Abstract
Background
Intracranial hemorrhage (ICH) may occur in patients admitted to the hospital for unrelated medical conditions, resulting in prolonged hospitalization and worse prognosis. We aim to assess the clinical presentation and outcomes of in-hospital ICH compared to patients with ICH presenting from the community.
Methods
We conducted a retrospective analysis of all acute stroke alerts diagnosed with ICH in an urban academic hospital over a 4-year period. Demographics, clinical presentation, use of antithrombotic therapy, and presence of coagulopathy were recorded. ICH score and a sequential organ failure assessment score were calculated during the initial assessment. Initial head computed tomography was reviewed to determine ICH subtype, location, and volume of the hematoma. In-hospital mortality and discharge disposition were used as surrogate of clinical outcome.
Results
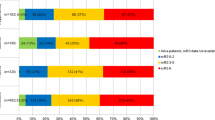
From the 1965 stroke alert cases analyzed over the studied years, 145 (7.4%) were diagnosed with ICH. Overall, the mean age was 62.9 ± 13.9 and 53.7% were women. Thirty-two patients (22%) developed ICH in the inpatient setting and 113 (78%) presented from the community. Systolic blood pressure at presentation was lower in the in-hospital group (p < 0.01). Inpatients who developed ICH were more likely than community ICH patients to be on combination of antiplatelet agents (21.9% vs. 5.3%, p < 0.05) or therapeutic heparinoids (21.9% vs. 0.9%, p < 0.01). Also, In-hospital ICH patients had a higher rate of spontaneous or iatrogenic coagulopathy (65.6% vs. 10.6%, p < 0.01) and thrombocytopenia (31.3% vs. 1.8%, p < 0.01). Lobar hemorrhages were more prevalent in the in-hospital group (82.6% vs. 39.1%, p < 0.01) and the mean hematoma volume was higher (40.9 ± 43.1 mL vs. 24.1 ± 30.4 mL; p < 0.02). Median ICH score in the in-hospital group was not statistically different from the emergency department group: 2 (IQR: 0–3) versus 1 (IQR: 0–3). When comparing patients with in-hospital ICH and those from the community, the short-term mortality was higher in the former group (81% vs. 31%, p < 0.01). The incidence of withdrawal of life-sustaining therapies as a proximate mechanism of death was higher, but not statistically significant, in the in-hospital group (86% vs. 61%).
Conclusion
ICH is a critical complication in the inpatient setting, predominantly occurring in already ill patients with underlying spontaneous or iatrogenic coagulopathy. Large volume lobar intraparenchymal hemorrhage is a common radiographic finding. ICH is frequently a catastrophic event and powerfully weighs in with end-of-life discussion, resulting in high short-term mortality rate.


Similar content being viewed by others
References
Rincon F, Mayer S. The epidemiology of intracerebral hemorrhage in the United States from 1979 to 2008. Neurocrit Care. 2013;19:95–102.
Hemphill CJ, Greenberg SM, Anderson CS, et al. Guidelines for the management of intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Hemphill CJ, Adeoye OM, Alexander DN, et al. Clinical performance measures for adults hospitalized with inctracerebral hemorrhage. Stroke. 2018;49:243–61.
Del Brutto VJ, Ardelt AA, Loggini A, et al. Clinical characteristics and emergent therapeutic interventions in patients evaluated through the in-hospital stroke alert protocol. J Stroke Cerebrovasc Dis. 2019;5:1362–70.
Gallagher TK, Thomas KA, Ladner DP, et al. Incidence and risk factors of intracranial hemorrhage in liver transplant recipients. Transplantation. 2018;102:448–53.
Tahir RA, Rotman LE, Davis MC, et al. Intracranial hemorrhage in patients with a left ventricular assist device. World Neurosurg. 2018;113:714–21.
Cavayas YA, Del Sorbo L, Fan E. Intracranial hemorrhage in adults on ECMO. Perfusion. 2018;33:42–50.
Hemphill JC, Bonovich DC, Besmertis L, Manley GT, Johnson SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32:891–7.
Wippold FJ. Expert panel on neurologic imaging. Focal neurologic deficit. Am J Neuroradiol. 2008;29:1998–2000.
Vincent JL, De Mendonca A, Cabtraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med. 1998;26:1793–800.
Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27:1304–5.
Belagaje SR, Zander K, Thackeray L, Gupta R. Disposition to home or acute rehabilitation is associated with a favorable clinical outcome in the SENTIS trial. J Neurointerv Surg. 2015;7:322–5.
Qureshi A, Chaudhry S, Sapkota B, Rodriguez G, Suri M. Discharge destination as a surrogate for modified rankin scale defined outcomes at 3- and 12-months poststroke among stroke survivors. Arch Phys Med Rehabil. 2012;93:1408–13.
Zhang Q, Yang Y, Saver J. Discharge destination after acute hospitalization strongly predicts three month disability outcome in ischemic stroke. Restor Neurol Neurosci. 2015;33:771–5.
Li Y, Gregory YH. Anticoagulation resumption after intracerebral hemorrhage. Curr Atheroscler Rep. 2018;20:32.
Goldstein J, Greenberg S. Should anticoagulation be resumed after intracerebral hemorrhage? Clevel Clin J Med. 2010;77:791.
Dayyani F, Mougalian SS, Naqvi K, et al. Intracranial hemorrhage (ICH) in patients (Pts) presenting with myeloid leukemia to a Tertiary Care Center. Blood. 2010;116(21):2170.
Chen CY, Tai C, Cheng A, et al. Intracranial hemorrhage in adult patients with hematological malignancies. BMC Med. 2012;10:97.
Owattanapanich W, Chirayu UA. Intracranial hemorrhage in patients with hematologic disorders: prevalence and predictive factors. J Med Assoc Thai. 2016;99:15–24.
Schiffer CA, Bohlke K, Delaney M, et al. Platelet transfusion for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;36:283–99.
Chern J, Tsung AJ, Humphries W, Sawaya R, Lang FF. Clinical outcome of leukemia patients with intracranial hemorrhage. J Neurosurg. 2011;115:268–72.
Flaherty ML, Haverbusch M, Sekar P, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66:1182–6.
Author information
Authors and Affiliations
Contributions
A.L. and V.D.B. were responsible for study concept, design, analysis, and drafting the manuscript. F.E.A., Z.B., F.S., C.M, and R.C. were responsible for data collection and analysis. J.B. and F.G. were responsible for critical revision of the manuscript. A.A. was responsible for the approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Source of support
This study received no external funding.
Conflict of interest
The authors declare that they have nothing to disclose.
Ethical Approval/Informed Consent
This study was approved by the University of Chicago Medical Center (UCMC) Institutional Review Board and ethics standards committee with a waiver of informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Loggini, A., Del Brutto, V.J., El Ammar, F. et al. Intracranial Hemorrhage in Hospitalized Patients: An Infrequently Studied Condition with High Mortality. Neurocrit Care 33, 725–731 (2020). https://doi.org/10.1007/s12028-020-00946-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-00946-y