Abstract
Although patients with early localized prostate cancer can survive longer, castration-resistant prostate cancer (CRPC) has gradually emerged with the use of androgen deprivation therapy (ADT). N-Myc and TEM8 play a vital role in the progression of several cancer types. However, the underlying mechanism of how N-Myc and TEM8 promote the progression of prostate cancer remains unclear. In this study, the expression of N-Myc and TEM8 was detected in benign prostatic hyperplasia (BPH) and prostate cancer (PCa) tissues by immunohistochemistry (IHC). LNCaP cell lines were maintained in RPMI 1640 medium supplemented with 10% charcoal-stripped fetal bovine serum. Subsequently, R language software was used to verify our results. Tubule formation assay of human umbilical vein endothelial cell (HUVEC) was conducted to examine the effect of N-Myc and TEM8 overexpression on angiogenesis in prostate cancer cells. IHC results showed a positive correlation between the expression of N-Myc and TEM8 in prostate cancer tissues. Further analysis showed that N-Myc and TEM8 were associated with clinicopathological features and poor prognosis in prostate cancer patients. Moreover, the overexpression of N-Myc and TEM8 promoted proliferation of prostate cancer cells and angiogenesis. Additionally, N-Myc and TEM8 overexpression was associated with therapeutic resistance. We further found that N-Myc promoted angiogenesis and therapeutic resistance in prostate cancer via TEM8. Hence, targeting N-Myc/TEM8 pathway in prostate cancer would be a novel therapeutic strategy to enhance the treatment of prostate cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most diagnosed malignancy in men and the second leading cause of cancer-related deaths in the USA. Although the recent improvement in treatment options has significantly reduced the incidence rate, there has been a steady increase in advanced or metastasized prostate cancers [1]. Generally, the symptoms of prostate cancer in the early stage are not evident in most cases, which makes treatment more difficult [2]. Prostate cancer progression follows a multistep process that includes prostate intraepithelial neoplasia (PIN), local prostate cancer, advanced prostate adenocarcinoma with local invasion, and metastatic prostate cancer [3]. Recently, the advent usage of androgen deprivation therapy (ADT) has brought some symptomatic relief to prostate cancer patients. However, this also leads to the development of castration-resistant prostate cancer. Therefore, a deeper understanding of the mechanism of the disease process is relevant in our quest to find a novel and specific biomarker for prostate cancer treatment.
N-Myc, a member of the MYC proto-oncogene family, is known to play several oncogenic activities. Mounting studies have indicated that N-Myc is involved in all facets of prostate cancer progression [4,5,6], including the transformation of castration-resistant prostate cancer to neuroendocrine [7, 8]. Previous study has shown that TEM8 is upregulated in LNCaP and 22RV1 prostate cancer cell lines, particularly after the overexpression of N-Myc [7]. However, the detailed mechanism of how N-Myc interacts with TEM8 to promote prostate cancer progression remains unknown. TEM8, also known as ANTXR1, is a cell-surface transmembrane protein initially identified in the vascular endothelial cells of colon cancer [9]. Some studies have shown that the vascular density in high-grade prostate cancer is significantly higher than that in low-grade prostate cancer tumors [10], which implicates angiogenesis as a mechanism of prostate cancer progression. Even though TEM8 is associated with poor prognosis in several solid tumors [11,12,13,14], little is known about its role in prostate cancer progression. Therefore, this study was designed to elucidate how N-Myc interacts with TEM8 to promote angiogenesis and treatment resistance in prostate cancer.
Materials and methods
Patients and specimens
Formalin-fixed paraffin-embedded tissues were collected from 151 patients who underwent surgical operation at the First Affiliated Hospital of Anhui Medical University. The protocols used in the study were approved by the ethical committee of Anhui medical university.
RT-qPCR assays
Total RNA was isolated from cultured cells using Trizol reagent (Invitrogen). RNA was reversely transcribed into cDNA using the PrimeScript RT Master Mix (Takara, RR036A). Gene-specific primers are as follows:
GAPDH: Forward, 5′-CATGAGAAGTATGACAACAGCCT-3′,
Reverse, 5′-AGTCCTTCCACGATACCAAAGT-3′;
N-Myc: Forward, 5′-CACGTCCGCTCAAGAGTGTC-3′,
Reverse, 5′-GTTTCTGCGACGCTCACTGT-3′;
TEM8: Forward 5′-GATGATGATGGTCTGCCTAAGA-3′,
Reverse 5′-TCTTTGCCTTTTCCAACTTAGC-3′.
Cell culture and construction
The cell lines were maintained in RPMI 1640 medium (HyClone, SH30809.01) supplemented with 10% FBS (BI, 04-001-01A) or 10% charcoal-stripped fetal bovine serum (MRC, CCS30010.01HT,), 1.5 mM L-Glutamine, and 1% penicillin–streptomycin solution. Lentiviral vector for N-Myc and TEM8 was purchased from Genepharma (Shanghai, China) and stably transfected into LNCap and C4-2 cell lines. Finally, stable prostate cancer cells were successfully screened with the appropriate concentration of puromycin. The specific concentration of puromycin used in screening LNCaP stable cell lines is 2.00ug/ml, and the concentration of puromycin used to screen C4-2 is 1.00ug/ml. The efficiency of overexpression was analyzed by quantitative real-time PCR (qPCR) and western blot. Also, cell lines with N-Myc overexpression were transfected with shRNA-TEM8. The sequences of shRNA-TEM8 were designed as follows: GCTGAACCATCCACCATATGT. A non-targeting shRNA (Genepharma) was used as a control.
Western blotting
Proteins were extracted from prostate cancer cells using RIPA buffer. Proteins were loaded onto 10% SDS-PAGE gels and then transferred to NC membranes. Nonspecific binding was blocked with 5% dried skim milk. The membranes were incubated overnight at 4 ℃ with the following primary antibodies: anti-GAPDH (dilution 1:1000, ProteinTech, 10,494-1-AP), anti-N-Myc (dilution 1:1000, CST, #51705 s), anti-TEM8 (dilution 1:400, Abcam, #13,798), and anti-AR (dilution 1:2000, CST, 5153 s). After incubation with a peroxidase-conjugated secondary antibody, the protein bands were observed with ECL. The intensity of the protein bands was normalized with GAPDH.
Immunohistochemical analysis
Formalin-fixed paraffin-embedded samples were obtained from benign prostatic hyperplasia and prostate cancer patients. Briefly, sections were deparaffinized with xylene and rehydrated with graded ethanol. Heat-induced antigen retrieval was performed according to the relevant antibody instructions and endogenous peroxidase activities were blocked with hydrogen peroxide for 10 min at room temperature. The sections were incubated with the following antibodies: anti-N-Myc antibody (dilution 1:640, CST, #51705 s), anti-TEM8 antibody (dilution 1:20, NOVUS, 200C1339). The scoring of N-Myc and TEM8 was performed as previously described [15].
Cell counting Kit-8
100ul of cell suspension with a concentration of 3 × 104 /ml was added to each well (96-well plate) and cultured for 1 day, 2 days, and 3 days. After incubation with 10 ul of cck8 solution for 4 h, the absorbance was measured at 450 nm. The fold change of cell viability was equal to 100% × (As–Ab)/(Ac−Ab): As = OD450nm of the experimental group; Ab = OD450nm of the blank control; Ac = OD450nm of the control.
Tubule formation assay
Matrigel (# 356,234, Corning) was added into precooled 96-well plates (60μL/well) and incubated at 37 °C for 30 min. 3 × 104 HUVEC cells were inoculated into each well, and the corresponding concentrated supernatant was added and placed into the incubator for further incubation. The tube formation was observed under an inverted microscope at different time points. ImageJ was used to measure the length of the tube.
Oncomine and GEO datasets analysis
Oncomine microarray database (https://www.oncomine.org) was used to validate the prognostic value of N-Myc and TEM8 in prostate cancer patients. In this study, the threshold was defined as p-value = 0.0001. The overall survival and expression levels of N-Myc and TEM8 were plotted using GraphPad Prism software.
In GSE150368 datasets, the LIMMA package and Edger package of R software was used to detect and screen differentially expressed genes (DEGs) in prostate tissue before and after ADT treatment. DEGs analysis was performed based on the screening criteria of FDR > 0.05 and |log (FC)|> 1. KEGG enrichment analysis was used to detect the relationship between the function and signaling pathway of DEGs. Furthermore, the String Online database (confidence score of ≥ 0.15) was used to identify the protein–protein interaction (PPI) network (https://string-db.org/).
Statistical methods
All the experiments had three independent replicates, and the data were presented as mean ± SD. Statistical analyses were performed using Pearson chi-square test or Log-rank test unless otherwise indicated. A p-value of < 0.05 was considered statistically significant.
Results
N-Myc and TEM8 expression were associated with clinicopathological features of PCa and there was a positive correlation between them
IHC results showed that the positive rate of N-Myc and TEM8 was significantly higher in PCa than in BPH samples (Fig. 1A–D; Table 1). High expressions N-Myc and TEM8 were associated with a high Gleason score, advanced TNM stage, and osseous metastasis. However, TEM8 but not N-Myc was associated with elevated PSA levels (Table 2).
Expression of N-Myc and TEM8 in prostate tissues and their correlation with prognosis. A N-Myc was negatively expressed in BPH. B N-Myc was positively expressed in PCa (left), and N-Myc was expressed in the nucleus and cytoplasm of PCa cells (right). C TEM8 was negatively expressed in BPH. D TEM8 was positively expressed in PCa (left), and TEM8 was expressed in the membrane and/or cytoplasm of PCa cells (right). (The magnification of Fig. 1. A–D is 100X on the left and 400X on the right). (E, F) N-Myc and TEM8 were related to the overall survival rate of PCa as shown by Taylor Prostate dataset in the Oncomine database
We observed that N-Myc was positively correlated to the expression of TEM8 in PCa (R = 0.244, P = 0.02) (Table 3). According to the oncomine database, patients with high expression of N-Myc or TEM8 had a significantly lower overall survival rate than those with low N-Myc or TEM8 expression (Fig. 1E, F). Taken together, N-Myc and TEM8 expressions are closely related to the clinical progression and prognosis of prostate cancer.
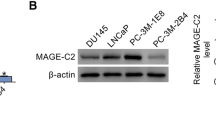
N-Myc overexpression upregulated TEM8 expression in PCa cells
This study found that high expression of N-Myc and TEM8 was associated with high degree of prostate cancer (P < 0.05) (Fig. 2A), suggesting that N-Myc and TEM8 are involved in the progression of prostate cancer. To further study the relationship between N-Myc and TEM8 in prostate cancer progression, stable cell lines with N-Myc and TEM8 overexpression were generated by lentivirus infection. The results were observed by fluorescence microscopy (Fig. 2B). Subsequently, the overexpression of N-Myc and TEM8 was verified in LNCaP and C4-2 cell lines by western blot and PCR (Fig. 2C).
Overexpression of N-Myc and TEM8 using lentivirus in prostate cancer cell lines. A The mRNA expression level of N-Myc and TEM8 in LNCaP, C4-2, and PC3 cell lines. B N-Myc and TEM8 overexpressing stable cell lines for LNCaP and C4-2 by lentivirus infection as observed under fluorescence microscope (× 100). C Expression of N-Myc and TEM8 were detected in lentivirus-transfected prostate cell lines at mRNA and protein levels. D Expression of TEM8 was detected in N-Myc overexpressing stable cell lines (*P < 0.05, **P < 0.005, ***P < 0.001)
To validate the results obtained from clinical samples, the mRNA and protein expressions of TEM8 were detected in N-Myc overexpressing stable cell lines. Our study further confirmed that N-Myc regulated the expression of TEM8 in prostate cancer cells (Fig. 2D).
Overexpression of N-Myc and TEM8 promoted the proliferation and tubule formation in prostate cancer cells
In N-Myc overexpressing stable cells (LNCaP and C4-2), the expression of TEM8 was verified after TEM8 shRNA knockdown (Fig. 3A). Compared with LNCaP/Vector, the growth rate of cancer cells was significantly higher in LNCaP/N-Myc and LNCaP/TEM8 groups (P < 0.05). However, the proliferation of cancer cells was lower in LNCaP/N-Myc/shTEM8 than LNCaP/N-Myc. A similar trend was observed in the C4-2 group (Fig. 3B). Next, we found from tube formation experiments that overexpression of N-Myc and TEM8 significantly promoted angiogenesis in prostate cancer (Fig. 3C).
Effects of N-Myc and TEM8 on the proliferative ability and tubule formation of PCa cells. A The mRNA and protein expressions of TEM8 were verified after LNCaP/N-Myc and C4-2/N-Myc cells were treated with TEM8-shRNA. B Compared with the control group, the overexpression of N-Myc and TEM8 affected the proliferative ability of LNCaP and C4-2 cells. C HUVEC tube formation assay was determined using the supernatant from LNCaP cells
N-Myc overexpression confers LNCaP cells resistant to ADT treatment
CCK8 experiment demonstrated that LNCaP/N-Myc and LNCaP/TEM8 cells could promote the proliferation of prostate cancer cells after ADT treatment. This suggests that N-Myc and TEM8 are likely to have ADT resistance (Fig. 4A). With the extension of ADT treatment time, the expression of AR protein in LNCaP/Vector cells was decreased. However, the opposite trend was observed in LNCaP/N-Myc cells. Although the expression of AR did not increase significantly in LNCaP/TEM8 cells, the expression of TEM8 was significantly increased (Fig. 4B).
Effects of ADT treatment on proliferation and protein expression in stable cell lines. A After 0, 1, 4, and 7 days of ADT treatment, the proliferation rates of LNCaP/N-Myc and LNCaP/TEM8 cells were higher than the control group (*P < 0.05, **P < 0.005, ***P < 0.001). B ADT treatment in LNCaP/Vector, LNCaP/N-Myc, and LNCaP/TEM8 cells could not inhibit the expression of N-Myc and TEM8. C KEGG pathway enrichment analysis of the differentially expressed genes after ADT treatment. D The Hub genes were identified. E A heatmap of ADT-treated differentially expressed genes in the GEO dataset was plotted. F Protein–protein interaction (PPI) network related to TEM8 was constructed using the STRING online database
To further confirm our experimental results, we used bioinformatics to analyze differentially expressed genes in PCa before and after ADT. 1693 differentially expressed genes were obtained, including 1227 upregulated and 466 down-regulated genes (Supplementary Table S1). KEGG analysis showed that differential genes were associated with pathways such as cytokine-cytokine receptor interaction, Staphylococcus aureus infection, Human T-cell leukemia virus 1 infection, cell adhesion molecules, and chemokine signaling pathway (Fig. 4C). The network core genes were obtained according to the number of adjacent gene nodes. As shown in (Fig. 4D, Supplementary Table S2), 75 adjacent gene nodes were identified for TEM8. The upregulated and down-regulated differential genes were summarized in Fig. 4E. Using the SRTING online database, protein network interacting with TEM8 was constructed (Fig. 4F).
Discussion
N-Myc, a critical oncoprotein required for neuroendocrine tumor development, is overexpressed and amplified in approximately 5% of PCA and 40% of NEPC [16, 17]. During prostate cancer progression, N-Myc overexpression can potentiate the escape of tumors from AR and promote the development of CRPC and NEPC [8]. Dardenne et al. found that N-Myc can cooperate with EZH2 to establish a new signaling pathway that can drive the differentiation of prostate cancer to neuroendocrine [7]. Emerging evidence shows that N-Myc amplification is associated with high vascular density in neuroblastoma [18]. However, the detailed underlying mechanism of action of N-Myc in PCa is not fully understood.
TEM8, an integrin-like cell-surface transmembrane protein, is highly upregulated in the tumor endothelium and expressed in several cancer types [19]. Antibodies against TEM8 have shown a broad range of anti-tumor activity due to their ability to target TEM8 and selectively inhibit pathological angiogenesis without causing severe side effects [20]. In breast cancer, specific antibodies against TEM8 can target cancer stem cells and tumor-associated vascular systems to inhibit tumor progression [21]. Although these suggest that TEM8 can be a therapeutic target, such evidence remains unknown in prostate cancer.
We found that the expression of N-Myc and TEM8 in clinical samples correlated with prostate cancer tissue type, tumor progression, and patient’s prognosis. The positive rates of N-Myc and TEM8 were significantly associated with a high Gleason score (Gleason score above 7) and TNM stage (III/IV). Additionally, N-Myc and TEM8 were significantly higher in patients with bone metastasis than those without bone metastasis. Furthermore, expressions of N-Myc and TEM8 were associated with poor prognosis in prostate cancer patients. These results suggest that N-Myc is a predictor of advanced stage of prostate cancer and plays a crucial role in prostate cancer progression.
Moreover, we demonstrated a significant positive correlation between N-Myc and TEM8 expression in PCa samples. Further experiments revealed that overexpression of N-Myc upregulated the expression of TEM8 in prostate cancer cells. This finding is consistent with previous report by Dardenne et al. [7]. Furthermore, our results showed that N-Myc promoted the proliferation rate of prostate cancer cells by regulating TEM8. However, the regulatory action of N-Myc on TEM8 in prostate cancer still requires further exploration.
It has been demonstrated that the incidence of lethal PCa might increase following the increased usage of androgen deprivation therapy, which has brought difficulty in treating patients with advanced prostate cancer. Our tubule formation assays confirmed that N-Myc and TEM8 may promote angiogenesis in prostate cancer cells. Furthermore, we found that overexpression of N-Myc and TEM8 significantly increased the proliferation of PCa cells after ADT treatment. However, compared with the control group, the expression level of AR protein in N-Myc overexpression group was not inhibited but showed a gradual increase. Consistent with our findings, previous studies have demonstrated that N-Myc has an inhibitory action on the expression of AR in PCa cells, thus rendering ADT ineffective. We showed that N-Myc upregulation after ADT treatment was associated with an increase in the expression of TEM8. Interestingly, AR protein levels in cell lines overexpressing TEM8 did not change significantly after ADT treatment, suggesting that TEM8 can potentiate the escape of prostate cancers from castration. This is suggestive that N-Myc can potentiate the escape of prostate cancer cells from ADT therapy by upregulating the expression of TEM8.
Changes in protein levels after ADT and tubule formation assays in our study showed that N-Myc might increase therapeutic resistance and angiogenesis in prostate cancer by regulating TEM8.
Conclusion
Our study has revealed that N-Myc and TEM8 can promote angiogenesis and therapeutic resistance in prostate cancer (Fig. 5). This study also showed for the first time that N-Myc could regulate the expression of TEM8 in prostate cancer. We also demonstrate that TEM8 is associated with markers of prostate cancer progression. Hence, our finding supports the notion that TEM8 can be used as a marker to indicate treatment response in patients with advanced prostate cancer.
Proposed mechanism of how N-Myc and TEM8 promote angiogenesis and therapeutic resistance of prostate cancer. N-Myc can regulate the expression of TEM8 in prostate cancer tissues. In prostate cancer cells, both N-Myc and TEM8 can induce AR which makes prostate cancer cells resistant to ADT therapy. Further, both N-Myc and TEM8 can promote angiogenesis and the proliferation of prostate cancer cells
Data availability
The datasets used in this study are available from the first author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- CRPC:
-
Castration resistance prostate cancer
- ADT:
-
Androgen deprivation therapy
- BPH:
-
Benign prostatic hyperplasia
- PCa:
-
Prostate cancer
- IHC:
-
Immunohistochemistry
- HUVEC:
-
Human umbilical vein endothelial cell
- PIN:
-
Prostate intraepithelial neoplasia
- shRNA:
-
Short hairpin RNA
- AR:
-
Androgen receptor
- DEGs:
-
Differentially expressed genes
- PPI:
-
Protein–protein interaction
- NEPC:
-
Neuroendocrine prostate cancer
References
Weiner AB, Matulewicz RS, Eggener SE, Schaeffer EM. Increasing incidence of metastatic prostate cancer in the United States (2004–2013). Prostate Cancer Prostatic Dis. 2016;19(4):395–7.
Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019;10(2):63–89.
Shen MM, Abate-Shen C. Molecular genetics of prostate cancer: new prospects for old challenges. Genes Dev. 2010;24(18):1967–2000.
He G, Li M, Fang L, Xu L, Huang X, Zheng L, Yang L, Luo W, Cai Y, Ma W, et al. N-Myc induces the tumor progression of prostate cancer by regulating FSCN1. Oncol Rep. 2020;44(5):2265–74.
Yin Y, Xu L, Chang Y, Zeng T, Chen X, Wang A, Groth J, Foo W-C, Liang C, Hu H, et al. N-Myc promotes therapeutic resistance development of neuroendocrine prostate cancer by differentially regulating miR-421/ATM pathway. Mol Cancer. 2019;18(1):11.
Cai C, Dang W, Liu S, Huang L, Li Y, Li G, Yan S, Jiang C, Song X, Hu Y, et al. Anthrax toxin receptor 1/tumor endothelial marker 8 promotes gastric cancer progression through activation of the PI3K/AKT/mTOR signaling pathway. Cancer Sci. 2020;111(4):1132–45.
Dardenne E, Beltran H, Benelli M, Gayvert K, Berger A, Puca L, Cyrta J, Sboner A, Noorzad Z, MacDonald T, et al. N-Myc induces an EZH2-mediated transcriptional program driving neuroendocrine prostate cancer. Cancer Cell. 2016;30(4):563–77.
Lee JK, Phillips JW, Smith BA, Park JW, Stoyanova T, McCaffrey EF, Baertsch R, Sokolov A, Meyerowitz JG, Mathis C, et al. N-Myc drives neuroendocrine prostate cancer initiated from human prostate epithelial cells. Cancer Cell. 2016;29(4):536–47.
Gu J, Faundez V, Werner E. Endosomal recycling regulates anthrax toxin receptor 1/tumor endothelial marker 8-dependent cell spreading. Exp Cell Res. 2010;316(12):1946–57.
Weidner N, Carroll PR, Flax J, Blumenfeld W, Folkman J. Tumor angiogenesis correlates with metastasis in invasive prostate carcinoma. Am J Pathol. 1993;143(2):401–9.
Wang C-X, Xiong H-F, Wang S, Wang J, Nie X, Guo Q, Li X, Qi Y, Liu J-J, Lin B. Overexpression of TEM8 promotes ovarian cancer progression via Rac1/Cdc42/JNK and MEK/ERK/STAT3 signaling pathways. Am J Transl Res. 2020;12(7):3557–76.
Sun M, Li H, Liu J, Ning L, Zhao D, Liu S. The relationship between TEM8 and early diagnosis and prognosis of lung cancer. Minerva Medica. 2020. https://doi.org/10.23736/S0026-4806.20.06444-7.
Høye AM, Tolstrup SD, Horton ER, Nicolau M, Frost H, Woo JH, Mauldin JP, Frankel AE, Cox TR, Erler JT. Tumor endothelial marker 8 promotes cancer progression and metastasis. Oncotarget. 2018;9(53):30173–88.
Chen D, Bhat-Nakshatri P, Goswami C, Badve S, Nakshatri H. ANTXR1, a stem cell-enriched functional biomarker, connects collagen signaling to cancer stem-like cells and metastasis in breast cancer. Can Res. 2013;73(18):5821–33.
He G, Li M, Fang L, Xu L, Huang X, Zheng L, Yang L, Luo W, Cai Y, Ma W, et al. NMyc induces the tumor progression of prostate cancer by regulating FSCN1. Oncol Rep. 2020;44(5):2265–74.
Beltran H, Rickman DS, Park K, Chae SS, Sboner A, MacDonald TY, Wang Y, Sheikh KL, Terry S, Tagawa ST, et al. Molecular characterization of neuroendocrine prostate cancer and identification of new drug targets. Cancer Discov. 2011;1(6):487–95.
Mosquera JM, Beltran H, Park K, MacDonald TY, Robinson BD, Tagawa ST, Perner S, Bismar TA, Erbersdobler A, Dhir R, et al. Concurrent AURKA and MYCN Gene amplifications are harbingers of lethal treatmentrelated neuroendocrine prostate cancer. Neoplasia. 2013;15(1):1-IN4.
Meitar D, Crawford SE, Rademaker AW, Cohn SL. Tumor angiogenesis correlates with metastatic disease, N-myc amplification, and poor outcome in human neuroblastoma. J Clin Oncol. 1996;14(2):405–14.
St Croix B, Rago C, Velculescu V, Traverso G, Romans KE, Montgomery E, Lal A, Riggins GJ, Lengauer C, Vogelstein B, et al. Genes expressed in human tumor endothelium. Science (New York, NY). 2000;289(5482):1197–202.
Chaudhary A, Hilton MB, Seaman S, Haines DC, Stevenson S, Lemotte PK, Tschantz WR, Zhang XM, Saha S, Fleming T, et al. TEM8/ANTXR1 blockade inhibits pathological angiogenesis and potentiates tumoricidal responses against multiple cancer types. Cancer Cell. 2012;21(2):212–26.
Byrd TT, Fousek K, Pignata A, Szot C, Samaha H, Seaman S, Dobrolecki L, Salsman VS, Oo HZ, Bielamowicz K, et al. TEM8/ANTXR1-specific CAR T cells as a targeted therapy for triple-negative breast cancer. Cancer Res. 2018;78(2):489–500.
Acknowledgements
The authors thank the Center for Scientific Research of Anhui Medical University for their valuable help in our experiment.
Funding
This work was supported by grant from the National Natural Science Foundation of China (Grant No. 81972414) and Scientific Research Foundation of the Institute for Translational Medicine of Anhui Province (2017ZHYX02).
Author information
Authors and Affiliations
Contributions
YY and CL designed the research. WL, LY, YH, and SY collected the data. ML, LF, GH cooperated to perform the experiments and drafted the manuscript. YC, WM, HZ, ZT, LZ, and Louis BK reviewed and revised the manuscript. All authors have reviewed the article and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, M., Fang, L., Kwantwi, L.B. et al. N-Myc promotes angiogenesis and therapeutic resistance of prostate cancer by TEM8. Med Oncol 38, 127 (2021). https://doi.org/10.1007/s12032-021-01575-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-021-01575-x