Abstract
The amyloid precursor protein (APP) is a transmembrane glycoprotein central to Alzheimer’s disease (AD) with functions in brain development and plasticity, including in neurogenesis and neurite outgrowth. Epidermal growth factor (EGF) and heparin-binding EGF-like growth factor (HB-EGF) are well-described neurotrophic and neuromodulator EGFR ligands, both implicated in neurological disorders, including AD. Pro-HB-EGF arose as a putative novel APP interactor in a human brain cDNA library yeast two-hybrid screen. Based on their structural and functional similarities, we first aimed to verify if APP could bind to (HB-)EGF proforms. Here, we show that APP interacts with these two EGFR ligands, and further characterized the effects of APP-EGF interaction in ERK activation and neuritogenesis. Yeast co-transformation and co-immunoprecipitation assays confirmed APP interaction with HB-EGF. Co-immunoprecipitation also revealed that APP binds to cellular pro-EGF. Overexpression of HB-EGF in HeLa cells, or exposure of SH-SY5Y cells to EGF, both resulted in increased APP protein levels. EGF and APP were observed to synergistically activate the ERK pathway, crucial for neuronal differentiation. Immunofluorescence analysis of cellular neuritogenesis in APP overexpression and EGF exposure conditions confirmed a synergistic effect in promoting the number and the mean length of neurite-like processes. Synergistic ERK activation and neuritogenic effects were completely blocked by the EGFR inhibitor PD 168393, implying APP/EGF-induced activation of EGFR as part of the mechanism. This work shows novel APP protein interactors and provides a major insight into the APP/EGF-driven mechanisms underlying neurite outgrowth and neuronal differentiation, with potential relevance for AD and for adult neuroregeneration.







Similar content being viewed by others
References
Coburger I, Hoefgen S, Than ME (2014) The structural biology of the amyloid precursor protein APP—a complex puzzle reveals its multi-domain architecture. Biol Chem 395:485–498. https://doi.org/10.1515/hsz-2013-0280
Nhan HS, Chiang K, Koo EH (2015) The multifaceted nature of amyloid precursor protein and its proteolytic fragments: friends and foes. Acta Neuropathol 129:1–19. https://doi.org/10.1007/s00401-014-1347-2
Lichtenthaler SF, Haass C, Steiner H (2011) Regulated intramembrane proteolysis—lessons from amyloid precursor protein processing. J Neurochem 117:779–796. https://doi.org/10.1111/j.1471-4159.2011.07248.x
Small SA, Gandy S (2006) Sorting through the cell biology of Alzheimer’s disease: intracellular pathways to pathogenesis. Neuron 52:15–31. https://doi.org/10.1016/j.neuron.2006.09.001
Westmark CJ (2013) What’s happening at synapses the role of amyloid β-protein precursor and β-Amyloid in neurological disorders. Mol Psychiatry 18:425–434. https://doi.org/10.1038/mp.2012.122
Müller UC, Zheng H (2012) Physiological functions of APP family proteins. Cold Spring Harb Perspect Med 2:a006288. https://doi.org/10.1101/cshperspect.a006288
Demars MP, Bartholomew A, Strakova Z, Lazarov O (2011) Soluble amyloid precursor protein: a novel proliferation factor of adult progenitor cells of ectodermal and mesodermal origin. Stem Cell Res Ther 2:36. https://doi.org/10.1186/scrt77
Young-Pearse TL, Bai J, Chang R, Zheng JB, LoTurco JJ, Selkoe DJ (2007) A critical function for β-amyloid precursor protein in neuronal migration revealed by in utero RNA interference. J Neurosci 27:14459–14469. https://doi.org/10.1523/JNEUROSCI.4701-07.2007
Hoe HS, Kea JL, Carney RSE et al (2009) Interaction of Reelin with amyloid precursor protein promotes neurite outgrowth. J Neurosci 29:7459–7473. https://doi.org/10.1523/JNEUROSCI.4872-08.2009
Sosa LJ, Bergman J, Estrada-Bernal A, Glorioso TJ, Kittelson JM, Pfenninger KH (2013) Amyloid precursor protein is an autonomous growth cone adhesion molecule engaged in contact guidance. PLoS One 8:e64521. https://doi.org/10.1371/journal.pone.0064521
Tyan SH, Shih AYJ, Walsh JJ, Maruyama H, Sarsoza F, Ku L, Eggert S, Hof PR et al (2012) Amyloid precursor protein (APP) regulates synaptic structure and function. Mol Cell Neurosci 51:43–52. https://doi.org/10.1016/j.mcn.2012.07.009
Weyer SW, Klevanski M, Delekate A, Voikar V, Aydin D, Hick M, Filippov M, Drost N et al (2011) APP and APLP2 are essential at PNS and CNS synapses for transmission, spatial learning and LTP. EMBO J 30:2266–2280. https://doi.org/10.1038/emboj.2011.119
Plummer S, Van den Heuvel C, Thornton E et al (2016) The neuroprotective properties of the amyloid precursor protein following traumatic brain injury. Aging Dis 7:163–179. https://doi.org/10.14336/AD.2015.0907
Mockett BG, Richter M, Abraham WC, Müller UC (2017) Therapeutic potential of secreted amyloid precursor protein APPsα. Front Mol Neurosci 10:30. https://doi.org/10.3389/fnmol.2017.00030
Carpenter G, Cohen S (1979) Epidermal growth factor. Annu Rev Biochem 48:193–216. https://doi.org/10.1146/annurev.bi.48.070179.001205
Zeng F, Harris RC (2014) Epidermal growth factor, from gene organization to bedside. Semin Cell Dev Biol 28:2–11. https://doi.org/10.1016/j.semcdb.2014.01.011
Raab G, Klagsbrun M (1997) Heparin-binding EGF-like growth factor. Biochim Biophys Acta - Rev Cancer 1333:F179–F199. https://doi.org/10.1016/S0304-419X(97)00024-3
Higashiyama S, Lau K, Besner GE et al (1992) Structure of heparin-binding EGF-like growth factor. Multiple forms, primary structure, and glycosylation of the mature protein. J Biol Chem 267:6205–6212. https://doi.org/10.1016/s0304-419x(97)00024-3
Massague J, Pandiella A (1993) Membrane-anchored growth factors. Annu Rev Biochem 62:515–541. https://doi.org/10.1146/annurev.bi.62.070193.002503
Harris RC, Chung E, Coffey RJ (2003) EGF receptor ligands. Exp Cell Res 284:2–13. https://doi.org/10.1016/S0014-4827(02)00105-2
Oda K, Matsuoka Y, Funahashi A, Kitano H (2005) A comprehensive pathway map of epidermal growth factor receptor signaling. Mol Syst Biol 1:2005.0010. https://doi.org/10.1038/msb4100014
Nelson AD, Suzuki M, Svendsen CN (2008) A high concentration of epidermal growth factor increases the growth and survival of neurogenic radial glial cells within human neurosphere cultures. Stem Cells 26:348–355. https://doi.org/10.1634/stemcells.2007-0299
Oyagi A, Hara H (2012) Essential roles of heparin-binding epidermal growth factor-like growth factor in the brain. CNS Neurosci Ther 18:803–810. https://doi.org/10.1111/j.1755-5949.2012.00371.x
Yamada M, Ikeuchi T, Hatanaka H (1997) The neurotrophic action and signalling of epidermal growth factor. Prog Neurobiol 51:19–37. https://doi.org/10.1016/S0301-0082(96)00046-9
Abe Y, Nawa H, Namba H (2009) Activation of epidermal growth factor receptor ErbB1 attenuates inhibitory synaptic development in mouse dentate gyrus. Neurosci Res 63:138–148. https://doi.org/10.1016/j.neures.2008.11.005
Wagner B, Natarajan A, Grünaug S, Kroismayr R, Wagner EF, Sibilia M (2006) Neuronal survival depends on EGFR signaling in cortical but not midbrain astrocytes. EMBO J 25:752–762. https://doi.org/10.1038/sj.emboj.7600988
Jin K, Mao XO, Sun Y, Xie L, Jin L, Nishi E, Klagsbrun M, Greenberg DA (2002) Heparin-binding epidermal growth factor-like growth factor: hypoxia-inducible expression in vitro and stimulation of neurogenesis in vitro and in vivo. J Neurosci 22:5365–5373. https://doi.org/10.1523/JNEUROSCI.22-13-05365.2002
Zhou Y, Besner GE (2011) Heparin-binding epidermal growth factor-like growth factor is a potent neurotrophic factor for PC12 cells. NeuroSignals 18:141–151. https://doi.org/10.1159/000319823
Chen-Plotkin AS, Hu WT, Siderowf A, Weintraub D, Goldmann Gross R, Hurtig HI, Xie SX, Arnold SE et al (2011) Plasma epidermal growth factor levels predict cognitive decline in Parkinson disease. Ann Neurol 69:655–663. https://doi.org/10.1002/ana.22271
Siddiqui S, Fang M, Ni B, Lu D, Martin B, Maudsley S (2012) Central role of the EGF receptor in neurometabolic aging. Int J Endocrinol 2012:739428–739414. https://doi.org/10.1155/2012/739428
Maurya SK, Mishra J, Abbas S, Bandyopadhyay S (2016) Cypermethrin stimulates GSK3β-dependent Aβ and p-tau proteins and cognitive loss in young rats: reduced HB-EGF signaling and downstream neuroinflammation as critical regulators. Mol Neurobiol 53:968–982. https://doi.org/10.1007/s12035-014-9061-6
Caillé I, Allinquant B, Dupont E et al (2004) Soluble form of amyloid precursor protein regulates proliferation of progenitors in the adult subventricular zone. Development 131:2173 LP–2172181. https://doi.org/10.1242/dev.01103
Refolo LM, Salton SRJ, Anderson JP, Mehta P, Robakis NK (1989) Nerve and epidermal growth factors induce the release of the Alzheimer amyloid precursor from PC 12 cell cultures. Biochem Biophys Res Commun 164:664–670. https://doi.org/10.1016/0006-291X(89)91511-8
Slack BE, Breu J, Muchnicki L, Wurtman RJ (1997) Rapid stimulation of amyloid precursor protein release by epidermal growth factor: role of protein kinase C. Biochem J 327:245–249. https://doi.org/10.1042/bj3270245
Zou L, Wang Z, Shen L, Bao GB, Wang T, Kang JH, Pei G (2007) Receptor tyrosine kinases positively regulate BACE activity and amyloid-β production through enhancing BACE internalization. Cell Res 17:389–401. https://doi.org/10.1038/cr.2007.5
Almeida CG, Takahashi RH, Gouras GK (2006) β-amyloid accumulation impairs multivesicular body sorting by inhibiting the ubiquitin-proteasome system. J Neurosci 26:4277–4288. https://doi.org/10.1523/JNEUROSCI.5078-05.2006
Zhang YW, Wang R, Liu Q, Zhang H, Liao FF, Xu H (2007) Presenilin/γ-secretase-dependent processing of β-amyloid precursor protein regulates EGF receptor expression. Proc Natl Acad Sci U S A 104:10613–10618. https://doi.org/10.1073/pnas.0703903104
Domingues SC, Henriques AG, Fardilha M, da Cruz e Silva EF, da Cruz e Silva OAB (2011) Identification and characterization of a neuronal enriched novel transcript encoding the previously described p60Fe65 isoform. J Neurochem 119:1086–1098. https://doi.org/10.1111/j.1471-4159.2011.07420.x
Domingues SC, Konietzko U, Henriques AG, Rebelo S, Fardilha M, Nishitani H, Nitsch RM, da Cruz e Silva EF et al (2014) RanBP9 modulates AICD localization and transcriptional activity via direct interaction with Tip60. J Alzheimers Dis 42:1415–1433. https://doi.org/10.3233/JAD-132495
Henriques AG, Vieira SI, Rebelo S, Domingues SCTS, da Cruz e Silva EF, da Cruz e Silva OAB (2007) Isoform specific amyloid-β protein precursor metabolism. J Alzheimers Dis 11:85–95. https://doi.org/10.3233/JAD-2007-11112
Martins F, Rebelo S, Santos M, Cotrim CZ, da Cruz e Silva EF, da Cruz e Silva OAB (2016) BRI2 and BRI3 are functionally distinct phosphoproteins. Cell Signal 28:130–144. https://doi.org/10.1016/j.cellsig.2015.10.012
Dittmer A, Dittmer J (2006) β-Actin is not a reliable loading control in Western blot analysis. Electrophoresis 27:2844–2845. https://doi.org/10.1002/elps.200500785
Da Rocha JF, Da Cruz e Silva OAB, Vieira SI (2015) Analysis of the amyloid precursor protein role in neuritogenesis reveals a biphasic SH-SY5Y neuronal cell differentiation model. J Neurochem 134:288–301. https://doi.org/10.1111/jnc.13133
Castano Z, Kypta RM (2008) Housekeeping proteins: limitations as references during neuronal differentiation. Open Neurosci J 2:36–40. https://doi.org/10.2174/1874082000802010036
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2-ΔΔCT method. Methods 25:402–408. https://doi.org/10.1006/meth.2001.1262
Zheng Y, Zhang C, Croucher DR, Soliman MA, St-Denis N, Pasculescu A, Taylor L, Tate SA et al (2013) Temporal regulation of EGF signalling networks by the scaffold protein Shc1. Nature 499:166–171. https://doi.org/10.1038/nature12308
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C et al (2012) Fiji: an open-source platform for biological-image analysis. Nat Methods 9:676–682. https://doi.org/10.1038/nmeth.2019
Vieira SI, Rebelo S, Domingues SC, da Cruz e Silva EF, da Cruz e Silva OAB (2009) S655 phosphorylation enhances APP secretory traffic. Mol Cell Biochem 328:145–154. https://doi.org/10.1007/s11010-009-0084-7
Vieira SI, Rebelo S, Esselmann H, Wiltfang J, Lah J, Lane R, Small SA, Gandy S et al (2010) Retrieval of the Alzheimer’s amyloid precursor protein from the endosome to the TGN is S655 phosphorylation state-dependent and retromer-mediated. Mol Neurodegener 5:40. https://doi.org/10.1186/1750-1326-5-40
Bolte S, Cordelières FP (2006) A guided tour into subcellular colocalization analysis in light microscopy. J Microsc 224:213–232. https://doi.org/10.1111/j.1365-2818.2006.01706.x
Manders EMM, Verbeek FJ, Aten JA (1993) Measurement of co-localization of objects in dual-colour confocal images. J Microsc 169:375–382. https://doi.org/10.1111/j.1365-2818.1993.tb03313.x
dos Domingues SCTS (2015) Identification of protein complexes in Alzheimer’s disease. https://ria.ua.pt/handle/10773/10851
Hieda M, Koizumi M, Higashi C, Tachibana T, Taguchi T, Higashiyama S (2012) The cytoplasmic tail of heparin-binding EGF-like growth factor regulates bidirectional intracellular trafficking between the plasma membrane and ER. FEBS Open Bio 2:339–344. https://doi.org/10.1016/j.fob.2012.09.002
Soba P, Eggert S, Wagner K, Zentgraf H, Siehl K, Kreger S, Löwer A, Langer A et al (2005) Homo- and heterodimerization of APP family members promotes intercellular adhesion. EMBO J 24:3624–3634. https://doi.org/10.1038/sj.emboj.7600824
Kohli BM, Pflieger D, Mueller LN, Carbonetti G, Aebersold R, Nitsch RM, Konietzko U (2012) Interactome of the amyloid precursor protein APP in brain reveals a protein network involved in synaptic vesicle turnover and a close association with synaptotagmin-1. J Proteome Res 11:4075–4090. https://doi.org/10.1021/pr300123g
Ono M, Raab G, Lau K et al (1994) Purification and characterization of transmembrane forms of heparin- binding EGF-like growth factor. J Biol Chem 269:31315–31321
Goishi K, Higashiyama S, Klagsbrun M, Nakano N, Umata T, Ishikawa M, Mekada E, Taniguchi N (1995) Phorbol ester induces the rapid processing of cell surface heparin-binding EGF-like growth factor: conversion from juxtacrine to paracrine growth factor activity. Mol Biol Cell 6:967–980. https://doi.org/10.1091/mbc.6.8.967
Gechtman Z, Alonso JL, Raab G et al (1999) The shedding of membrane-anchored heparin-binding epidermal-like growth factor is regulated by the Raf/mitogen-activated protein kinase cascade and by cell adhesion and spreading. J Biol Chem 274:28828–28835. https://doi.org/10.1074/jbc.274.40.28828
Evangelopoulos ME, Weis J, Krüttgen A (2005) Signalling pathways leading to neuroblastoma differentiation after serum withdrawal: HDL blocks neuroblastoma differentiation by inhibition of EGFR. Oncogene 24:3309–3318. https://doi.org/10.1038/sj.onc.1208494
Li Z, Theus MH, Wei L (2006) Role of ERK 1/2 signaling in neuronal differentiation of cultured embryonic stem cells. Develop Growth Differ 48:513–523. https://doi.org/10.1111/j.1440-169X.2006.00889.x
Evangelopoulos ME, Weis J, Krüttgen A (2009) Mevastatin-induced neurite outgrowth of neuroblastoma cells via activation of EGFR. J Neurosci Res 87:2138–2144. https://doi.org/10.1002/jnr.22025
Turner PR, O’Connor K, Tate WP, Abraham WC (2003) Roles of amyloid precursor protein and its fragments in regulating neural activity, plasticity and memory. Prog Neurobiol 70:1–32. https://doi.org/10.1016/S0301-0082(03)00089-3
Reinhard C, Hébert SS, De Strooper B (2005) The amyloid-β precursor protein: integrating structure with biological function. EMBO J 24:3996–4006. https://doi.org/10.1038/sj.emboj.7600860
Sosa LJ, Cáceres A, Dupraz S, Oksdath M, Quiroga S, Lorenzo A (2017) The physiological role of the amyloid precursor protein as an adhesion molecule in the developing nervous system. J Neurochem 143:11–29. https://doi.org/10.1111/jnc.14122
Small D, Nurcombe V, Reed G, Clarris H, Moir R, Beyreuther K, Masters CL (1994) A heparin-binding domain in the amyloid protein precursor of Alzheimer’s disease is involved in the regulation of neurite outgrowth. J Neurosci 14:2117–2127. https://doi.org/10.1523/JNEUROSCI.14-04-02117.1994
Nakamura K, Mitamura T, Takahashi T, Kobayashi T, Mekada E (2000) Importance of the major extracellular domain of CD9 and the epidermal growth factor (EGF)-like domain of heparin-binding EGF-like growth factor for up-regulation of binding and activity. J Biol Chem 275:18284–18290. https://doi.org/10.1074/jbc.M907971199
Martins SA, Correia PD, Dias RA, da Cruz e Silva OAB, Vieira SI (2019) CD81 promotes a migratory phenotype in neuronal-like cells. Microsc Microanal 25:229–235. https://doi.org/10.1017/S1431927618015532
Le Gall SM, Auger R, Dreux C, Mauduit P (2003) Regulated cell surface Pro-EGF ectodomain shedding is a zinc metalloprotease-dependent process. J Biol Chem 278:45255–45268. https://doi.org/10.1074/jbc.M307745200
Uhlen M, Fagerberg L, Hallstrom BM et al (2015) Tissue-based map of the human proteome. Science (80) 347:1260419. https://doi.org/10.1126/science.1260419
The Human Protein Atlas. https://www.proteinatlas.org/ENSG00000138798-EGF/cell
Teramoto T, Qiu J, Plumier J-C, Moskowitz MA (2003) EGF amplifies the replacement of parvalbumin-expressing striatal interneurons after ischemia. J Clin Invest 111:1125–1132. https://doi.org/10.1172/JCI17170
Wildering WC, Hermann PM, Bulloch AGM (2001) Lymnaea epidermal growth factor promotes axonal regeneration in CNS organ culture. J Neurosci 21:9345–9354. https://doi.org/10.1523/JNEUROSCI.21-23-09345.2001
Sun D, Bullock MR, Altememi N, Zhou Z, Hagood S, Rolfe A, McGinn MJ, Hamm R et al (2010) The effect of epidermal growth factor in the injured brain after trauma in rats. J Neurotrauma 27:923–938. https://doi.org/10.1089/neu.2009.1209
Thomas JT, Chhuy-Hy L, Andrykovich KR, Moos M Jr (2016) SMOC binds to pro-EGF, but does not induce Erk phosphorylation via the EGFR. PLoS One 11:e0154294. https://doi.org/10.1371/journal.pone.0154294
Kounnas MZ, Moir RD, Rebeck GW, Bush AI, Argraves WS, Tanzi RE, Hyman BT, Strickland DK (1995) LDL receptor-related protein, a multifunctional ApoE receptor, binds secreted beta-amyloid precursor protein and mediates its degradation. Cell 82:331–340. https://doi.org/10.1016/0092-8674(95)90320-8
Goto JJ, Tanzi RE (2002) The role of the low-density lipoprotein receptor-related protein (LRP1) in Alzheimer’s A beta generation: development of a cell-based model system. J Mol Neurosci 19:37–41. https://doi.org/10.1007/s12031-002-0008-4
Kitago Y, Nagae M, Nakata Z, Yagi-Utsumi M, Takagi-Niidome S, Mihara E, Nogi T, Kato K et al (2015) Structural basis for amyloidogenic peptide recognition by sorLA. Nat Struct Mol Biol 22:199–206. https://doi.org/10.1038/nsmb.2954
Andersen OM, Reiche J, Schmidt V, Gotthardt M, Spoelgen R, Behlke J, von Arnim CAF, Breiderhoff T et al (2005) Neuronal sorting protein-related receptor sorLA/LR11 regulates processing of the amyloid precursor protein. Proc Natl Acad Sci U S A 102:13461–13466. https://doi.org/10.1073/pnas.0503689102
Fassa A, Mehta P, Efthimiopoulos S (2005) Notch 1 interacts with the amyloid precursor protein in a Numb-independent manner. J Neurosci Res 82:214–224. https://doi.org/10.1002/jnr.20642
Oh SY, Chen C-D, Abraham CR (2010) Cell-type dependent modulation of Notch signaling by the amyloid precursor protein. J Neurochem 113:262–274. https://doi.org/10.1111/j.1471-4159.2010.06603.x
Cotman SL, Halfter W, Cole GJ (2000) Agrin binds to beta-amyloid (Abeta), accelerates abeta fibril formation, and is localized to Abeta deposits in Alzheimer’s disease brain. Mol Cell Neurosci 15:183–198. https://doi.org/10.1006/mcne.1999.0816
Salza R, Lethias C, Ricard-Blum S (2017) The multimerization state of the amyloid-β42 peptide (Aβ42) governs its interaction network with the extracellular matrix. J Alzheimers Dis 56:991–1005. https://doi.org/10.3233/JAD-160751
Ohsawa I, Takamura C, Kohsaka S (2001) Fibulin-1 binds the amino-terminal head of beta-amyloid precursor protein and modulates its physiological function. J Neurochem 76:1411–1420. https://doi.org/10.1046/j.1471-4159.2001.00144.x
Twal WO, Czirok A, Hegedus B et al (2001) Fibulin-1 suppression of fibronectin-regulated cell adhesion and motility. J Cell Sci 114:4587–4598
Daniels MP (2012) The role of agrin in synaptic development, plasticity and signaling in the central nervous system. Neurochem Int 61:848–853. https://doi.org/10.1016/j.neuint.2012.02.028
Choi HY, Liu Y, Tennert C, Sugiura Y, Karakatsani A, Kröger S, Johnson EB, Hammer RE et al (2013) APP interacts with LRP4 and agrin to coordinate the development of the neuromuscular junction in mice. Elife 2:e00220. https://doi.org/10.7554/eLife.00220
Handara G, Hetsch FJA, Jüttner R, Schick A, Haupt C, Rathjen FG, Kröger S (2019) The role of agrin, Lrp4 and MuSK during dendritic arborization and synaptogenesis in cultured embryonic CNS neurons. Dev Biol 445:54–67. https://doi.org/10.1016/j.ydbio.2018.10.017
Brooke JS, Cha J-H, Eidels L (2002) Latent transforming growth factor beta-binding protein-3 and fibulin-1C interact with the extracellular domain of the heparin-binding EGF-like growth factor precursor. BMC Cell Biol 3:2. https://doi.org/10.1186/1471-2121-3-2
Borel F, Marzocca F, Delcros J-G, Rama N, Mehlen P, Ferrer JL (2017) Molecular characterization of Netrin-1 and APP receptor binding: new leads to block the progression of senile plaques in Alzheimer’s disease. Biochem Biophys Res Commun 488:466–470. https://doi.org/10.1016/j.bbrc.2017.05.056
Mills J, Laurent Charest D, Lam F, Beyreuther K, Ida N, Pelech SL, Reiner PB (1997) Regulation of amyloid precursor protein catabolism involves the mitogen-activated protein kinase signal transduction pathway. J Neurosci 17:9415–9422. https://doi.org/10.1523/JNEUROSCI.17-24-09415.1997
da Cruz e Silva OAB, Rebelo S, Vieira SI et al (2009) Enhanced generation of Alzheimer’s amyloid-beta following chronic exposure to phorbol ester correlates with differential effects on alpha and epsilon isozymes of protein kinase C. J Neurochem 108:319–330. https://doi.org/10.1111/j.1471-4159.2008.05770.x
Kim S, Sato Y, Mohan PS, Peterhoff C, Pensalfini A, Rigoglioso A, Jiang Y, Nixon RA (2016) Evidence that the rab5 effector APPL1 mediates APP-βCTF-induced dysfunction of endosomes in Down syndrome and Alzheimer’s disease. Mol Psychiatry 21:707–716. https://doi.org/10.1038/mp.2015.97
Laifenfeld D, Patzek LJ, McPhie DL et al (2007) Rab5 mediates an amyloid precursor protein signaling pathway that leads to apoptosis. J Neurosci 27:7141–7153. https://doi.org/10.1523/JNEUROSCI.4599-06.2007
Edgar JR, Willén K, Gouras GK, Futter CE (2015) ESCRTs regulate amyloid precursor protein sorting in multivesicular bodies and intracellular amyloid-β accumulation. J Cell Sci 128:2520–2528. https://doi.org/10.1242/jcs.170233
da Motta LACR, Galli P, Piva F, Maggi R (1997) Effects of epidermal growth factor on the [3H]-thymidine uptake in the SK-N-SH and SH-SY5Y human neuroblastoma cell lines. Arq Neuropsiquiatr 55:444–451
Marshall CJ (1995) Specificity of receptor tyrosine kinase signaling: transient versus sustained extracellular signal-regulated kinase activation. Cell 80:179–185. https://doi.org/10.1016/0092-8674(95)90401-8
Santos SDM, Verveer PJ, Bastiaens PIH (2007) Growth factor-induced MAPK network topology shapes Erk response determining PC-12 cell fate. Nat Cell Biol 9:324–330. https://doi.org/10.1038/ncb1543
Young-Pearse TL, Chen AC, Chang R, Marquez C, Selkoe DJ (2008) Secreted APP regulates the function of full-length APP in neurite outgrowth through interaction with integrin beta1. Neural Dev 3:15. https://doi.org/10.1186/1749-8104-3-15
Tamayev R, Zhou D, D'Adamio L (2009) The interactome of the amyloid beta precursor protein family members is shaped by phosphorylation of their intracellular domains. Mol Neurodegener 4:28. https://doi.org/10.1186/1750-1326-4-28
Nizzari M, Venezia V, Repetto E, Caorsi V, Magrassi R, Gagliani MC, Carlo P, Florio T et al (2007) Amyloid precursor protein and Presenilin1 interact with the adaptor GRB2 and modulate ERK 1,2 signaling. J Biol Chem 282(18):13833–13844. https://doi.org/10.1074/jbc.M610146200
Chasseigneaux S, Dinc L, Rose C, Chabret C, Coulpier F, Topilko P, Mauger G, Allinquant B (2011) Secreted amyloid precursor protein β and secreted amyloid precursor protein α induce axon outgrowth in vitro through Egr1 signaling pathway. PLoS One 6(1):e16301. https://doi.org/10.1371/journal.pone.0016301
Gaviglio AL, Knelson EH, Blobe GC (2017) Heparin-binding epidermal growth factor-like growth factor promotes neuroblastoma differentiation. FASEB J 31:1903–1915. https://doi.org/10.1096/fj.201600828R
Funding
This work was supported by Fundação para a Ciência e a Tecnologia (FCT), Centro 2020 and Portugal 2020, the COMPETE program, QREN, and the European Union (FEDER program), via funding for the ongoing GoBack project (PTDC/CVT-CVT/32261/2017), the finished PTDC/SAU-NMC/111980/2009 project and JR SFRH/BD/78507/2011 PhD grant, and the support to the IBiMED Research Unit strategic program (UID/BIM/04501/2013; UID/BIM/04501/2019) and the LiM Facility via the Portuguese Platform of BioImaging (PPBI-POCI-01-0145-FEDER-022122). The authors also acknowledge the Swiss National Science Foundation (SNF 31003A_166177 grant). Microphotographs were acquired in the LiM facility of iBiMED/UA, a member of the Portuguese Platform of BioImaging (PPBI; POCI-01-0145-FEDER-022122).
Author information
Authors and Affiliations
Contributions
JR performed the EGF experiments, LB built the MycHB-EGF construct and performed the HB-EGF assays, SD performed the YTH screens and helped on the yeast co-transformation assays, and ARB performed the real-time PCR assays, under SIV supervision, with the help of OAB, and of UK (rodents’ brains IPs). JR, LB, ARB, and SIV analyzed and interpreted all data, and wrote the manuscript, which all authors have revised.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Consent for Publication
All authors have approved the final version of the manuscript and give their consent to be published.
Ethics Approval
The experiments including rodent brain lysates have followed the European legislation for animal experimentation, namely the 2010/63/EU and Council Directive 86/609/EEC. The experiments were approved and supervised by our Institutional Animal Care and Use Committee (IACUC): Comissão Responsável pela Experimentação e Bem-Estar Animal (CREBEA), and followed the 3R’s (Replacement, Reduction and Refinement) guidelines. The number of animals used and the suffering was minimized. The animals were housed under a controlled environment and their health status and well-being monitored daily. Under the EU guidelines, no specific ethics approval was required for this project since the rats were not manipulated and only euthanized by cervical stretching followed by decapitation, for brain removal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online resource 1.
Subcellular distribution and co-localization of exogenous Myc-HB-EGF with endogenous HB-EGF. HeLa cells transiently overexpressing the Myc-HB-EGF cDNA were immunolabeled with the anti-Myc tag antibody (green) and with the anti-HB-EGF antibody (red). Bar = 10 μm (PNG 2682 kb)
Online resource 2.
Effects of EGF treatment and APP overexpression on SH-SY5Y cell proliferation and survival. a SH-SY5Y cells were either transfected (‘Tf’) with the GFP empty vector (‘V’) or APP695-GFP (‘APP’) cDNAs, and stimulated or not for 3 min with 100 ng/mL human recombinant EGF (‘V+EGF’ and ‘APP+EGF’) immediately before cell media change. Fresh media included the Click-iT® EdU, a nucleotide analog incorporated in proliferating cells, and cells were fixed processed for analysis after 12h. b Representative epifluorescence microphotographs of cells tested with the Click-iT® EdU Alexa Fluor® imaging kit. Edu is labeled with a red fluorescing dye, and stains proliferating cells. Blue fluorescing Hoechst 33342 was used to assed the total number of cells. Bar = 50 μm. c Percentage of cell proliferation was calculated by counting the number of EdU red fluorescing cells versus the total number of Hoechst blue fluorescing cells (scored in 20 fields of view). d Plot of the total number of Hoechst positive cells per well in each experimental condition (scored in 20 fields of view). n = 3. Statistically non-significant results by the one-way ANOVA. Data is presented as mean ± standard error of the mean. (PNG 5360 kb)
Online resource 3.
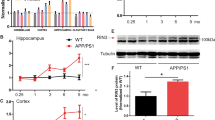
APP and EGF/EGFR interplay in SH-SY5Y neuronal-like differentiation. a APP and EGF combined treatment increases βIII-tubulin protein levels. SH-SY5Y cells, either transfected with the GFP empty vector (‘V’) or APP695-GFP (‘APP’) cDNAs, were stimulated or not for 3 min with 100 ng/mL of human recombinant EGF (‘V+EGF’ and ‘APP+EGF’) immediately before cell media change (16h before fixation/harvesting). When indicated, this EGF stimulation was performed under EGFR inhibition with 10 μM PD168393 (‘INIB’), added 1h before EGF. Cells were collected for analysis after 24h of cell transfection. Immunoblots of cell lysates were probed with the βIII-tubulin antibody, and βIII-tubulin protein levels were plotted as fold increases of the non-treated GFP-expressing cells (‘V’). n = 4-5. *p < 0.05, **p < 0.01 by one-way ANOVA followed by the Tukey’s multicomparison post-test. b EGFR inhibition reduces APP levels and APP-induced ERK activation, even in the absence of EGF. SH-SY5Y cells overexpressing APP-GFP were treated with 10 μM of the EGFR inhibitor PD168393 for 6 hours before transfection medium change, when the cells were incubated for more 16h with fresh culture medium. Immunoblots of cell lysates were probed with the APP C-terminal, phospho-ERK1/2 (‘pERK’), and total ERK 1/2 (‘tERK’) antibodies. Total APP full-length protein levels and the pERK/ERK ratio were plotted as fold increases of the respective non-treated APP-GFP control cells. n = 3. *p<0.05, **p<0.01 using the two-tailed unpaired t-test. Of note, in a and b, the lanes are from the same blots and were rearranged into the present order. Ponceau-S staining of total proteins bands was used as loading control for all the data, and data are presented as mean ± standard error of the mean (PNG 4166 kb)
Rights and permissions
About this article
Cite this article
da Rocha, J.F., Bastos, L., Domingues, S.C. et al. APP Binds to the EGFR Ligands HB-EGF and EGF, Acting Synergistically with EGF to Promote ERK Signaling and Neuritogenesis. Mol Neurobiol 58, 668–688 (2021). https://doi.org/10.1007/s12035-020-02139-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-020-02139-2