Abstract
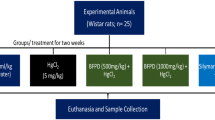
This investigation examines the possibility that exposure to silica dust of hypertensive individuals may exacerbate brain pathology and sensory motor dysfunction at high environmental temperature. Hypertension was produced in rats (200–250 g) by two-kidney one clip (2K1C) method, and in these animals, SiO2 nanoparticles (NPs; 50 to 60 nm) were administered at 50 mg/kg, i.p. daily for 1 week. On the 8th day, these rats were subjected to partial restraint in a Perspex box for 4 h either at room temperature (21 °C) or at 33 °C in a biological oxygen demand incubator (wind velocity, 2.6 cm/s; relative humidity, 65 to 67 %). In these animals, behavioral functions, blood–brain barrier (BBB) permeability to Evans blue albumin (EBA) and radioiodine ([131]-Iodine), brain water content and neuronal injuries were determined. Hypertensive rats subjected to 4 h restraint at room temperature did not exhibit BBB dysfunction, brain edema, neural injury, or alterations in rotarod or inclined plane angle performances. However, when these hypertensive rats were subjected to restraint at 33 °C, breakdown of the cortical BBB (EBA, +38 %; radioiodine, +56 %), brain water (+0.88 %), neuronal damages (+18 %), and behavioral impairment were exacerbated. Interestingly, SiO2 exposure to these rats further exacerbated BBB breakdown (EBA, 280 %; radioiodine, 350 %), brain edema (4 %), and neural injury (30 %) after identical restraint depending on the ambient temperature. SiO2 treatment also induced brain pathology and alteration in behavioral functions in normotensive rats after restraint at high temperature. These observations clearly show that hypertension significantly enhances restraint-induced brain pathology, and behavioral anomalies particularly at high ambient temperature and SiO2 intoxication further exacerbated these brain pathologies and cognitive dysfunctions.








Similar content being viewed by others
References
Sharma HS, Westman J (2004) Blood-spinal cord and brain barriers in health and disease. Academic, New York, pp 1–617
Sharma HS (2009) Blood–central nervous system barriers: the gateway to neurodegeneration, neuroprotection and neuroregeneration. In: Lajtha A, Banik N, Ray SK (eds) Handbook of neurochemistry and molecular neurobiology: brain and spinal cord trauma. Springer, Berlin, pp 363–457
Sharma HS, Sharma A (2010) Breakdown of the blood–brain barrier in stress alters cognitive dysfunction and induces brain pathology. New perspective for neuroprotective strategies. In: Ritsner M (ed) Brain protection in schizophrenia, mood and cognitive disorders. Springer, Berlin, pp 243–304
Sharma HS (2009) Nanoneuroscience and nanoneuropharmacology. Prog Brain Res 180:1–286
Sharma HS, Sharma A (2007) Nanoparticles aggravate heat stress induced cognitive deficits, blood–brain barrier disruption, edema formation and brain pathology. Prog Brain Res 162:245–273
Sharma HS, Sharma A (2012) Nanowired drug delivery for neuroprotection in central nervous system injuries: modulation by environmental temperature, intoxication of nanoparticles, and comorbidity factors. Wiley Interdiscip Rev Nanomed Nanobiotechnol 4:184–203
Sharma HS (2006) Hyperthermia influences excitatory and inhibitory amino acid neurotransmitters in the central nervous system. An experimental study in the rat using behavioural, biochemical, pharmacological, and morphological approaches. J Neural Transm 113:497–519
Sharma HS, Dey PK (1986) Influence of long-term immobilization stress on regional blood–brain barrier permeability, cerebral blood flow and 5-HT level in conscious normotensive young rats. J Neurol Sci 72:61–76
Sharma HS, Dey PK (1988) EEG changes following increased blood–brain barrier permeability under long-term immobilization stress in young rats. Neurosci Res 5:224–239
Sharma HS, Dey PK (1987) Influence of long-term acute heat exposure on regional blood–brain barrier permeability, cerebral blood flow and 5-HT level in conscious normotensive young rats. Brain Res 424:153–162
Sharma HS, Sharma A (2012) Neurotoxicity of engineered nanoparticles from metals. CNS Neurol Disord Drug Targets 11:65–80
Muresanu DF, Sharma HS (2007) Chronic hypertension aggravates heat stress induced cognitive dysfunction and brain pathology: an experimental study in the rat, using growth hormone therapy for possible neuroprotection. Ann N Y Acad Sci 1122:1–22
Muresanu DF, Zimmermann-Meinzingen S, Sharma HS (2010) Chronic hypertension aggravates heat stress-induced brain damage: possible neuroprotection by cerebrolysin. Acta Neurochir Suppl 106:327–333
Granado NS, Smith TC, Swanson GM, Harris RB, Shahar E, Smith B, Boyko EJ, Wells TS, Ryan MA, Millennium Cohort Study Team (2009) Newly reported hypertension after military combat deployment in a large population-based study. Hypertension 54:966–973
Wenzel D, Souza JM, Souza SB (2009) Prevalence of arterial hypertension in young military personnel and associated factors. Rev Saude Publica 43:789–795
Muresanu DF, Sharma A, Tian ZR, Smith MA, Sharma HS (2012) Nanowired drug delivery of antioxidant compound H-290/51 enhances neuroprotection in hyperthermia-induced neurotoxicity. CNS Neurol Disord Drug Targets 11:50–64
Sharma HS, Ali SF, Tian ZR, Hussain SM, Schlager JJ, Sjöquist PO, Sharma A, Muresanu DF (2009) Chronic treatment with nanoparticles exacerbate hyperthermia induced blood–brain barrier breakdown, cognitive dysfunction and brain pathology in the rat. Neuroprotective effects of nanowired-antioxidant compound H-290/51. J Nanosci Nanotechnol 9:5073–5090
Brimfield AA (2012) Chemicals of military deployments: revisiting Gulf War Syndrome in light of new information. Prog Mol Biol Transl Sci 112:209–230
Sharma HS, Patnaik R, Sharma A, Sjöquist PO, Lafuente JV (2009) Silicon dioxide nanoparticles (SiO2, 40–50 nm) exacerbate pathophysiology of traumatic spinal cord injury and deteriorate functional outcome in the rat. An experimental study using pharmacological and morphological approaches. J Nanosci Nanotechnol 9:4970–4980
Black DW, Carney CP, Peloso PM, Woolson FR, Schwartz DA, Voelker MD, Barrett DH, Doebbeling BN (2004) Gulf War veterans with anxiety: prevalence, comorbidity, and risk factors. Epidemiology 15:135–142
Bleich A, Solomon Z (2004) Evaluation of psychiatric disability in PTSD of military origin. Isr J Psychiatry Relat Sci 41:268–276
Sokrab TE, Johansson BB, Kalimo H, Olsson Y (1988) A transient hypertensive opening of the blood–brain barrier can lead to brain damage. Extravasation of serum proteins and cellular changes in rats subjected to aortic compression. Acta Neuropathol 75:557–565
Fredriksson K, Kalimo H, Westergren I, Kåhrström J, Johansson BB (1987) Blood–brain barrier leakage and brain edema in stroke-prone spontaneously hypertensive rats. Effect of chronic sympathectomy and low protein/high salt diet. Acta Neuropathol 74:259–268
Johansson BB (1984) Cerebral vascular bed in hypertension and consequences for the brain. Hypertension 6(6 Pt 2):III81–III86
Dey PK, Sharma HS, Rao KS (1980) Effect of indomethacin (a prostaglandin synthetase inhibitor) on the permeability of blood–brain and blood-CSF barriers in rat. Indian J Physiol Pharmacol 24:25–36
Kalimo H, Fredriksson K, Nordborg C, Auer RN, Olsson Y, Johansson B (1986) The spread of brain oedema in hypertensive brain injury. Med Biol 64:133–137
Sharma HS, Westman J, Nyberg F (1998) Pathophysiology of brain edema and cell changes following hyperthermic brain injury. Prog Brain Res 115:351–412
Sharma HS, Hoopes PJ (2003) Hyperthermia induced pathophysiology of the central nervous system. Int J Hyperthermia 19:325–354
Overstreet DH, Wegener G (2013) The flinders sensitive line rat model of depression—25 years and still producing. Pharmacol Rev 65:143–155
Sharma HS, Cervós-Navarro J, Dey PK (1991) Increased blood–brain barrier permeability following acute short-term swimming exercise in conscious normotensive young rats. Neurosci Res 10:211–221
Sharma HS, Westman J, Navarro JC, Dey PK, Nyberg F (1995) Probable involvement of serotonin in the increased permeability of the blood–brain barrier by forced swimming. An experimental study using Evans blue and 131I-sodium tracers in the rat. Behav Brain Res 72:189–196
Lafuente JV, Sharma A, Patnaik R, Muresanu DF, Sharma HS (2012) Diabetes exacerbates nanoparticles induced brain pathology. CNS Neurol Disord Drug Targets 11:26–39
Acknowledgments
This investigation is partially supported by the Air Force Office of Scientific Research (London), Air Force Material Command, USAF, under grant number FA8655-05-1-3065. The US Government is authorized to reproduce and distribute reprints for Government purpose notwithstanding any copyright notation thereon. The views and conclusions contained herein are those of the authors and should not be interpreted as necessarily representing the official policies or endorsements, either expressed or implied, of the Air Force Office of Scientific Research or the US Government. Financial support of Swedish Medical Research Council (Grant No. 2710, HSS); Astra-Zeneca, Mölndal, Sweden (HSS), Alexander von Humboldt Foundation, Germany (HSS); India-EU Research Co-operation (AS/RP), Ministry of Science and Technology, Government of India, New Delhi, India (AS/RP) and University Grants Commission, New Delhi, India (HSS); Indian Council of Medical Research, New Delhi, India (HSS) is gratefully acknowledged. The authors have no conflict of interest with any agencies mentioned above.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, H.S., Muresanu, D.F., Patnaik, R. et al. Exacerbation of Brain Pathology After Partial Restraint in Hypertensive Rats Following SiO2 Nanoparticles Exposure at High Ambient Temperature. Mol Neurobiol 48, 368–379 (2013). https://doi.org/10.1007/s12035-013-8502-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-013-8502-y