Abstract
Background
Quantitative electroencephalogram (EEG) analysis has shown promising results in studying brain injury and functional recovery after cardiac arrest (CA). However, whether the quantitative characteristics of EEG, as potential indicators of neurological prognosis, are influenced by CA causes is unknown. The purpose of this study was designed to compare the quantitative characteristics of early post-resuscitation EEG between asphyxial CA (ACA) and ventricular fibrillation CA (VFCA) in rats.
Methods
Thirty-two Sprague–Dawley rats of both sexes were randomized into either ACA or VFCA group. Cardiopulmonary resuscitation was initiated after 5-min untreated CA. Characteristics of early post-resuscitation EEG were compared, and the relationships between quantitative EEG features and neurological outcomes were investigated.
Results
Compared with VFCA, serum level of S100B, neurological deficit score and brain histopathologic damage score were dramatically higher in the ACA group. Quantitative measures of EEG, including onset time of EEG burst, time to normal trace, burst suppression ratio, and information quantity, were significantly lower for CA caused by asphyxia and correlated with the 96-h neurological outcome and survival.
Conclusions
Characteristics of earlier post-resuscitation EEG differed between cardiac and respiratory causes. Quantitative measures of EEG not only predicted neurological outcome and survival, but also have the potential to stratify CA with different causes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac arrest (CA) remains a major public health problem all over the world [1]. The common causes of non-traumatic CA are ventricular fibrillation CA (VFCA) and asphyxial CA (ACA) [2, 3]. Although the initial success of cardiopulmonary resuscitation (CPR) is approximately 39%, the majority of victims die within 72 h of hospital admission [4]. Among patients who achieved restoration of spontaneous circulation (ROSC), two-thirds died due to significant neurological disability after cerebral ischemia and reperfusion [4]. In addition to the unsatisfactory outcome is the fact that CA of respiratory causes are associated with a poor prognosis, even treated with therapeutic hypothermia [5]. The greatest post-resuscitation emphasis has therefore been on minimizing brain injury together with the aim to preserve neurological function [6]. Early and reliable prediction of outcome may be helpful in clinical decision making, such as stratifying CA patients and determining who would benefit from alternative or aggressive post-resuscitation interventions.
The electroencephalogram (EEG) has been frequently employed for neuromonitoring and prognostication in comatose survivors after CA due to its real-time measurement of brain function [7]. Earlier qualitative studies indicated that a continuous pattern of EEG within 12 h was associated with a good outcome, while isoelectric, low voltage or burst suppression at 24 h was associated with a poor outcome [8]. Recent clinical studies demonstrated that quantitative EEG analysis, including burst suppression ratio (BSR), time to normal trace (TTNT), and approximate entropy, was promising for the prediction of neurological outcome and survival at the earlier phase after CA [9–11].
Despite the utility of EEG in prognosis in CA, the majority of the reported studies are focused on CA due to cardiac causes. Since CA is not a uniform condition and ACA differs significantly from VFCA with regard to pathophysiologic mechanisms, neuropathologic damage, post-resuscitation organ dysfunction, and response to therapy, the treatment of CA survivors may need to be tailored to the etiology [12, 13]. However, whether the quantitative characteristics of EEG, as potential indicators of brain injury and neurological prognosis, are influenced by CA causes is unknown. In this study, we compared characteristics of early post-resuscitation EEG activity between ACA and VFCA and investigated the relationships between quantitative EEG features and post-resuscitation brain injury and neurological outcomes in established CA models of rats.
Materials and Methods
Animal Preparation
This study was approved by the ethics of animal investigation committee of Third Military Medical University. The study was conducted in strict accordance with the National Guide for the Care and Use of Laboratory Animals.
Thirty-two adult Sprague–Dawley rats (10–12 weeks) of both sexes (16 males and 16 females) weighing 184–337 g provided by laboratorial animal center of Third Military Medical University were fasted overnight, except for free access to water. Anesthesia was initiated by intramuscular injection of pentobarbital sodium (45 mg/kg). Additional doses of 10 mg/kg were administered if signs of pain and stress occurred. The trachea was orally intubated with a 14-gauge cannula (Abbocath-T, Abbott Laboratories, North Chicago, IL, USA) for mechanical ventilation by a volume-controlled ventilator (ALC-V9, Alcott Biotech CO. Ltd, Shanghai, China) with a tidal volume of 6.5 mL/kg at a FiO2 of 0.21. For measurement of arterial pressure, a polyethylene tubing PE50 (Instech Laboratories Inc., Plymouth Meeting, PA, USA) was advanced from the right femoral artery into the thoracic/descending aorta. The left femoral vein was also cannulated with an additional PE-50 catheter to allow for administration of fluids and drugs. To monitor the core temperature, a thermocouple sensor (TH-212, Bjhocy science and technology Co. Ltd., Beijing, China) was orally inserted into esophagus. Core temperature was maintained between 36.5 and 37.5 °C until the end of the experiment. To record the EEG signals, four subdermal needles were inserted into the left and right surface of the skull (Fig. 1). All of the catheters were flushed intermittently with saline containing 2.5 IU/mL of crystalline bovine heparin to prevent clotting.
Induction of CA
After collection of baseline data, the thermocouple sensor was removed, and rats were randomized into ACA and VFCA groups. In the ACA group, asphyxia was induced by endotracheal tube clamping. CA was defined as a mean arterial pressure (MAP) less than 20 mmHg, occurring approximately 3 min after asphyxia. In the VFCA group, VF was induced through high frequency transesophageal cardiac pacing with an alternating current of 3–5 mA for 2 min and was verified by the presence of VF in ECG and an abrupt decrease in MAP. In the setting of VF, a MAP less than 20 mmHg was also defined as the beginning of CA. Mechanical ventilation was ceased at the onset of asphyxia or cardiac pacing.
Method of CPR
After 5 min of untreated CA, CPR, including chest compression and ventilation, was begun. Mechanical chest compression was delivered by a pneumatically driven compressor at a compression rate of 200/min with a depth of 25–30% of the anterior posterior diameter of the animal’s chest. Coincident with the start of chest compression, animals were mechanically ventilated at a frequency of 80/min with a tidal volume of 6.5 mL/kg at a FiO2 of 1.0. A dose of epinephrine (0.02 mg/kg) was injected 1 min after the start of CPR. After 2 min of CPR, a defibrillation was attempted with a single 2-J rectilinear biphasic shock (M-Series, Zoll Medical corporation, Chelmsford, MA, USA) if the cardiac rhythm was VF. An organized cardiac rhythm with MAP at or greater than 60 mmHg for an interval exceeding 5 min was defined as ROSC. If ROSC could not be achieved, CPR was continued for another 1 min and followed by another 2-J shock unless the animal was either successfully resuscitated or pronounced dead after a total of 10 min CPR.
The animals received intensive care for additional 4 h under normothermia (36.7–37.3 °C) after ROSC. For all animals, mechanical ventilation was continued with 100% oxygen for 1 h and then with room air for another 3 h. All catheters, including endotracheal tube, were removed, and wounds were surgically sutured 4 h after resuscitation. Animals were then returned to their cages with a room temperature maintained at 20–24 °C and observed for 96 h.
Measurements
Aortic pressure and lead II electrocardiogram (ECG) were continuously monitored during the experiment with a multiparameter patient monitor (Model 90369, Spacelabs, Snoqualmie, WA, USA). A two-channel EEG differential preamplifier (PRE-ISO.EEG100, Xiangyun Computing Technology, Beijing, China) was used for signal amplification and condition. The amplifier gain of each channel was set at 10,000, and the cutoff frequencies were set at 0.3 and 70 Hz for the high-pass and low-pass filters, respectively. EEG, ECG and arterial pressure were synchronously recorded through a data acquisition system supported by Windaq hardware/software (Dataq Instruments Inc., Akron, OH, USA) at a sample rate of 1000 Hz respectively.
Cardiac function was noninvasively measured at baseline and at hourly intervals after resuscitation with an echocardiograph system (DC-6, Mindray Medical International Limited, Shenzhen, China). Left ventricular ejection fraction (LVEF) and cardiac output index (COI) served as quantitative measurements of myocardial contractile function.
Arterial blood samples were drawn at baseline, 2 and 4 h after ROSC. Blood gases were measured with the aid of a blood analyzer (i15, Edan Instruments Inc, Shenzhen, China). Serum concentration of S100B and cardiac troponin T (cTnT) that were quantified with an enzyme-linked immunoassay (Elisa Kit, Cusbio Biotech Co. Ltd, Wuhan, China) according to the manufacturer’s instructions served as biomarkers of cerebral and cardiac injury.
We adopted neurological deficit score (NDS) that was developed to evaluate neurological outcome after global cerebral ischemia for rats based on a series of behavioral tests [14]. NDS was examined every 24 h and confirmed by two investigators blinded to the treatment.
After 96-h NDS evaluation, survived animals were euthanized with pentobarbital sodium. The brains were removed and immersed in paraformaldehyde. Paraffin-embedded brains were sliced in 10 µm sections and then stained with hematoxylin and eosin. Each section was visually assessed according to histopathologic damage score (HDS) in the CA1 region of hippocampus under microscopic fields at 400× magnifications [15].
Quantitative EEG Analysis
EEG analysis was performed off-line using MATLAB 7.0 (The MathWorks, Inc., Natick, MA, USA) after the experiment was finished. The EEG pattern was annotated and classified as one of the three following categories during the 4-h recording period: isoelectric/suppression, burst suppression, and continuous background EEG activity [16, 17]. Isoelectric/suppression was defined as there is not any visible EEG activity during a 30-s recording episode. Burst suppression was defined by the presence of clear increases in amplitude (burst, amplitude >10 µV in both left and right channels) followed by interburst intervals of at least 0.5 s without EEG activity or low amplitude activity (suppression, <10 µV). Characteristics of earlier post-resuscitation EEG, including the onset time of identifiable burst, TTNT, BSR, and information quantity (IQ), were quantitatively analyzed [18].
Statistical Analysis
Statistical analysis was performed with SPSS 19.0 software (SPSS, Chicago, IL, USA). Continuous data were presented as mean ± SD. For baseline and experimental measurements between groups, two-tailed Student’s t test was used. Quantitative EEG characteristics were analyzed by two-way analysis of variance (ANOVA) for post hoc comparison between groups. Survival curves were obtained with a Kaplan–Meier analysis and compared between groups with a log-rank test. The relationships between characteristics of EEG and neurological outcome and survival were analyzed using Pearson’s correlation and single-variable logistic regression. A p < 0.05 was considered statistically significant.
Results
Baseline and Resuscitation Data
There were no differences in body weight and baseline measurements of heart rate, core temperature, and MAP between ACA and VFCA groups (Table 1; Fig. 2). CA was induced 179.8 ± 28.1 s after asphyxia in the ACA group and immediately induced after transesophageal cardiac pacing in the VFCA group (Fig. 3). VF was occurred for one animal in ACA after 5 s of CPR and was defibrillated with a 2-J shock 2 min later. The duration of CPR, number of shocks, and total dosage of epinephrine were significantly higher in VFCA group (Table 1).
Hemodynamic and cardiac function measurement at baseline and throughout post-resuscitation recording period. a heart rate, b mean arterial pressure, c left ventricular ejection fraction and d cardiac output index. ACA Asphyxial cardiac arrest, BL baseline, bpm beat per minute, PR post-resuscitation, VFCA ventricular fibrillation cardiac arrest. *p < 0.05 and **p < 0.01 compared with ACA group
Hemodynamic and Cardiac Function
As shown in Fig. 2 and Table 2, no statistical differences were observed in MAP, LVEF, and arterial blood gases between ACA and VFCA groups. However, heart rate and COI were significantly lower in ACA group during the 4-h post-resuscitation period.
Post-resuscitation Brain and Cardiac Injury
Serum levels of S-100B (Fig. 4a) measured at 120 (127.4 ± 34.4 vs. 76.3 ± 47.4 pg/mL, p = 0.002) and 240 min (270.2 ± 69.7 vs. 72.4 ± 44.1 pg/mL, p < 0.001) post-resuscitation were significantly higher for animals subjected to ACA. At the same time, serum levels of cTnT (Fig. 4b) were statistically lower compared with VFCA (PR120: 205.0 ± 66.1 vs. 285.6 ± 127.1 pg/mL, p = 0.040; PR240: 129.1 ± 41.4 vs. 323.1 ± 160 pg/mL, p = 0.005).
Microscopic examination revealed that nuclear pyknosis, karyorrhexis, and vacuolization occurred in the CA1 region in both groups (Fig. 5). However, both percentage of dystrophic neurons (60.2 ± 12.8 vs. 28.7 ± 7.6%, p = 0.002) and HDS (2.75 ± 0.61 vs. 1.75 ± 0.50, p = 0.03) were significantly higher in ACA group.
Representative histological images of the hippocampus CA1 regions in ACA (a) and VFCA (b) groups at 96 h after resuscitation. All images were captured at ×400 magnification. ACA Asphyxial cardiac arrest, VFCA ventricular fibrillation cardiac arrest. N (white arrow), P (black arrow), K (green arrow), and V (yellow arrow) indicate normal, pyknosis, karyorrhexis, and vacuolization pyramidal cells (Color figure online)
Neurological Outcomes and Survival
The NDS measurements during the 96-h observational period are listed in Table 3. Animals in the ACA group had significantly higher NDS compared with animals in the VFCA group at each assessment time points. Four rats (1 male and 3 females) in ACA and fourteen rats (7 males and 7 females) in VFCA survived to 96 h. The average survival time (53.6 ± 31.6 vs. 89.0 ± 19.1 h, p < 0.001) and cumulative survival rate were significantly lower for ACA (Fig. 6).
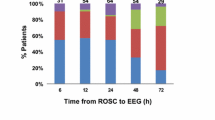
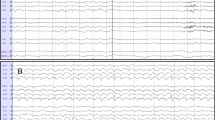
Difference in Quantitative Characteristics of EEG
EEG waveform showed a flat trace after CA was successfully induced. As shown in Fig. 7, all animals showed the same EEG recovery pattern in the order of isoelectric tracing, burst suppression, and continuous background EEG activity except two rats still in the phase of burst suppression in ACA group 4 h after resuscitation. The onset time of EEG burst (22.5 ± 4.1 vs. 16.0 ± 2.5 min, p < 0.001) and TTNT (204.5 ± 38.5 vs. 156.7 ± 23.4 min, p < 0.001) were significantly longer in the ACA group compared to VFCA. Figure 8 illustrates the trend of BSR and IQ during the 4-h post-resuscitation period between ACA and VFCA. Thirty minutes after ROSC, both BSR and IQ were significantly lower in the ACA group. The difference of IQ persisted during the 4-h post-resuscitation recording period while BSR values in the 2 groups converged after 3 h.
Relationships Between Characteristics of EEG and Neurological Outcomes
Pearson’s correlation showed that onset time of EEG bursting (r = 0.393, 95% CI 0.115–0.638, p = 0.026), TTNT (r = 0.399, 95% CI 0.068–0.623, p = 0.024), 3-hour IQ (r = −0.369, 95% CI −0.606 to −0.053, p = 0.038) and 4-h IQ (r = −0.469, 95% CI −0.688 to −0.192, p = 0.007) associated with 96-h NDS.
Single logistic regression analysis indicated that onset time of EEG bursting (p = 0.028, adjusted R 2 = 0.286, β = 0.291, 95% CI 0.093–1.243), TTNT (p = 0.013, adjusted R 2 = 0.321, β = 0.031, 95% CI 0.012–0.096), 3-h BSR (p = 0.033, adjusted R 2 = 0.180, β = 0.026, 95% CI 0.028–0.106), 3-h IQ (p = 0.030, adjusted R 2 = 0.265 β = −8.101, 95% CI −21.739 to −2.484) and 4-h IQ (p = 0.019, adjusted R 2 = 0.310, β = −9.232, 95% CI −25.746 to −3.226) were independent predictors of 96-h survival.
Discussion
The present study demonstrates that quantitative characteristics of early (first four hours) post-resuscitation EEG differ considerably between ACA and VFCA with equivalent CA time in rats. The prolonged isoelectric and burst suppression phases, depressed BSR and IQ values in ACA associated with severe brain injury, poor neurological outcome, and survival.
The unique vulnerability of the brain is attributed to its limited tolerance of ischemia and its unique response to reperfusion [19]. Brain injury alone contributes greatly to overall morbidity and mortality in the resuscitated CA patient [4]. Cerebral edema, ischemic degeneration, and impaired autoregulation characterize the brain injury pattern in a series of pathophysiological processes that have been termed the post-cardiac arrest syndrome [20].
Consistent with previous animal studies, ACA presented more severe brain injuries with worse neurological outcome and survival compared with VFCA in rats with identical 5-min CA duration in the current study [21]. Although the pathophysiology of post-resuscitation brain injury is not fully understood, earlier studies suggest that the mechanisms of brain damage are different from ACA and VFCA [12, 13]. In contrast to the sudden pulselessness and complete cessation of blood flow after the onset of lethal tachyarrhythmia VFCA, the development of ACA is gradual and is characterized by a pre-arrest period of tissue hypoxia and hypercapnia with incomplete ischemia for several minutes preceding the onset of pulselessness. The impaired cerebrovascular autoregulation that occurs during asphyxia contributes to the decreased cerebral blood flow that consecutively follows the changes in MAP prior to its cessation [12]. At the onset of VF, pulmonary veins, the left side of the heart and the entire arterial system are filled with oxygenated blood; thus, acceptable pO2/pCO2 levels can be maintained for several minutes after CA without CPR. On the contrary, ACA is characterized by severe hypoxia and acidosis, depleted pulmonary reservoir, and worse metabolic reserve prior to onset of CA [22]. During the complete ischemia, asphyxia further exacerbates brain acidosis, which results in irreversible neuronal injuries and brain damage [23]. Additionally, prolonged delivery of substrates during anaerobic metabolism to the brain along with platelets and coagulation factors may impair microcirculation and subsequently alter post-resuscitation cerebral reperfusion [12, 22, 24]. As a consequence, worse neurological outcome and survival were observed in the ACA group, even though the post-resuscitation myocardial injury was milder than that of VFCA [25].
The EEG is observed to become isoelectric within 10–40 s after respiratory or circulatory arrest in mammals [26]. Since EEG directly reflects the functioning of cortical synapses, the disappearance of synaptic activity is the earliest consequence of cerebral ischemia and failure of synaptic transmission has been proposed to account for electric silence in the EEG after CA [27]. The very rapid failure of the cortical synaptic activity during CA may result from a decline in adenosine triphosphate (ATP), which is a main factor causing hypoxic block of synaptic transmission [28]. The changes of synaptic function are, in principle, reversible if blood flow is restored in time. However, prolonged ischemia can lead to persistent synaptic failure because of insufficient oxygen and glucose supply [26].
In order to investigate the recovery of EEG, along with neurological outcome in humans immediately after resuscitation from CA, Jorgensen et al. [29] outlined the sequential recovery of EEG which resembled orderly post-ischemic recovery into 3 phases: an initial phase without detectable cortical activity (isoelectric EEG) associated with the presence of cranial nerve reflexes, followed by a transition phase of intermittent cortical activity (burst suppression) associated with posturing and stereotypic motor responses and lastly, a phase of continuous cortical activity accompanied by stereotypic reactivity and with consciousness returning subsequently.
In the current study, the EEG recovery patterns in rats were similar to those occurring in human [16, 29]. The isoelectric EEG that reflects massive cortical synaptic arrest in the earlier phase after ROSC does not necessarily preclude favorable functional recovery because EEG burst appeared in all of the animals within 34 min. When the EEG evolved to the transition phase of burst suppression and/or ultimate continuous pattern, the neurological recovery could be predictable [30]. However, compared with VFCA, the onset time of EEG burst, duration of burst suppression, BSR and IQ, were remarkably lower in the ACA group. The differences in characteristics of EEG can be explained by the difference in severity of post-resuscitation brain damage between ACA and VFCA. Zhang et al. [21] reported that ACA causes more severe cerebral metabolism injuries than VFCA with identical 8-min CA duration in pig models. Kass et al. [31] investigated the effects of anoxia on the recovery of neural transmission in the in vitro rat hippocampal slice and demonstrated that the fall in tissue ATP during anoxia is associated with the production of irreversible damage after reperfusion. The different forms of dysfunction of cortical synapses, which occur at different stages of post-resuscitation period, were directly reflected in the EEG waveforms [32]. This inference was confirmed by the accompanying brain injury markers of S100 and exemplified by the good outcome in the VFCA group.
Another observation of the current study was that earlier post-resuscitation quantitative measures of EEG are more sensitive to CA causes than the prognosis of outcomes. For example, significant differences in BSR and IQ were observed between groups 30 min after ROSC but the two measures predicted survival 3 h later. This might be explained by the fact that post-resuscitation neurological recovery is a dynamic process [32]. The severity of brain injury affects synaptic transmission, axonal conduction, and cellular action potential firing in a sequential manner and plays a critical role in determining characteristics of EEG. The prognosis, however, also depends on damage to other organs than the brain [33].
The current study has several limitations. First, the design of the current study is to assess the difference of characteristics of early post-resuscitation EEG between ACA and VFCA models. However, the duration of untreated CA is another important factor that affects brain injury and the post-resuscitation EEG. The effect of duration of CA on post-resuscitation EEG is not considered in this study. Second, this study did not induct therapeutic hypothermia, which provides the most persuasive benefits for both the brain and the heart and is recommended for post-resuscitation care since ACA and VFCA may respond differently to hypothermia, and differences of characteristics of early post-resuscitation EEG between respiratory and cardiac causes are need to be investigated under hypothermia. Third, the study was performed in healthy animals. The presence of an underlying respiratory or cardiac disease might affect ischemic reperfusion-induced brain injury and EEG. Finally, quantitative EEG parameters are also affected by other factors, such as duration of CA, anesthetic and analgesic agents. Additionally, lack of standardized EEG terminology and threshold for prognostication after CA also obstruct its translation into humans at this point. Therefore, these results should be more carefully interpreted when applied into clinical practice.
Conclusion
Characteristics of earlier post-resuscitation EEG differ considerably between ACA and VFCA with equivalent CA time in rats. Quantitative measures of EEG not only predicted neurological outcome and survival, but also have the potential to stratify CA with different causes.
References
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–87.
Ro YS, Shin SD, Song KJ, Park CB, Lee EJ, Ahn KO, et al. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low-and high-resuscitation case volume. Resuscitation. 2012;83:855–61.
Wallmuller C, Meron G, Kurkciyan I, Schober A, Stratil P, Sterz F. Causes of in-hospital cardiac arrest and influence on outcome. Resuscitation. 2012;83(10):1206–11.
Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30(11):2126–8.
Sakurai A, Kinoshita K, Komatsu T, Yamaguchi J, Sugita A, Ihara S. Comparison of outcomes between patients treated by therapeutic hypothermia for cardiac arrest due to cardiac or respiratory causes. Ther Hypothermia Temp Manag. 2016;6(3):130–4.
Popp E, Böttiger BW. Cerebral resuscitation: state of the art, experimental approaches and clinical perspectives. Neurol Clin. 2006;24(1):73–87.
Feng G, Jiang G, Li Z, Wang X. Prognostic value of electroencephalography (EEG) for brain injury after cardiopulmonary resuscitation. Neurol Sci. 2016;37(6):843–9.
Hofmeijer J, Beernink TM, Bosch FH, Beishuizen A, Tjepkema-Cloostermans MC, et al. Early EEG contributes to multimodal outcome prediction of postanoxic coma. Neurology. 2015;85(2):137–43.
Wennervirta JE, Ermes MJ, Tiainen SM, Salmi TK, Hynninen MS, Särkelä MO, et al. Hypothermia-treated cardiac arrest patients with good neurological outcome differ early in quantitative variables of EEG suppression and epileptiform activity. Crit Care Med. 2009;37(8):2427–35.
Noirhomme Q, Lehembre R, Lugo Zdel R, Lesenfants D, Luxen A, Laureys S, et al. Automated analysis of background EEG and reactivity during therapeutic hypothermia in comatose patients after cardiac arrest. Clin EEG Neurosci. 2014;45(1):6–13.
Oh SH, Park KN, Shon YM, Kim YM, Kim HJ, Youn CS, et al. Continuous amplitude-integrated electroencephalographic monitoring is a useful prognostic tool for hypothermia-treated cardiac arrest patients. Circulation. 2015;132(12):1094–103.
Varvarousis D, Varvarousi G, Iacovidou N, D’Aloja E, Gulati A, Xanthos T. The pathophysiologies of asphyxial vs dysrhythmic cardiac arrest: implications for resuscitation and post-event management. Am J Emerg Med. 2015;33(9):1297–304.
Vaagenes P, Safar P, Moossy J, Rao G, Diven W, Ravi C, et al. Asphyxiation versus ventricular fibrillation cardiac arrest in dogs. Differences in cerebral resuscitation effects—a preliminary study. Resuscitation. 1997;35(1):41–52.
Hendrickx HH, Safar P, Miller A. Asphyxia, cardiac arrest and resuscitation in rats. II. Long term behavioral changes. Resuscitation. 1984;12(2):117–28.
Neigh GN, Kofler J, Meyers JL, Bergdall V, La Perle KM, Traystman RJ, et al. Cardiac arrest/cardiopulmonary resuscitation increases anxiety-like behavior and decreases social interaction. J Cereb Blood Flow Metab. 2004;24(4):372–82.
Rundgren M, Rosén I, Friberg H. Amplitude-integrated EEG (aEEG) predicts outcome after cardiac arrest and induced hypothermia. Intensive Care Med. 2006;32:836–42.
Chen B, Song FQ, Sun LL, Lei LY, Gan WN, Chen MH, et al. Improved early postresuscitation EEG activity for animals treated with hypothermia predicted 96 h neurological outcome and survival in a rat model of cardiac arrest. Biomed Res Int. 2013;2013:312137.
Deng R, Koenig MA, Young LM, Jia X. Early quantitative gamma-band eeg marker is associated with outcomes after cardiac arrest and targeted temperature management. Neurocrit Care. 2015;23(2):262–73.
Stub D, Bernard S, Duffy SJ, Kaye DM. Post cardiac arrest syndrome: a review of therapeutic strategies. Circulation. 2011;123(13):1428–35.
Sundgreen C, Larsen FS, Herzog TM, Knudsen GM, Boesgaard S, Aldershvile J. Autoregulation of cerebral blood flow in patients resuscitated from cardiac arrest. Stroke. 2001;32(1):128–32.
Zhang Y, Li CS, Wu CJ, Yang J, Hang CC. Comparison of cerebral metabolism between pig ventricular fibrillation and asphyxial cardiac arrest models. Chin Med J. 2015;128(12):1643–8.
Boettiger BW, Krumnikl JJ, Gass P, Schmitz B, Motsch J, Martin E. The cerebral ‘no-reflow’ phenomenon after cardiac arrest in rats-influence of low-flow reperfusion. Resuscitation. 1997;34:79–87.
Kalimo H, Rehncrona S, Söderfeldt B, Olsson Y, Siesjö BK. Brain lactic acidosis and ischemic cell damage: 2. Histopathology. J Cereb Blood Flow Metab. 1981;1(3):313–27.
Hickey RW, Painter MJ. Brain injury from cardiac arrest in children. Neurol Clin. 2006;24:147–58.
Kamohara T, Weil MH, Tang W, Sun S, Yamaguchi H, Klouche K, et al. A comparison of myocardial function after primary cardiac and primary asphyxial cardiac arrest. Am J Respir Crit Care Med. 2001;164(7):1221–4.
Hofmeijer J, van Putten MJ. EEG in postanoxic coma: prognostic and diagnostic value. Clin Neurophysiol. 2016;127(4):2047–55.
Hofmeijer J, van Putten MJ. Ischemic cerebral damage: an appraisal of synaptic failure. Stroke. 2012;43(2):607–15.
Lipton P, Whittingham TS. Reduced ATP concentration as a basis for synaptic transmission failure during hypoxia in the in vitro guinea-pig hippocampus. J Physiol. 1982;325:51–65.
Jørgensen EO, Malchow-Møller A. Natural history of global and critical brain ischaemia. Part I: EEG and neurological signs during the first year after cardiopulmonary resuscitation in patients subsequently regaining consciousness. Resuscitation. 1981;9(2):133–53.
Geocadin RG, Sherman DL, Christian Hansen H, Kimura T, Niedermeyer E, Thakor NV, et al. Neurological recovery by EEG bursting after resuscitation from cardiac arrest in rats. Resuscitation. 2002;55(2):193–200.
Kass IS, Lipton P. Mechanisms involved in irreversible anoxic damage to the in vitro rat hippocampal slice. J Physiol. 1982;332:459–72.
Thömke F, Brand A, Weilemann SL. The temporal dynamics of postanoxic burst-suppression EEG. J Clin Neurophysiol. 2002;19(1):24–31.
Tjepkema-Cloostermans MC, Hofmeijer J, Trof RJ, Blans MJ, Beishuizen A, van Putten MJ. Electroencephalogram predicts outcome in patients with postanoxic coma during mild therapeutic hypothermia. Crit Care Med. 2015;43(1):159–67.
Acknowledgements
This study was supported, in part by the National Nature Science Foundation of China (NSFC81271656), and a Foundation for the Author of National Excellent Doctoral Dissertation of China (FANEDD201060).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Rights and permissions
About this article
Cite this article
Chen, B., Chen, G., Dai, C. et al. Comparison of Quantitative Characteristics of Early Post-resuscitation EEG Between Asphyxial and Ventricular Fibrillation Cardiac Arrest in Rats. Neurocrit Care 28, 247–256 (2018). https://doi.org/10.1007/s12028-017-0401-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0401-z