Abstract
Purpose
Elective surgical resection is the curative treatment for colorectal cancer (CRC). Up to 30 % of patients present as surgical emergencies. The objective was to determine the association between presenting with an emergency condition and consequent outcomes of CRC surgery in the Appalachian state of West Virginia (WV) in comparison to the rest of the USA.
Methods
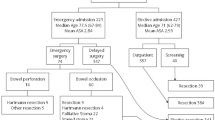
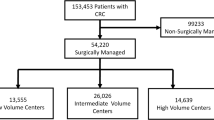
Patients diagnosed with CRC who underwent a surgical procedure from January 1, 2003 to December 31, 2007 were selected, and those with a diagnosis requiring emergency surgery were identified. Primary outcome measures were length of stay (LOS), total hospital charges, and inpatient death.
Results
Mean LOS was higher for WV. Mean charges were higher for the USA than for WV. Inpatient deaths in WV were greater than the rest of the USA. Those undergoing emergency surgery spent 51.9 % (β = 0.40) more days in the hospital than those who did not. For WV, LOS was 7.6 % (β = 0.07) higher than that of the US. Hospital charges for those that underwent emergency resection were 68.3 % (β = 0.52) higher than those who did not. The odds of in-hospital death were 1.68 (95 % CI = 1.42–1.98) times greater in WV than in the USA. Those that underwent emergency surgery had a nearly four times (OR 3.88; 95 % CI = 3.74–4.03) greater chance of in-hospital death.
Conclusions
The study stresses the ongoing burden of emergency surgeries in many states around the nation and the need to increase awareness about CRC screening practices, especially in patients who are at increased risk of the disease.
Similar content being viewed by others
References
Gellad ZF, Provenzale D. Colorectal cancer: national and international perspective on the burden of disease and public health impact. Gastroenterology. 2010;138(6):2177–90. doi:10.1053/j.gastro.2010.01.056.
Hao Y, Jemal A, Zhang X, Ward EM. Trends in colorectal cancer incidence rates by age, race/ethnicity, and indices of access to medical care, 1995–2004 (United States). Cancer Causes Control. 2009;20(10):1855–63. doi:10.1007/s10552-009-9379-y.
Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15(2):389–94. doi:10.1158/1055-9965.EPI-05-0678.
Hoff G, Dominitz JA. Contrasting US and European approaches to colorectal cancer screening: which is best? Gut. 2010;59(3):407–14. doi:10.1136/gut.2009.192948.
American Cancer Society. Colorectal cancer facts & figures 2011–2013. Atlanta: American Cancer Society; 2011.
Miller AB. Implementation of colon cancer screening: techniques, costs, and barriers. Gastroenterol Clin North Am. 2008;37(1):83–95. doi:10.1016/j.gtc.2007.12.015.
Redaelli A, Cranor CW, Okano GJ, Reese PR. Screening, prevention and socioeconomic costs associated with the treatment of colorectal cancer. Pharmacoeconomics. 2003;21(17):1213–38.
Cuffy M, Abir F, Audisio RA, Longo WE. Colorectal cancer presenting as surgical emergencies. Surg Oncol. 2004;13(2–3):149–57. doi:10.1016/j.suronc.2004.08.002.
Rabeneck L, Paszat LF, Li C. Risk factors for obstruction, perforation, or emergency admission at presentation in patients with colorectal cancer: a population-based study. Am J Gastroenterol. 2006;101(5):1098–103. doi:10.1111/j.1572-0241.2006.00488.x.
Kim J, Mittal R, Konyalian V, King J, Stamos MJ, Kumar RR. Outcome analysis of patients undergoing colorectal resection for emergent and elective indications. Am Surg. 2007;73(10):991–3.
Polednak AP. Inpatient hospital admission through an emergency department in relation to stage at diagnosis of colorectal cancer. Cancer Detect Prev. 2000;24(3):283–9.
Smothers L, Hynan L, Fleming J, Turnage R, Simmang C, Anthony T. Emergency surgery for colon carcinoma. Dis Colon Rectum. 2003;46(1):24–30. doi:10.1097/01.DCR.0000044719.17980.4C.
Diggs JC, Xu F, Diaz M, Cooper GS, Koroukian SM. Failure to screen: predictors and burden of emergency colorectal cancer resection. Am J Manag Care. 2007;13(3):157–64.
McGillicuddy EA, Schuster KM, Davis KA, Longo WE. Factors predicting morbidity and mortality in emergency colorectal procedures in elderly patients. Arch Surg. 2009;144(12):1157–62. doi:10.1001/archsurg.2009.203.
Harris JR, Brown PK, Coughlin S, et al. The cancer prevention and control research network. Prev Chronic Dis. 2005;2(1):A21.
Lengerich EJ, Wyatt SW, Rubio A, et al. The Appalachia Cancer Network: cancer control research among a rural, medically underserved population. J Rural Health. 2004;20(2):181–7.
American Cancer Society (South Atlantic Division). South Atlantic Division cancer facts & figures 2009. Atlanta: American Cancer Society; 2009.
The Appalachia Community Cancer Network. Colorectal cancer screening reimbursement and state legislation in Appalachia. http://www.accnweb.com/docs/2008/PolicyBrief1.pdf. Accessed 10/12, 2011.
State Cancer Profiles. Screening and risk factors report. http://statecancerprofiles.cancer.gov/risk/index.php?risk=09&sex=0&type=risk&stateFIPS=00&sortVariableName=default&sortOrder=default. Accessed 1/3, 2011.
American Cancer Society. Colorectal cancer facts & figures 2008–2010. Atlanta: American Cancer Society; 2008.
Etzioni DA, Beart Jr RW, Madoff RD, Ault GT. Impact of the aging population on the demand for colorectal procedures. Dis Colon Rectum. 2009;52(4):583–90. doi:10.1007/DCR.0b013e3181a1d183. discussion 590-1.
Hayanga AJ, Mukherjee D, Chang D, et al. Teaching hospital status and operative mortality in the United States: tipping point in the volume–outcome relationship following colon resections? Arch Surg. 2010;145(4):346–50. doi:10.1001/archsurg.2010.24.
Holt PR, Kozuch P, Mewar S. Colon cancer and the elderly: from screening to treatment in management of GI disease in the elderly. Best Pract Res Clin Gastroenterol. 2009;23(6):889–907. doi:10.1016/j.bpg.2009.10.010.
Qaseem A, Denberg TD, Hopkins RH, et al. Screening for colorectal cancer: a guidance statement from the American College of Physicians. Ann Intern Med. 2012;156:378–86.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Giovannucci E. Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr. 2001;131(11 Suppl):3109S–20.
Meyerhardt JA, Catalano PJ, Haller DG, et al. Impact of diabetes mellitus on outcomes in patients with colon cancer. J Clin Oncol. 2003;21(3):433–40.
Gross CP, Guo Z, McAvay GJ, Allore HG, Young M, Tinetti ME. Multimorbidity and survival in older persons with colorectal cancer. J Am Geriatr Soc. 2006;54(12):1898–904. doi:10.1111/j.1532-5415.2006.00973.x.
Halvorsen R, Palmquist R. The interpretation of dummy variables in semilogarithmic equations. Am Econ Rev. 1980;70(3):474–5. http://econpapers.repec.org/RePEc:aea:aecrev:v:70:y:1980:i:3:p:474-75.
Hernandez RA, de Verteuil RM, Fraser CM, Vale LD, Aberdeen Health Technology Assessment Group. Systematic review of economic evaluations of laparoscopic surgery for colorectal cancer. Colorectal Dis. 2008;10(9):859–68. doi:10.1111/j.1463-1318.2008.01609.x.
Wray CM, Ziogas A, Hinojosa MW, Le H, Stamos MJ, Zell JA. Tumor subsite location within the colon is prognostic for survival after colon cancer diagnosis. Dis Colon Rectum. 2009;52(8):1359–66. doi:10.1007/DCR.0b013e3181a7b7de.
Jubelirer SJ, Wells JB, Emmett M, Broce M. Incidence of colorectal cancer in West Virginia from 1993–1999: an update by gender, age, subsite and stage. W V Med J. 2003;99(5):182–6.
Heflin MT, Oddone EZ, Pieper CF, Burchett BM, Cohen HJ. The effect of comorbid illness on receipt of cancer screening by older people. J Am Geriatr Soc. 2002;50(10):1651–8.
Koroukian SM, Xu F, Bakaki PM, Diaz-Insua M, Towe TP, Owusu C. Comorbidities, functional limitations, and geriatric syndromes in relation to treatment and survival patterns among elders with colorectal cancer. J Gerontol A Biol Sci Med Sci. 2010;65(3):322–9. doi:10.1093/gerona/glp180.
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ. Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol. 2004;159(12):1160–7. doi:10.1093/aje/kwh161.
Ahluwalia IB, Tessaro I, Greenlund KJ, Ford ES. Factors associated with control of hypertension, hypercholesterolemia, and diabetes among low-income women in West Virginia. J Womens Health (Larchmt). 2010;19(3):417–24. doi:10.1089/jwh.2009.1590.
Mushinski M. Variation in in-hospital charges for colorectal cancer treatment. Stat Bull Metrop Insur Co. 1998;79(1):19–27.
Tessaro I, Mangone C, Parkar I, Pawar V. Knowledge, barriers, and predictors of colorectal cancer screening in an Appalachian church population. Prev Chronic Dis. 2006;3(4):A123.
Felsen CB, Piasecki A, Ferrante JM, Ohman-Strickland PA, Crabtree BF. Colorectal cancer screening among primary care patients: does risk affect screening behavior? J Community Health. 2011;36(4):605–11. doi:10.1007/s10900-010-9348-0.
Acknowledgments
The primary author was supported by a grant (1R24HS018622-01 PI: S. Madhavan) from the Agency of Healthcare Research and Quality during the conduct of this study.
Disclosure
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The authors claim no conflicts of interest. At the time the study was conducted, manuscript written, and sent for initial review, Neel A. Shah was a graduate student and PhD candidate at West Virginia University, School of Pharmacy, Morgantown, WV. At the time of acceptance and publication, Neel A. Shah was an employee of Amgen, Inc., Thousand Oaks, CA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, N.A., Halverson, J. & Madhavan, S. Burden of Emergency and Non-emergency Colorectal Cancer Surgeries in West Virginia and the USA. J Gastrointest Canc 44, 46–53 (2013). https://doi.org/10.1007/s12029-012-9455-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-012-9455-5