doi.org/10.1371/journal.pone.0066122
Huang Z, Lujan R, Kadurin I, Uebele VN, Renger JJ, Dolphin AC, Shah MM (2011) Presynaptic HCN1 channels regulate Cav3.2 activity and neurotransmission at select cortical synapses. Nat Neurosci 14:478–486. https://doi.org/10.1038/nn.2757
Cai W, Liu SS, Li BM, Zhang XH (2022) Presynaptic HCN channels constrain GABAergic synaptic transmission in pyramidal cells of the medial prefrontal cortex. Biol Open 11:bio058840. https://doi.org/10.1242/bio.058840
Moosmang S, Biel M, Hofmann F, Ludwig A (1999) Differential distribution of four hyperpolarization-activated cation channels in mouse brain. Biol Chem 380:975–980. https://doi.org/10.1515/BC.1999.121
Zhang S, You Z, Wang S, Yang J, Yang L, Sun Y, Mi W, Yang L et al (2016) Neuropeptide S modulates the amygdaloidal HCN activities (Ih) in rats: implication in chronic pain. Neuropharmacology 105:420–433. https://doi.org/10.1016/j.neuropharm.2016.02.004
Ni L, Xu Y, Dong S, Kong Y, Wang H, Lu G, Wang Y, Li Q et al (2020) The potential role of the HCN1 ion channel and BDNF-mTOR signaling pathways and synaptic transmission in the alleviation of PTSD. Transl Psychiatry 10:101. https://doi.org/10.1038/s41398-020-0782-1
Inaba Y, Biagini G, Avoli M (2006) The H current blocker ZD7288 decreases epileptiform hyperexcitability in the rat neocortex by depressing synaptic transmission. Neuropharmacology 51:681–691. https://doi.org/10.1016/j.neuropharm.2006.05.017
Doan TN, Stephans K, Ramirez AN, Glazebrook PA, Andresen MC, Kunze DL (2004) Differential distribution and function of hyperpolarization-activated channels in sensory neurons and mechanosensitive fibers. J Neurosci 24:3335–3343. https://doi.org/10.1523/JNEUROSCI.5156-03.2004
Nolan MF, Malleret G, Lee KH, Gibbs E, Dudman JT, Santoro B, Yin D, Thompson RF et al (2003) The hyperpolarization-activated HCN1 channel is important for motor learning and neuronal integration by cerebellar Purkinje cells. Cell 115:551–564. https://doi.org/10.1016/s0092-8674(03)00884-5
Thompson JM, Neugebauer V (2019) Cortico-limbic pain mechanisms. Neurosci Lett 702:15–23. https://doi.org/10.1016/j.neulet.2018.11.037
Zhang Z, Gadotti VM, Chen L, Souza IA, Stemkowski PL, Zamponi GW (2015) Role of prelimbic GABAergic circuits in sensory and emotional aspects of neuropathic pain. Cell Rep 12:752–759. https://doi.org/10.1016/j.celrep.2015.07.001
Acknowledgements
We sincerely appreciate the electrophysiological platform provided by the South-Central University for Nationalities.
Funding
This study was supported by grants from the National Natural Science Foundation of China (grant number: 81974165).
Author information
Authors and Affiliations
Contributions
Designed experiments: Xixi Wang and Fang Luo; performed experiments: Xixi Wang and Sifei Gan; analyzed data: Xixi Wang and Sifei Gan; assisted in writing manuscript: Xixi Wang, Sifei Gan, Fang Luo, Zeru Zhang, Pengfei Zhu, and Chen Hong Li.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the ethical guidelines imposed by Laboratory Animal and Biomedical Ethics Committee of South-Central University for Nationalities (number: 2019-SCUEC-AEC-022).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Gan, S., Zhang, Z. et al. HCN-Channel-Dependent Hyperexcitability of the Layer V Pyramidal Neurons in IL-mPFC Contributes to Fentanyl-Induced Hyperalgesia in Male Rats. Mol Neurobiol 60, 2553–2571 (2023). https://doi.org/10.1007/s12035-023-03218-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03218-w