Abstract
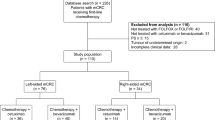
Neoadjuvant chemotherapy (NACT) prior to liver resection is advantageous for patients with colorectal cancer liver metastases (CLM). Bevacizumab- or cetuximab-based NACT may affect patient outcome and curative resection rate, but comparative studies on differential tumour regression grade (TRG) associated with distinct antibodies-associated regimens are lacking. Ninety-three consecutive patients received NACT plus bevacizumab (n = 46) or cetuximab (n = 47) followed by CLM resection. Pathological response was determined in each resected metastasis as TRG rated from 1 (complete) to 5 (no response). Except for KRAS mutations prevailing in bevacizumab versus cetuximab (57 vs. 21 %, p = 0.001), patients characteristics were well balanced. Median follow-up was 31 months (IQR 17–48). Bevacizumab induced significantly better pathological response rates (TRG1–3: 78 vs. 34 %, p < 0.001) as well as complete responses (TRG1: 13 vs. 0 %, p = 0.012) with respect to cetuximab. Three-year progression-free survival (PFS) and overall survival (OS) were not significantly different in the two cohorts. At multivariable analysis, significant association with pathological response was found for number of resected metastases (p = 0.015) and bevacizumab allocation (p < 0.001), while KRAS mutation showed only a trend. Significant association with poorer PFS and OS was found for low grades of pathological response (p = 0.009 and p < 0.001, respectively), R2 resection or presence of extrahepatic disease (both p < 0.001) and presence of KRAS mutation (p = 0.007 and p < 0.001, respectively). Bevacizumab-based regimens, although influenced by the number of metastases and KRAS status, improve significantly pathological response if compared to cetuximab-based NACT. Possible differential impact among regimens on patient outcome has still to be elucidated.


Similar content being viewed by others
References
Nordlinger B, van Cutsem E, Gruenberger T, et al. Combination of surgery and chemotherapy and the role of targeted agents in the treatment of patients with colorectal liver metastases: recommendations from an expert panel. Ann Oncol. 2009;20:985–92.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long term survival. Ann Surg. 2004;240:644–57.
Lam VW, Spiro C, Laurence JM, et al. A systematic review of clinical response and survival outcomes of downsizing systemic chemotherapy and rescue liver surgery in patients with initially unresectable colorectal liver metastases. Ann Surg Oncol. 2012;19:1292–301.
Nordlinger B, Sorbye H, Grimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomized controlled trial. Lancet. 2008;371:1007–16.
Folprecht G, Grothey A, Alberts S, Raab HR, Köhne CH. Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann Oncol. 2005;16:1311–9.
Van Cutsem E, Kohne CH, Lang I, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2011;29:2011–9.
Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360:1408–17.
Petrelli F, Barni S. Resectability and outcome with anti-EGFR agents in patients with KRAS wildtype colorectal liver-limited metastases. A metaanalysis. Int J Colorectal Dis. 2012;27:997–1004.
Folprecht G, Gruenberger T, Bechstein WO, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11:38–47.
Ye LC, Liu TS, Ren L, et al. Randomized controlled trial of cetuximab plus chemotherapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases. J Clin Oncol. 2013;. doi:10.1200/JCO.2012.44.8308.
de Jong MC, Pulitano C, Ribero D, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009;250(3):440–8.
Rees M, Tekkis PP, Welsh FK, et al. Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg. 2008;247:125–35.
Zakaria S, Donohue JH, Que FG, et al. Hepatic resection for colorectal metastases: Value for risk scoring systems? Ann Surg. 2007;246:183–91.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
Blazer DG III, Kishi Y, Maru DM, et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008;25:5344–51.
Rubbia-Brandt L, Giostra E, Brezault C, et al. Importance of histological tumor response assessment in predicting the outcome in patients with colorectal liver metastases treated with neo-adjuvant chemotherapy followed by liver surgery. Ann Oncol. 2007;18:299–304.
Adam R, Wicherts DA, de Haas RJ, et al. Complete pathologic response after preoperative chemotherapy for colorectal liver metastases: Myth or reality? J Clin Oncol. 2008;26:1635–41.
Klinger M, Dietmar Tamandl D, Eipeldauer S, et al. Bevacizumab improves pathological response of colorectal cancer liver metastases treated with XELOX/FOLFOX. Ann Surg Oncol. 2010;17:2059–65.
Ribero D, Wang H, Donadon M, et al. Bevacizumab improves pathologic response and protects against hepatic injury in patients treated with oxaliplatin-based chemotherapy for colorectal liver metastases. Cancer. 2007;12:2761–7.
Perrone F, Lampis A, Orsenigo M, et al. PI3KCA/PTEN deregulation contributes to impaired responses to cetuximab in metastatic colorectal cancer patients. Ann Oncol. 2009;20:84–90.
Molinari F, Felicioni L, Buscarino M, et al. Increased detection sensitivity for KRAS mutations enhances the prediction of anti-EGFR monoclonal antibody resistance in metastatic colorectal cancer. Clin Cancer Res. 2011;17:4901–14.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Zeger SL, Liang KY. Longitudinal data analysis using generalized linear models. Biometrica. 1986;73:13–22.
Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80:27–38.
Goeman JJ. L-1 penalized estimation in the cox proportional hazards model. Biom J. 2010;52(1):70–84.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61.
Chun YS, Vauthey J-N, Boonsirikamchai P, et al. Association of computed tomography morphologic criteria with pathologic response and survival in patients treated with bevacizumab for colorectal liver metastases. JAMA. 2009;302:2338–44.
Shindoh J, Loyer EM, Kopetz S, et al. Optimal morphologic response to preoperative chemotherapy: an alternate outcome end point before resection of hepatic colorectal metastases. J Clin Oncol. 2012;30:4566–72.
Maru DM, Kopetz S, Boonsirikamchai P, et al. Tumor thickness at the tumor-normal interface: a novel pathologic indicator of chemotherapy response in hepatic colorectal metastases. Am J Surg Pathol. 2010;34:1287–94.
Kishi Y, Zorzi D, Contreras CM, et al. Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2010;17:2870–6.
Gruenberger T, Arnold D, Rubbia-Brandt L. Pathologic response to bevacizumab-containing chemotherapy in patients with colorectal liver metastases and its correlation with survival. Surg Oncol. 2012;21:309–15.
Karapetis C-S, Khambata-Ford S, Jonker DJ, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359:1757–65.
Zlobec I, Bihl MP, Schwarb H, et al. Clinicopathological and protein characterization of BRAF- and K-RAS-mutated colorectal cancer and implications for prognosis. Int J Cancer. 2010;127:367–80.
Andreyev HJ, Norman AR, Cunningham D, et al. Kirsten ras mutations in patients with colorectal cancer: the ‘RASCAL II’ study. Br J Cancer. 2001;85:692–6.
Stremitzer S, Stift J, Gruenberger B, et al. KRAS status and outcome of liver resection after neoadjuvant chemotherapy including bevacizumab. Br J Surg. 2012;99:1575–82.
Nash GM, Gimbel M, Shia J, et al. KRAS mutation correlates with accelerated metastatic progression in patients with colorectal liver metastases. Ann Surg Oncol. 2010;17:572–8.
Tie J, Lipton L, Desai J, et al. KRAS mutation is associated with lung metastasis in patients with curatively resected colorectal cancer. Clin Cancer Res. 2011;17:1122–30.
Carey LA, Dees EC, Sawyer L, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–34.
Pietrantonio F, Orlandi A, Inno A, et al. Bevacizumab-based neoadjuvant chemotherapy for colorectal cancer liver metastases: pitfalls and helpful tricks in a review for clinicians. Crit Rev Oncol Hematol. 2015. doi:10.1016/j.critrevonc.2015.04.008.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
12032_2015_638_MOESM1_ESM.pptx
Distributions of three-category tumour regression grade (TRG) according to treatment group (bevacizumab- versus cetuximab-based neoadjuvant chemotherapy). TRG categories (TRG1–2: major-to-complete pathological response vs. TRG3: partial response vs. TRG4–5: no response) are shown as absolute percentages (bars). (PPTX 47 kb)
Rights and permissions
About this article
Cite this article
Pietrantonio, F., Mazzaferro, V., Miceli, R. et al. Pathological response after neoadjuvant bevacizumab- or cetuximab-based chemotherapy in resected colorectal cancer liver metastases. Med Oncol 32, 182 (2015). https://doi.org/10.1007/s12032-015-0638-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-015-0638-3