Abstract
Background
Both seizures and spreading depolarizations (SDs) are commonly detected using electrocorticography (ECoG) after severe traumatic brain injury (TBI). A close relationship between seizures and SDs has been described, but the implications of detecting either or both remain unclear. We sought to characterize the relationship between these two phenomena and their clinical significance.
Methods
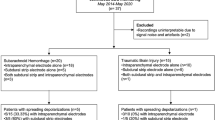
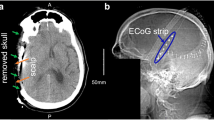
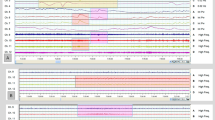
We performed a post hoc analysis of a prospective observational clinical study of patients with severe TBI requiring neurosurgery at five academic neurotrauma centers. A subdural electrode array was placed intraoperatively and ECoG was recorded during intensive care. SDs, seizures, and high-frequency background characteristics were quantified offline using published standards and terminology. The primary outcome was the Glasgow Outcome Scale-Extended score at 6 months post injury.
Results
There were 138 patients with valid ECoG recordings; the mean age was 47 ± 19 years, and 104 (75%) were men. Overall, 2,219 ECoG-detected seizures occurred in 38 of 138 (28%) patients in a bimodal pattern, with peak incidences at 1.7–1.8 days and 3.8–4.0 days post injury. Seizures detected on scalp electroencephalography (EEG) were diagnosed by standard clinical care in only 18 of 138 (13%). Of 15 patients with ECoG-detected seizures and contemporaneous scalp EEG, seven (47%) had no definite scalp EEG correlate. ECoG-detected seizures were significantly associated with the severity and number of SDs, which occurred in 83 of 138 (60%) of patients. Temporal interactions were observed in 17 of 24 (70.8%) patients with both ECoG-detected seizures and SDs. After controlling for known prognostic covariates and the presence of SDs, seizures detected on either ECoG or scalp EEG did not have an independent association with 6-month functional outcome but portended worse outcome among those with clustered or isoelectric SDs.
Conclusions
In patients with severe TBI requiring neurosurgery, seizures were half as common as SDs. Seizures would have gone undetected without ECoG monitoring in 20% of patients. Although seizures alone did not influence 6-month functional outcomes in this cohort, they were independently associated with electrographic worsening and a lack of motor improvement following surgery. Temporal interactions between ECoG-detected seizures and SDs were common and held prognostic implications. Together, seizures and SDs may occur along a dynamic continuum of factors critical to the development of secondary brain injury. ECoG provides information integral to the clinical management of patients with TBI.







Similar content being viewed by others
References
Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury–related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1.
Reddy GD, Gopinath S, Robertson C. Critical Care Management of the Patient with Traumatic Brain Injury. Semin Neurol. 2016;36(6):570–6.
Le Roux P, Menon DK, Citerio G, Vespa P, Bader MK, Brophy GM, et al. Consensus summary statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care : a statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(9):1189–209.
Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, et al. Consensus statement on continuous EEG in critically ill adults and children, part I: indications. J Clin Neurophysiol. 2015;32(2):87–95.
Waziri A, Claassen J, Stuart RM, Arif H, Schmidt JM, Mayer SA, et al. Intracortical electroencephalography in acute brain injury. Ann Neurol. 2009;66(3):366–77.
Vespa P, Tubi M, Claassen J, Buitrago-Blanco M, McArthur D, Velazquez AG, et al. Metabolic crisis occurs with seizures and periodic discharges after brain trauma. Ann Neurol. 2016;79(4):579–90.
Dreier JP. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med. 2011;17(4):439–47.
Hartings JA. Spreading depolarization monitoring in neurocritical care of acute brain injury. Curr Opin Crit Care. 2017;23(2):94–102.
Drenckhahn C, Winkler MK, Major S, Scheel M, Kang EJ, Pinczolits A, et al. Correlates of spreading depolarization in human scalp electroencephalography. Brain. 2012;135(Pt 3):853–68.
Hartings JA, Wilson JA, Hinzman JM, Pollandt S, Dreier JP, DiNapoli V, et al. Spreading depression in continuous electroencephalography of brain trauma. Ann Neurol. 2014;76(5):681–94.
Hartings JA, Andaluz N, Bullock MR, Hinzman JM, Mathern B, Pahl C, et al. Prognostic Value of Spreading Depolarizations in Patients With Severe Traumatic Brain Injury. JAMA Neurol. 2020;77(4):489–99.
Leao AAP. SPREADING DEPRESSION OF ACTIVITY IN THE CEREBRAL CORTEX. J Neurophysiol. 1944;7(6):359–90.
Fabricius M, Fuhr S, Willumsen L, Dreier JP, Bhatia R, Boutelle MG, et al. Association of seizures with cortical spreading depression and peri-infarct depolarisations in the acutely injured human brain. Clin Neurophysiol. 2008;119(9):1973–84.
Dreier JP, Major S, Pannek HW, Woitzik J, Scheel M, Wiesenthal D, et al. Spreading convulsions, spreading depolarization and epileptogenesis in human cerebral cortex. Brain. 2012;135(Pt 1):259–75.
Eickhoff M, Kovac S, Shahabi P, Ghadiri MK, Dreier JP, Stummer W, et al. Spreading depression triggers ictaform activity in partially disinhibited neuronal tissues. Exp Neurol. 2014;253:1–15.
Hablitz JJ, Heinemann U. Alterations in the microenvironment during spreading depression associated with epileptiform activity in the immature neocortex. Dev Brain Res. 1989;46(2):243–52.
Mody I, Lambert J, Heinemann U. Low extracellular magnesium induces epileptiform activity and spreading depression in rat hippocampal slices. J Neurophysiol. 1987;57(3):869–88.
Avoli M, Drapeau C, Louvel J, Pumain R, Olivier A, Villemure JG. Epileptiform activity induced by low extracellular magnesium in the human cortex maintained in vitro. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 1991;30(4):589–96.
Koroleva V, Bureš J. Cortical penicillin focus as a generator of repetitive spike-triggered waves of spreading depression in rats. Exp Brain Res. 1983;51(2):291–7.
Dreier JP, Isele T, Reiffurth C, Offenhauser N, Kirov SA, Dahlem MA, et al. Is spreading depolarization characterized by an abrupt, massive release of gibbs free energy from the human brain cortex? Neuroscientist. 2013;19(1):25–42.
Tamim I, Chung DY, de Morais AL, Loonen IC, Qin T, Misra A, et al. Spreading depression as an innate antiseizure mechanism. Nat Commun. 2021;12(1):1–15.
Hinzman JM, DiNapoli VA, Mahoney EJ, Gerhardt GA, Hartings JA. Spreading depolarizations mediate excitotoxicity in the development of acute cortical lesions. Exp Neurol. 2015;267:243–53.
Hinzman JM, Wilson JA, Mazzeo AT, Bullock MR, Hartings JA. Excitotoxicity and metabolic crisis are associated with spreading depolarizations in severe traumatic brain injury patients. J Neurotrauma. 2016;33(19):1775–83.
Vespa P, McArthur D, Xu Y, Eliseo M, Etchepare M, Dinov I, et al. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010;75(9):792–8.
Tubi MA, Lutkenhoff E, Blanco MB, McArthur D, Villablanca P, Ellingson B, et al. Early seizures and temporal lobe trauma predict post-traumatic epilepsy: a longitudinal study. Neurobiol Dis. 2019;123:115–21.
Lückl J, Lemale CL, Kola V, Horst V, Khojasteh U, Oliveira-Ferreira AI, et al. The negative ultraslow potential, electrophysiological correlate of infarction in the human cortex. Brain. 2018;141(6):1734–52.
Hartings JA, Watanabe T, Bullock MR, Okonkwo DO, Fabricius M, Woitzik J, et al. Spreading depolarizations have prolonged direct current shifts and are associated with poor outcome in brain trauma. Brain. 2011;134(5):1529–40.
Helbok R, Hartings JA, Schiefecker A, Balança B, Jewel S, Foreman B, et al., editors. What should a clinician do when spreading depolarizations are observed in a patient? Neurocritical care; 2020: Springer.
Dreier JP, Fabricius M, Ayata C, Sakowitz OW, William Shuttleworth C, Dohmen C, et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: review and recommendations of the COSBID research group. J Cereb Blood Flow Metab. 2017;37(5):1595–625.
Hirsch L, LaRoche S, Gaspard N, Gerard E, Svoronos A, Herman S, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30(1):1–27.
Lee H, Mizrahi MA, Hartings JA, Sharma S, Pahren L, Ngwenya LB, et al. Continuous Electroencephalography After Moderate to Severe Traumatic Brain Injury. Crit Care Med. 2019;47(4):574–82.
Wickham H, Chang W, Wickham MH. Package ‘ggplot2.’ Create Elegant Data Visualisations Using the Grammar of Graphics Version. 2016;2(1):1–189.
Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
Venables W, Ripley B, Hornik K, Gebhardt A. Package ‘Mass’. https://cran.r-project.org/web/packages/MASS/.
Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5(8):e165; discussion e.
Struck AF, Tabaeizadeh M, Schmitt SE, Ruiz AR, Swisher CB, Subramaniam T, et al. Assessment of the validity of the 2HELPS2B score for inpatient seizure risk prediction. JAMA Neurol. 2020;77(4):500–7.
Hartings JA, Shuttleworth CW, Kirov SA, Ayata C, Hinzman JM, Foreman B, et al. The continuum of spreading depolarizations in acute cortical lesion development: Examining Leao’s legacy. J Cereb Blood Flow Metab. 2017;37(5):1571–94.
Claassen J, Perotte A, Albers D, Kleinberg S, Schmidt JM, Tu B, et al. Nonconvulsive seizures after subarachnoid hemorrhage: Multimodal detection and outcomes. Ann Neurol. 2013;74(1):53–64.
Vespa PM, Miller C, McArthur D, Eliseo M, Etchepare M, Hirt D, et al. Nonconvulsive electrographic seizures after traumatic brain injury result in a delayed, prolonged increase in intracranial pressure and metabolic crisis. Crit Care Med. 2007;35(12):2830.
Dreier JP, Reiffurth C. The stroke-migraine depolarization continuum. Neuron. 2015;86(4):902–22.
Li Z, Song Y, Xiao G, Gao F, Xu S, Wang M, et al. Bio-electrochemical microelectrode arrays for glutamate and electrophysiology detection in hippocampus of temporal lobe epileptic rats. Anal Biochem. 2018;550:123–31.
Zhou N, Rungta RL, Malik A, Han H, Wu DC, MacVicar BA. Regenerative glutamate release by presynaptic NMDA receptors contributes to spreading depression. J Cereb Blood Flow Metab. 2013;33(10):1582–94.
Revankar GS, Winkler MK, Major S, Schoknecht K, Heinemann U, Woitzik J, et al. Spreading depolarizations and seizures in clinical subdural electrocorticographic recordings. Seizures in Critical Care: Springer; 2017. p. 77–90.
Revah O, Lasser-Katz E, Fleidervish IA, Gutnick MJ. The earliest neuronal responses to hypoxia in the neocortical circuit are glutamate-dependent. Neurobiol Dis. 2016;95:158–67.
Dietz RM, Weiss JH, Shuttleworth CW. Zn2+ influx is critical for some forms of spreading depression in brain slices. J Neurosci. 2008;28(32):8014–24.
Aiba I, Shuttleworth CW. Sustained NMDA receptor activation by spreading depolarizations can initiate excitotoxic injury in metabolically compromised neurons. J Physiol. 2012;590(22):5877–93.
Köhling R, Koch U, Hagemann G, Redecker C, Straub H, Speckmann E-J. Differential sensitivity to induction of spreading depression by partial disinhibition in chronically epileptic human and rat as compared to native rat neocortical tissue. Brain Res. 2003;975(1–2):129–34.
Allen NJ, Rossi DJ, Attwell D. Sequential release of GABA by exocytosis and reversed uptake leads to neuronal swelling in simulated ischemia of hippocampal slices. J Neurosci. 2004;24(15):3837–49.
Fabricius M, Jensen LH, Lauritzen M. Microdialysis of interstitial amino acids during spreading depression and anoxic depolarization in rat neocortex. Brain Res. 1993;612(1–2):61–9.
Jansen NA, Dehghani A, Linssen MM, Breukel C, Tolner EA, van den Maagdenberg AM. First FHM3 mouse model shows spontaneous cortical spreading depolarizations. Annals of clinical and translational neurology. 2020;7(1):132–8.
Claes L, Del-Favero J, Ceulemans B, Lagae L, Van Broeckhoven C, De Jonghe P. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. The American Journal of Human Genetics. 2001;68(6):1327–32.
Escayg A, MacDonald BT, Meisler MH, Baulac S, Huberfeld G, An-Gourfinkel I, et al. Mutations of SCN1A, encoding a neuronal sodium channel, in two families with GEFS+ 2. Nat Genet. 2000;24(4):343–5.
Gursoy-Ozdemir Y, Qiu J, Matsuoka N, Bolay H, Bermpohl D, Jin H, et al. Cortical spreading depression activates and upregulates MMP-9. J Clin Investig. 2004;113(10):1447–55.
Sadeghian H, Lacoste B, Qin T, Toussay X, Rosa R, Oka F, et al. Spreading depolarizations trigger caveolin-1–dependent endothelial transcytosis. Ann Neurol. 2018;84(3):409–23.
Dreier JP, Lemale CL, Kola V, Friedman A, Schoknecht K. Spreading depolarization is not an epiphenomenon but the principal mechanism of the cytotoxic edema in various gray matter structures of the brain during stroke. Neuropharmacology. 2018;134:189–207.
Mestre H, Du T, Sweeney AM, Liu G, Samson AJ, Peng W, et al. Cerebrospinal fluid influx drives acute ischemic tissue swelling. Science. 2020;367(6483).
Ullah G, Wei Y, Dahlem MA, Wechselberger M, Schiff SJ. The role of cell volume in the dynamics of seizure, spreading depression, and anoxic depolarization. PLoS computational biology. 2015;11(8):e1004414.
Takizawa T, Qin T, Lopes de Morais A, Sugimoto K, Chung JY, Morsett L, et al. Non-invasively triggered spreading depolarizations induce a rapid pro-inflammatory response in cerebral cortex. Journal of Cerebral Blood Flow & Metabolism. 2020;40(5):1117–31.
Claassen J, Albers D, Schmidt JM, De Marchis GM, Pugin D, Falo CM, et al. Nonconvulsive seizures in subarachnoid hemorrhage link inflammation and outcome. Ann Neurol. 2014;75(5):771–81.
Winkler MK, Chassidim Y, Lublinsky S, Revankar GS, Major S, Kang EJ, et al. Impaired neurovascular coupling to ictal epileptic activity and spreading depolarization in a patient with subarachnoid hemorrhage: possible link to blood–brain barrier dysfunction. Epilepsia. 2012;53:22–30.
Maslarova A, Alam M, Reiffurth C, Lapilover E, Gorji A, Dreier JP. Chronically epileptic human and rat neocortex display a similar resistance against spreading depolarization in vitro. Stroke. 2011;42(10):2917–22.
Tomkins O, Friedman O, Ivens S, Reiffurth C, Major S, Dreier J, et al. Blood–brain barrier disruption results in delayed functional and structural alterations in the rat neocortex. Neurobiol Dis. 2007;25(2):367–77.
Wei Y, Ullah G, Schiff SJ. Unification of neuronal spikes, seizures, and spreading depression. J Neurosci. 2014;34(35):11733–43.
Launey Y, Fryer TD, Hong YT, Steiner LA, Nortje J, Veenith TV, et al. Spatial and Temporal Pattern of Ischemia and Abnormal Vascular Function Following Traumatic Brain Injury. JAMA Neurol. 2020;77(3):339–49.
Hartings JA, Li C, Hinzman JM, Shuttleworth CW, Ernst GL, Dreier JP, et al. Direct current electrocorticography for clinical neuromonitoring of spreading depolarizations. J Cereb Blood Flow Metab. 2017;37(5):1857–70.
Funding
This study was funded by the US Army Congressionally Directed Medical Research Program Psychological Health/Traumatic Brain Injury Research Program (W81XWH-08–2-0016). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Defense.
Author information
Authors and Affiliations
Contributions
Brandon Foreman conceived and designed the analysis, contributed data or analysis tools, performed the analysis, and wrote the article. Hyunjo Lee contributed data or analysis tools and performed the analysis. David O. Okonkwo collected and contributed data and contributed to critical revisions of the manuscript. Anthony J. Strong collected and contributed data and contributed to critical revisions of the manuscript. Clemens Pahl collected and contributed data. Lori A. Shutter collected and contributed data and contributed to critical revisions of the manuscript. Jens P. Dreier conceived and designed the analysis, contributed data or analysis tools, and contributed to critical revisions of the manuscript. Laura B Ngwenya contributed to critical revisions of the manuscript. Jed A. Hartings conceived and designed the study and the analysis, contributed data or analysis tools, and wrote the article. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Foreman reports grant funding from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (K23NS101123), the US Department of Defense (W81XWH1620020, W81XWH1920013), and the National Science Foundation (IIS1838730) and personal fees from UCB Pharma and the Micromed Group outside the submitted work. Dr. Dreier reports grants from the DFG Deutsche Forschungsgemeinschaft (German Research Council) (DFG DR 323/5–1 and DFG DR 323/10–1) and BMBF Bundesministerium fuer Bildung und Forschung (Era-Net Neuron EBio2 with funds from BMBF 0101EW2004).
Ethical approval and informed consent
This study adheres to ethical guidelines, and ethical approval is reported in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the collection “Spreading Cortical Depolarization”.
Rights and permissions
About this article
Cite this article
Foreman, B., Lee, H., Okonkwo, D.O. et al. The Relationship Between Seizures and Spreading Depolarizations in Patients with Severe Traumatic Brain Injury. Neurocrit Care 37 (Suppl 1), 31–48 (2022). https://doi.org/10.1007/s12028-022-01441-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01441-2