Abstract
Background
Extracorporeal membrane oxygenation (ECMO) is associated with neurologic morbidity and mortality. We investigated whether cerebral regional oxygen saturation (rSO2) is associated with neurologic outcomes and survival in children on ECMO.
Methods
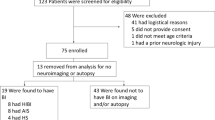
This was a retrospective observational study of children aged 1 day to 20 years who underwent ECMO with routine cerebral rSO2 monitoring in the pediatric intensive care unit at a single academic center between February 2008 and September 2014. We collected all serial rSO2 values recorded in the electronic medical record during the ECMO course. Favorable outcome was defined as survival with Pediatric Cerebral Performance Category (PCPC) ≤ 2 at hospital discharge or no decline from baseline PCPC.
Results
We reviewed data from 153 patients who underwent 156 ECMO runs. The median age was 12.5 days (interquartile range [IQR], 2 days—15 months). Ninety-nine (64%) patients survived to hospital discharge, and 82/99 (83%) survivors had favorable neurologic outcome by discharge PCPC. Neuroimaging studies were obtained in 135 (87%) patients, 59 (44%) of which showed abnormal findings. Ninety-two (59%) patients had any rSO2 ≤ 50%, 60 (38%) had any rSO2 decline > 20% from baseline, and 26 (17%) had any rSO2 decline > 20% from the reading 1 h prior. Any rSO2 ≤ 50% and any rSO2 decline > 20% from baseline were each associated with unfavorable outcome at hospital discharge (multivariable-adjusted odds ratio [OR], 2.82 [95% CI 1.10–7.25] and 4.52 [95% CI 1.76–11.58], respectively). rSO2 decline > 20% from the reading 1 h prior was not significantly associated with the outcomes.
Conclusion
Among children in one institution who underwent routine clinical rSO2 monitoring during ECMO, rSO2 decline was associated with unfavorable short-term neurologic outcome and death after adjusting for potential confounders. The effectiveness of initiating early preventative measures in these high-risk patients needs further study.

Similar content being viewed by others
References
Makdisi G, Wang IW. Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J Thorac Dis. 2015;7:E166–76.
Thiagarajan RR, Barbaro RP, Rycus PT, et al. Extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:60–7.
Barbaro RP, Paden ML, Guner YS, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:456–63.
Polito A, Barrett CS, Wypij D, et al. Neurologic complications in neonates supported with extracorporeal membrane oxygenation. An analysis of ELSO registry data. Intensive Care Med. 2013;39:1594–601.
Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. 2007;116:1693–700.
Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. Pediatr Crit Care Med. 2009;10:445–51.
Cengiz P, Seidel K, Rycus PT, Brogan TV, Roberts JS. Central nervous system complications during pediatric extracorporeal life support: incidence and risk factors. Crit Care Med. 2005;33:2817–24.
Weber TR, Kountzman B. Extracorporeal membrane oxygenation for nonneonatal pulmonary and multiple-organ failure. J Pediatr Surg. 1998;33:1605–9.
Fenik JC, Rais-Bahrami K. Neonatal cerebral oximetry monitoring during ECMO cannulation. J Perinatol. 2009;29:376–81.
Liem KD, Hopman JC, Oeseburg B, de Haan AF, Festen C, Kollee LA. Cerebral oxygenation and hemodynamics during induction of extracorporeal membrane oxygenation as investigated by near infrared spectrophotometry. Pediatrics. 1995;95:555–61.
Van Heijst A, Liem D, Hopman J, Van Der Staak F, Sengers R. Oxygenation and hemodynamics in left and right cerebral hemispheres during induction of veno-arterial extracorporeal membrane oxygenation. J Pediatr. 2004;144:223–8.
Tweed A, Cote J, Lou H, Gregory G, Wade J. Impairment of cerebral blood flow autoregulation in the newborn lamb by hypoxia. Pediatr Res. 1986;20:516–9.
Short BL, Walker LK, Traystman RJ. Impaired cerebral autoregulation in the newborn lamb during recovery from severe, prolonged hypoxia, combined with carotid artery and jugular vein ligation. Crit Care Med. 1994;22:1262–8.
Short BL, Walker LK, Bender KS, Traystman RJ. Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr Res. 1993;33:289–94.
Salen P, Melniker L, Chooljian C, et al. Does the presence or absence of sonographically identified cardiac activity predict resuscitation outcomes of cardiac arrest patients? Am J Emerg Med. 2005;23:459–62.
Paden ML, Conrad SA, Rycus PT, Thiagarajan RR, Registry E. Extracorporeal life support organization registry report 2012. ASAIO J. 2013;59:202–10.
Maldonado Y, Singh S, Taylor MA. Cerebral near-infrared spectroscopy in perioperative management of left ventricular assist device and extracorporeal membrane oxygenation patients. Curr Opin Anaesthesiol. 2014;27:81–8.
Yu Y, Lu Y, Meng L, Han R. Monitoring cerebral ischemia using cerebral oximetry: pros and cons. J Biomed Res. 2015;30:1.
Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Murkin JM, Adams SJ, Novick RJ, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Sood ED, Benzaquen JS, Davies RR, Woodford E, Pizarro C. Predictive value of perioperative near-infrared spectroscopy for neurodevelopmental outcomes after cardiac surgery in infancy. J Thorac Cardiovasc Surg. 2013;145:438–45 (discussion 44–5).
Wong JK, Smith TN, Pitcher HT, Hirose H, Cavarocchi NC. Cerebral and lower limb near-infrared spectroscopy in adults on extracorporeal membrane oxygenation. Artif Organs. 2012;36:659–67.
Kurth CD, Steven JM, Nicolson SC. Cerebral oxygenation during pediatric cardiac surgery using deep hypothermic circulatory arrest. Anesthesiology. 1995;82:74–82.
Zheng F, Sheinberg R, Yee MS, Ono M, Zheng Y, Hogue CW. Cerebral near-infrared spectroscopy monitoring and neurologic outcomes in adult cardiac surgery patients: a systematic review. Anesth Analg. 2013;116:663–76.
Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74.
Fiser DH, Long N, Roberson PK, Hefley G, Zolten K, Brodie-Fowler M. Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit Care Med. 2000;28:2616–20.
Cashen K, Reeder R, Dalton HJ, et al. Functional status of neonatal and pediatric patients after extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2017;18:561–70.
Lin JJ, Banwell BL, Berg RA, et al. Electrographic seizures in children and neonates undergoing extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2017;18:249–57.
Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62:44–54 (discussion-5).
Lima A, van Bommel J, Jansen TC, Ince C, Bakker J. Low tissue oxygen saturation at the end of early goal-directed therapy is associated with worse outcome in critically ill patients. Crit Care. 2009;13(Suppl 5):S13.
Storm C, Leithner C, Krannich A, et al. Regional cerebral oxygen saturation after cardiac arrest in 60 patients–a prospective outcome study. Resuscitation. 2014;85:1037–41.
Tsuji M, Saul JP, du Plessis A, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics. 2000;106:625–32.
Muehlschlegel S, Selb J, Patel M, et al. Feasibility of NIRS in the neurointensive care unit: a pilot study in stroke using physiological oscillations. Neurocrit Care. 2009;11:288–95.
Liem KD, Hopman JC, Kollee LA, Oeseburg B. Assessment of cerebral oxygenation and hemodynamics by near infrared spectrophotometry during induction of ECMO: preliminary results. The ECMO Research Group. Adv Exp Med Biol. 1992;317:841–6.
Ejike JC, Schenkman KA, Seidel K, Ramamoorthy C, Roberts JS. Cerebral oxygenation in neonatal and pediatric patients during veno-arterial extracorporeal life support. Pediatr Crit Care Med. 2006;7:154–8.
Papademetriou MD, Tachtsidis I, Elliot MJ, Hoskote A, Elwell CE. Multichannel near infrared spectroscopy indicates regional variations in cerebral autoregulation in infants supported on extracorporeal membrane oxygenation. J Biomed Opt. 2012;17:067008.
Papademetriou MD, Tachtsidis I, Leung TS, Elliott MJ, Hoskote A, Elwell CE. Cerebral and peripheral tissue oxygenation in children supported on ECMO for cardio-respiratory failure. Adv Exp Med Biol. 2010;662:447–53.
Clair MP, Rambaud J, Flahault A, et al. Prognostic value of cerebral tissue oxygen saturation during neonatal extracorporeal membrane oxygenation. PLoS ONE. 2017;12:e0172991.
Mateen FJ, Muralidharan R, Shinohara RT, Parisi JE, Schears GJ, Wijdicks EF. Neurological injury in adults treated with extracorporeal membrane oxygenation. Arch Neurol. 2011;68:1543–9.
Acknowledgements
The authors are thankful to Claire Levine, MS, ELS, Department of Anesthesiology and Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA, for the final editing of the text.
Funding
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Numbers K23NS076674, R21HD096389 and R01NS106292 (MMB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12028_2019_892_MOESM1_ESM.tif
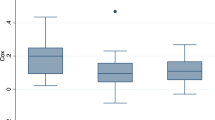
Percentage of time cerebral regional oxygen saturation (rSO2) was ≤ 40% during extracorporeal membrane oxygenation (ECMO) distributed by neurologic outcome at hospital discharge. Neurologic outcome was assessed by Pediatric Cerebral Performance Category. Results of the nonparametric test suggested a significant difference in the median percentage of time that rSO2 was ≤ 40% between patients with favorable and unfavorable outcomes (p < 0.001). (TIFF 170 kb)
12028_2019_892_MOESM2_ESM.tif
Percentage of time cerebral regional oxygen saturation (rSO2) was ≤ 50% during extracorporeal membrane oxygenation (ECMO) distributed by neurologic outcome at hospital discharge. Neurologic outcome was assessed by Pediatric Cerebral Performance Category. Results of the nonparametric test suggested a significant difference in the median percentage of time rSO2 was ≤ 50% between patients with favorable and unfavorable outcomes (p < 0.001). (TIFF 170 kb)
12028_2019_892_MOESM3_ESM.tif
Comparison of the time percentage that cerebral regional oxygen saturation (rSO2) was reduced > 20% from the baseline value during extracorporeal membrane oxygenation (ECMO) between patients with favorable and unfavorable neurologic outcome at hospital discharge. Neurologic outcome was assessed by Pediatric Cerebral Performance Category. Results of the nonparametric test suggested a significant difference in the median percentage of time that rSO2 was reduced > 20% from baseline between patients with favorable and unfavorable outcomes (p = 0.008). (TIFF 206 kb)
Rights and permissions
About this article
Cite this article
Tsou, PY., Garcia, A.V., Yiu, A. et al. Association of Cerebral Oximetry with Outcomes after Extracorporeal Membrane Oxygenation. Neurocrit Care 33, 429–437 (2020). https://doi.org/10.1007/s12028-019-00892-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00892-4