Abstract
Background
Existing scoring systems for aneurysmal subarachnoid hemorrhage (SAH) patients fail to accurately predict patient outcome. Our goal was to prospectively study the Full Outline of UnResponsiveness (FOUR) score as applied to newly admitted aneurysmal SAH patients.
Methods
All adult patients presenting to Health Sciences Center in Winnipeg from January 2013 to July 2015 (2.5 year period) with aneurysmal SAH were prospectively enrolled in this study. All patients were followed up to 6 months. FOUR score was calculated upon admission, with repeat calculation at 7 and 14 days. The primary outcomes were: mortality, as well as dichotomized 1- and 6-month Glasgow Outcome Scale (GOS) and modified Rankin Scale (mRS) values.
Results
Sixty-four patients were included, with a mean age of 54.2 years (range 26–85 years). The mean FOUR score upon admission pre- and post-external ventricular drain (EVD) was 10.3 (range 0–16) and 11.1 (range 3–16), respectively. There was a statistically significant association between pre-EVD FOUR score (total, eye, respiratory and motor sub-scores) with mortality, 1-month GOS, and 6-month GOS/mRS (p < 0.05 in all). The day 7 total, eye, respiratory, and motor FOUR scores were associated with mortality, 1-month GOS/mRS, and 6-month GOS/mRS (p < 0.05 in all). The day 14 total, eye, respiratory, and motor FOUR scores were associated with 6-month GOS (p < 0.05 in all). The day 7 cumulative FOUR score was associated with the development of clinical vasospasm (p < 0.05).
Conclusions
The FOUR score at admission and day 7 post-SAH is associated with mortality, 1-month GOS/mRS, and 6-month GOS/mRS. The FOUR score at day 14 post-SAH is associated with 6-month GOS. The brainstem sub-score was not associated with 1- or 6-month primary outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Outcome prediction in aneurysmal subarachnoid hemorrhage (SAH) has been attempted utilizing a variety of scoring systems. One-month mortality rate for aneurysmal SAH is around 40%, with the 6-month rates approaching 50–60%. The intention through past attempts was to reliably predict, by way of clinical status and neuroimaging, the risk of developing the serious complications and adverse outcomes associated with SAH. Complications such as vasospasm, shunt-dependent hydrocephalus, subendocardial ischemia, and neurogenic pulmonary edema are of primary interest. In addition, length of intensive care unit (ICU) stay, ventilator dependency, tracheostomy and gastrostomy status, discharge rates, and 1- and 6-month outcome prediction are desired.
Commonly used clinical assessment scores include the World Federation of Neurological Surgeons (WFNS) [1], based on Glasgow Coma Scale (GCS), and the classical Hunt and Hess (H + H) [2] score based on general level of consciousness and the presence of focal deficits. These scores have demonstrated some usefulness in predicting the risk of post-aneurysmal SAH vasospasm rates and outcome. However, reliability has been drawn into question [3], and prediction value has fallen short of what is desired.
Furthermore, these current clinical assessment scores fail to reliably differentiate outcome among those patients with severe deficits. In particular, those patients that are intubated are notoriously difficult to assess on presentation to tertiary care neurosurgical services due to difficulties with communication and the pitfalls in the GCS score when endotracheal tubes are in place. One of the most important clinical factors in this category of patients is brainstem reflexes on neurological examination, which is documented but not included objectively in those scores currently used for aneurysmal SAH.
The Full Outline of UnResponsiveness (FOUR) score [4] has been validated in recent literature as equivalent to GCS in outcome prediction of post-traumatic brain injury [5]. In addition, recent analysis within the critical care literature has demonstrated good inter-rater agreement across multiple institutions [6]. More recently, a study comparing the FOUR score and GCS displayed superiority of the FOUR score to predict in-hospital mortality in severe traumatic brain injury (TBI) patients [7, 8]. The benefit that the FOUR score has over preexisting systems is the inclusion of specific categories for eyelid movement, motor examination, brainstem reflexes, and respiratory pattern.
Thus, the FOUR score does provide a structured objective scoring for aspects of brainstem function that can be assessed in all patients, especially those unable to verbally communicate. In addition to recent validation in the TBI population, the FOUR score has been shown to predict poor outcome and in-hospital mortality in general neurosurgical patients [8] and predict outcome in ICU settings [9]. Based on this, one could expect that this scoring system when applied to aneurysmal SAH will provide predictive value for post-SAH 1- and 6-month mortality rates, in addition to complications and patient functional outcomes. To date, there have been no studies assessing the use of the FOUR score in outcome prediction in a purely aneurysmal SAH population. Chen et al. has described the application of the FOUR score for SAH patients previously; however, this was conducted as the assessment of the FOUR score in an amalgamated, heterogeneous, neurosurgical population [10].
Our objective was to prospectively study the use of the FOUR score as applied to newly admitted aneurysmal SAH patients and determine its predictive value for a primary outcome of post-SAH 1- and 6-month mortality and morbidity. In addition, the FOUR score’s ability to predict post-SAH complications will be assessed in secondary analysis. To the author’s knowledge, this is the only such study in the literature to date.
Methods
Study Design
This study was a prospective observational study with patient recruitment over a 2.5-year period from January 2013 to July 2015. Local institutional research ethics board (REB) approval was obtained prior to initiation of this study. Any need for individual patient consent was waived by the REB panel.
Patient Population
All patients presenting to Health Sciences Center in Winnipeg during the above time period were included in this study. Any patient suffering complications related to the aneurysm treatment modality (i.e., clipping versus coiling) were removed from the study, so as to avoid confounding of outcome analysis secondary to surgical complications. However, during the above recruitment period there were no such treatment complications suffered by the study population. Thus, no patients were removed from the study or final analysis.
Primary Study Outcome
One- and 6-month mortality and functional outcomes as assessed by the modified Rankin Score (mRS) and Glasgow Outcome Scale (GOS).
The mRS system employed ranged from 0 to 6, with 0 representing complete recovery back to baseline, 1 representing no significant disability despite mild symptoms, 2 representing mild disability, 3 representing moderate disability requiring some assistance, 4 representing moderate-severe disability requiring significant assistance ambulating and with activities of daily living, 5 representing severe disability leaving the individual bed bound and completely dependent, and 6 representing death. For the purpose of analysis, we dichotomized the mRS scores into: Good Outcome = 0, 1, 2, or 3; and Poor Outcome = 4, 5, or 6.
The GOS system employed ranged from 1 to 5, with 5 representing complete recovery back to baseline, 4 representing mild deficits, 3 representing moderate deficits, 2 representing severe deficits, and 1 representing death. For the purpose of analysis, we dichotomized the GOS scores into: Good Outcome = 4 or 5 and Poor Outcome = 3 or less.
These specific dichotomizations were selected given that they have been readily described in the literature in various neurological outcome studies, including FOUR score in TBI [10, 11].
Secondary Study Outcomes
Vasospasm rate (radiographic and clinical), shunt-dependent hydrocephalus, subendocardial ischemia, neurogenic pulmonary edema, length of ICU stay, duration of mechanical ventilation, tracheostomy status, gastrostomy status, length of hospital stay, survival to discharge, and rehabilitation candidacy were recorded.
FOUR Score Calculation
Admission FOUR score was calculated by the assessing physician assistant, resident or attending from the neurosurgery service within 48 h of aneurysmal SAH onset. Only 3 individuals were responsible for the acquisition of the FOUR score. If delayed presentation to hospital occurred, the FOUR score was then calculated upon admission. Repeat calculation occurred at 7 and 14 days post-hemorrhage.
The reason behind the long recruitment window of 48 h is secondary to the geographic limitations of the region which our neurosurgical center covers. We cover a vast territory within Canada, and transport times lead to delayed presentations to the only neurosurgical service within the city of Winnipeg. Thus, setting a 48-h window allowed us to capture as many people within a “reasonable” timetable for patient transport to our location.
The FOUR score is graded as follows: The eye response (E) is graded as: E4 = eyelids open or opened, tracking or blinking to command, E3 = eyelids open but not tracking, E2 = eyelids closed but open to loud voice, E1 = eyelids closed but open to pain, and E0 = eyelids remain closed to pain. The motor response (M) is graded as: M4 = thumbs-up, fist or peace sign, M3 = localizing to pain, M2 = flexion response to pain, M1 = extension to pain, and M0 = no response to pain. The brainstem reflexes (B) are graded as: B4 = pupil and corneal reflexes present, B3 = one pupil wide and fixed, B2 = pupil or corneal reflexes absent, B1 = pupil and corneal reflexes absent, and B0 = pupil, corneal and cough reflex absent. Finally, the respiration pattern (R) is graded as: R4 = not intubated, regular breathing pattern, R3 = not intubated, Cheyne–Stokes breathing, R2 = no intubated, irregular breathing, R1 = breathes above ventilator rate, and R0 = breathes at ventilator rate or apnea.
Data Acquisition
All data were collected prospectively during their hospital stay, with a focus on: vasospasm rate, shunt-dependent hydrocephalus, subendocardial ischemia, neurogenic pulmonary edema, length of ICU stay, duration of mechanical ventilation, tracheostomy status, gastrostomy status, length of hospital stay, survival to discharge, rehabilitation candidacy, mortality rate at 1 and 6 months, and 6-month GOS and mRS.
Clinical vasospasm was determined by a change in neurological examination which coincided with computed tomography (CT) angiographic or formal catheter angiographic presence of cerebral vasospasm. The diagnosis of subendocardial ischemia was made via serum troponin elevations seen persistently for 72 h post-SAH, with evidence of some degree of dysfunction on bedside echocardiography. The diagnosis of neurogenic pulmonary edema was made via clinical examination with radiographic evidence of bilateral patchy infiltrates in the absence of cardiac, renal, and hepatologic dysfunction.
All data were recorded on a standard form (Appendix A of supplementary materials) included in the patients chart during their hospital stay, with a copy sent to their outpatient neurosurgery chart upon discharge to ensure transcription of follow-up data onto their data sheet. Functional assessments were conducted in clinic by physician assistant at the 1- and 6-month intervals.
Statistical Analysis
All statistical analysis was conducted via: SPSS statistical software (IBM Corp. Released 2013, IBM SPSS Statistics for Windows, version 22.0, Armonk, NY: IBM Corp.), XLSTAT (Addinsoft, New York, USA https://www.xlstat.com/en/) add-on package to Microsoft Excel (Microsoft Office 15, version 16.0.7369.1323) and R statistical software ((R Core Team (2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
For all analysis, alpha was set at 0.05. Comparison of demographic factors between various subgroups of patients (i.e., “good” vs. “poor” outcome, and “alive” vs. “dead”) was conducted using: two tailed t test, Mann-Whitney U test, and Chi-squared analysis depending on the parametric/nonparametric nature of continuous variables and the presence of categorical variables, respectively.
Cumulative FOUR score and FOUR sub-scores were compared with mortality, 1-month GOS/mRS, and 6-month GOS/mRS. The FOUR score values upon admission, day 7 and day 14 post-SAH were assessed with relation to the primary outcomes. The pre-external ventricular drain (EVD) FOUR score was utilized for the admission FOUR score values, since 26 patients did not receive an EVD upon admission, and those whom did receive an EVD had no significant difference in pre- versus post-EVD FOUR score values.
Analysis of the relation between FOUR score and the primary outcome of interest (i.e., patient outcome as per GOS/mRS) was conducted utilizing the dichotomized outcome scores (dichotomization described above). We employed a binary logistic regression analysis, in order to determine the association between sequential increases in FOUR score values (both total and sub-scores) and patient outcomes. All analysis between FOUR score (cumulative and sub-score values) and patient outcomes (dichotomized GOS/mRS) were done controlling for age.
Post-SAH complications and other secondary outcome measures were assessed in a secondary analysis to prove predictive value in these areas. This was conducted via univariate logistic regression, followed by a multivariate logistic regression for those variables which reached significance via univariate analysis. Receiver operating curves were generated for each admission scoring system (GCS, WFNS, H + H, Fisher CT, and FOUR) in prediction of 1-month mortality, 6-month mortality, 1-month dichotomized GOS, and dichotomized 6-month GOS.
Results
General
There were 64 patients included in the study with a mean age of 54.2 years (range 26–85 years). There were 49 females and 15 males. The mean time from bleed until neurosurgery assessment was 35.6 h (range 2–264 h). The mean admission GCS, WFNS grade, and H + H grade were 12 (range 3–15), 2.5 (range 1–5), and 2.4 (range 1–5), respectively. The mean Fischer CT grade was 3.4. Forty-one patients (64.1%) underwent microsurgical clipping of their aneurysm, with the remaining undergoing endovascular coiling.
The mean FOUR score upon admission pre- and post-EVD (if needed) was 10.3 (range 0–16) and 11.1 (range 3–16), respectively. Twenty-six patients did not receive an EVD. The remaining 38 whom received an EVD had no substantial difference in their FOUR score total, or sub-scores, comparing pre- to post-EVD. Hence, for the purpose of the statistical analysis, the pre-EVD score was utilized. The mean post-bleed day 7 and 14 FOUR scores were 14.5 (range 4–16) and 15.4 (range 6–16), respectively. No patients were lost to follow up.
A summary of the patient demographics is given in Table 1. Table 2 displays demographic comparison between patients with “good” versus “poor” dichotomized GOS at 1 and 6 months, and “alive” versus “dead” status at both 1 and 6 months (p values <0.05 were considered significant). Of note, there was no difference in age, sex or mean time to presentation to hospital between those with “good” versus “poor” outcome, and those with “alive” versus “dead’ status at both 1 and 6 months post-bleed. Details surrounding the aneurysm characteristics are shown in Appendix B of supplementary materials.
Primary Outcome
Overall 10 patients (15.6%) died in hospital. The mean GOS and mRS values at 1 month were 3.8 (range 1–5) and 2.6 (range 0–6), respectively. The mean GOS and mRS at 6 months were 4.0 (range 1–5) and 2.0 (range 0–6), respectively. Bar diagrams depicting 1- and 6-month GOS and mRS outcomes for the patients in this study are shown in Appendix C of supplementary materials. Upon comparing the aneurysm treatment modality (i.e., clip versus coiling) with patient outcomes, there was no statistically significant difference in: 1-month mortality (p = 0.205), 6-month mortality (p = 0.115), 1-month dichotomized GOS (p = 0.655), 1-month dichotomized mRS (p = 0.935), 6-month dichotomized GOS (p = 0.118), and 6-month dichotomized mRS (p = 0.650) between treatment modalities.
There was a statistically significant correlation between admission GCS with mortality and 1- and 6-month mRS and GOS values (p < 0.05 in all). There was a statically significant correlation between the admission H + H grade with mortality and 1- and 6-month mRS and GOS values (p < 0.05 in all). There was a statistically significant correlation between the admission WFNS score with mortality and 1- and 6-month mRS and GOS values (p < 0.05 in all). The admission Fisher CT score was not associated with mortality and 1- and 6-month mRS/GOS values.
There was a statistically significant association between pre-EVD FOUR score (total and E/R/M sub-scores) with mortality and 1-month GOS/mRS and 6-month GOS/mRS (p < 0.05 in all). The pre-EVD brainstem sub-score was only associated with overall mortality (p = 0.036), but not with 1- or 6-month GOS/mRS.
The day 7 FOUR score (total and E/R sub-scores) was associated with mortality, 1-month GOS and 6-month GOS/mRS (p < 0.05 in all). The brainstem sub-score at day 7 was not associated with any primary outcome. The motor sub-score at day 7 was only associated with overall mortality (p < 0.001) and 6-month GOS (p = 0.015). There was no statistically significant difference in day 7 FOUR score for those undergoing surgical clipping or endovascular coiling (p = 0.587).
The day 14 FOUR score was rarely found to be associated with any of the primary outcome measures. The total, eye, respiratory, and motor day 14 scores were only associated with 6-month GOS (p < 0.05 in all). The day 14 motor score was associated with overall mortality (p < 0.001). Table 3 displays the admission pre-EVD, day 7 and day 14 FOUR score categories and their association with mortality, 1-month GOS/mRS and 6-month GOS/mRS. There was no statistically significant difference in day 14 FOUR score for those undergoing surgical clipping or endovascular coiling (p = 0.474).
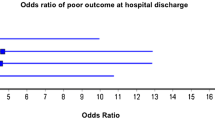
We also determined the ROCs for primary outcome prediction across all admission scoring systems (GCS, Fisher CT, WFNS, H + H, and FOUR), allowing comparison between the scoring systems. Table 4 displays a tabulated version of all area under the curve (AUC) for the ROCs of all scoring systems in the prediction of 1-month mortality, 6-month mortality, 1-month dichotomized GOS, and 6-month dichotomized GOS. Of note, admission FOUR score displays superior AUC in the prediction of 1-month (AUC = 0.762, p = 0.009) and 6-month mortality (AUC = 0.823, p = 0.004), when compared to all other scoring systems. Furthermore, the admission FOUR score displayed co-superiority in the prediction of 1-month (AUC = 0.810, p < 0.001) and 6-month (AUC = 0.832, p = 0.001) GOS with the admission H + H score (AUC = 0.831, p < 0.0001; AUC = 0.842, p < 0.001, respectively). Figure 1 displays all ROCs for the prediction of 6-month mortality. The ROCs for 1-month mortality, 1-month dichotomized GOS and 6-month dichotomized GOS are found in Appendix D of supplementary materials.
Binary logistic regression analysis—6-month mortality ROCs. AUC area under the curve, B brainstem, CT computed tomography, FOUR Full Outlined of UnResponsiveness, E eyes, GCS Glasgow Coma Scale, GOS Glasgow Outcome Score, H + H Hunt and Hess, M motor, Ma male, R respiratory, ROC receiver operating curve, T total, WFNS World Federation of Neurological Surgeons
Secondary Outcomes
The mean ventilator-dependent days, length of ICU stay, and hospital stay were 3.6 days (range 0–24 days), 5.8 days (range 0–40 days), and 30.7 days (range 3–290), respectively.
Clinical and radiographic vasospasm occurred in 29.7 and 62.5% of patients, respectively. Subendocardial ischemia and neurogenic pulmonary edema occurred in 9.4 and 20.3%, respectively. Tracheostomy and gastrostomy were required in 4.7 and 9.4%, respectively.
Only 48.4% of patients were able to be discharged to home directly from hospital. The remaining patients either spent a period of time in rehabilitation or were sent directly to long-term care facilities.
Through multivariate analysis, the following significant associations were discovered. There was a statistically significant correlation between the presence of subendocardial ischemia with mortality and 1- and 6-month GOS values (p < 0.05). In addition, the development of clinical vasospasm was statistically significantly correlated with 1- and 6-month GOS values (p < 0.05). Similarly, the development of neurogenic pulmonary edema was statistically significantly correlated with mortality (p < 0.05).
The total FOUR score (at 7 days post-hemorrhage) was found to be statistically significantly correlated with the development of clinical vasospasm (p < 0.05). The total FOUR score at admission (pre-EVD), at day 7 and day 14 post-bleed was not statistically associated with any other of the secondary outcomes included in this study. Appendix E of supplementary materials depicts the number of patients developing the secondary outcomes of interest.
Discussion
The FOUR score provides us with a clinical assessment tool and a potential means of subcategorizing these moderate to severe SAH patients in greater detail. Existing studies in TBI [4] and in the intensive care unit setting have displayed the utility of this scoring system. Inter-rater variability is low [6] with the FOUR score and in fact has been demonstrated to be less than GCS [11], with scoring of intensivists equivalent to neurologists. Patients considered to be in “vegetative states” as per GCS have been displayed to be minimally conscious according to FOUR calculation [12].
Despite the advantages of this relatively new coma scoring system, the FOUR score has yet to be commonly applied in the setting of aneurysmal SAH. Given easy use, its early success in the intensive care setting, and potential to further clinically subcategorize those patients with moderate and severe hemorrhage grade, our hope is that it will prove superior to existing grading and scoring systems in prediction of outcome. With improved prediction value, the FOUR score has the potential to replace existing aneurysmal subarachnoid hemorrhage grading schemes, simplifying the assessment of these patients and improving communication among healthcare professionals involved in the care of this patient population. As well, better prediction of adverse events and outcomes allows for enhanced communication with the patient and family in terms of in-hospital and suspected out-of-hospital clinical course.
Our study on the application of the FOUR score in the SAH population is, to the authors’ knowledge, the only study to do this in a purely SAH population. We have identified some interesting correlations between the FOUR score and our primary and secondary outcomes.
First, the FOUR score upon admission (pre-EVD) displayed a statistically significant relationship to mortality, 1-month GOS/mRS, and 6-month GOS/mRS. Further to this, the admission FOUR score displayed superior AUC (0.762, p = 0.009; 0.823, p = 0.004, respectively) in the prediction of 1- and 6-month mortality, compared to all other admission scoring systems (GCS, Fisher CT, WFNS, and H + H). The admission FOUR score also displayed co-superiority (with H + H) in the prediction of 1-month dichotomized GOS (AUC = 0.810, p < 0.001) and 6-month dichotomized GOS (AUC = 0.832, p = 0.001). The brainstem sub-score was the only admission FOUR sub-score not associated with 1- or 6-month primary outcomes. Thus, the admission FOUR score may prove to be superior, particularly in mortality prediction, compared to other standard clinical scoring systems in SAH.
Second, the cumulative FOUR score (in addition to the eyes and respiratory sub-scores) at day 7 post-hemorrhage correlated mortality, 1-month GOS, and 6-month GOS/mRS. The brainstem sub-score at day 7 failed to be associated with any primary outcome measure.
Third, the day 14 FOUR scores (total, eyes, respiratory, and motor) were only associated with 6-month GOS. The day 14 brainstem sub-score failed to be associated with any primary outcome.
Fourth, the brainstem sub-score at various time points (admission, days 7 and 14) was not found to be associated with the primary outcomes. Only the admission pre-EVD brainstem sub-score was found to be associated with overall mortality. This is contradictory to our initial thoughts regarding the benefit of this scoring tool. The brainstem score is not found in the GCS, WFNS or H + H scoring systems, and thus, it was our belief that this sub-score would be able to predict outcome in those with severe neurological impairment. Our study does not support this. We believe this is secondary to a mean admission WFNS and H + H scores of 2.5 and 2.4, respectively. Thus, with the majority of our patients in low to moderate grade for SAH severity, our numbers for those with heavy deficits and high-grade SAH are likely too small to determine the association between abnormal brainstem sub-score values and the various primary outcomes.
Finally, the cumulative FOUR score at day 7 post-hemorrhage was found to be statistically significantly linked to the development of clinical vasospasm. The association of the total FOUR score at day 7 with the development of clinical vasospasm needs to be viewed with caution. Only 19 patients developed clinical vasospasm; thus, despite a “statistically significant” association, this relationship requires further large confirmatory studies.
Limitations
Despite the interesting trends and associations identified, there are some significant limitations within our study which need to be highlighted.
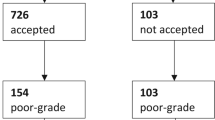
First, there were a small number of patients included in the study across the 2.5-year recruitment period. This likely stems from the fact that our center covers a significant territory, where a large portion of SAH patients typically present to their local community hospital setting. In the case of severe grade SAH, the decision to transfer the patient to our neurosurgical center is at the discretion of the attending neurosurgeon fielding the phone call from the local hospital. Thus, we are likely missing a large number of severe clinical grade SAH patients since it was elected to palliate them at their local facilities. Missing these patients potentially impacts our analysis of the FOUR scores ability to predict outcome.
Second, the average time until neurosurgical assessment was quite high in some cases. This stems from the geographic territory that our hospital services. Thus, suboptimal care for these SAH patients during this time delay may have led to the development of complications such as clinical vasospasm and clinical deterioration prior to neurosurgical assessment. This would also skew our results on the association of FOUR score and the primary outcomes. Furthermore, the admission FOUR score values could have varied between patients solely based on the time from hemorrhage to presentation, thus making the statistical associations between the admission FOUR score on the primary/secondary outcomes somewhat difficult to comment on.
Third, EVD placement varied significantly within our patient population. We found that there was not a significant difference between the FOUR score values when comparing pre- and post-EVD scores. However, the decision to place EVDs within our patients was made on an individual basis, based on: patient clinical presentation and radiographic appearance of hydrocephalus. Finally, the ultimate decision to place, and the timing of placement, of an EVD was made by the staff vascular neurosurgeon on call at the time. Given the potential for heterogeneity in EVD placement and variable time lag between pre- and post-EVD FOUR scores, it is possible that we are missing a significant difference between these two scores.
Fourth, the day 14 post-hemorrhage cumulative FOUR score (in addition to eye, respiratory, and motor sub-scores) was essentially only associated with 6-month GOS. It is not surprising that the 14-day FOUR score values were not associated with mortality in our group, since most of those whom died had already done so by day 14 given the complexity and severity of the ICU course. It is slightly surprising that the day 14 scores were not associated with 1-month GOS/mRS. This lack of association may by again due to lack of power. Finally, despite previous literature displaying acceptable inter-rater variability in the assignment of the FOUR score [6], there is still the potential that inter-rater variability impacted out FOUR score calculations. We utilized 3 individuals for the FOUR score assessment at the various time points. We did not undertake overlapping assessments of the FOUR scores; thus, we cannot make a comment on our individual institution’s inter-rater variability throughout this study.
Future Directions
We have displayed interesting results with the use of the FOUR score for outcome prediction in the SAH population. However, further prospective application of the FOUR score in the setting of aneurysmal SAH is required. We postulate that further study of this scoring system will demonstrate its ability to predict outcome in the high-grade SAH patients, superior to existing SAH clinical scoring systems. Future plans include multicenter application of this scoring system to SAH patients in order to achieve much high patient numbers, with the hopes of validating our results from this study. Furthermore, we plan to focus on the high clinical grade SAH patients in order to determine the FOUR score’s ability to predict both short- and long-term outcome.
Conclusions
The FOUR score at admission and day 7 post-SAH is associated with mortality, 1-month GOS/mRS and 6-month GOS/mRS. The FOUR score at day 14 post-SAH is associated with 6-month GOS. The brainstem sub-score was not associated with 1- or 6-month primary outcomes.
References
[Anonymous]. Report of world federation of neurological surgeons committee on a universal subarachnoid hemorrhage grading scale. J Neurosurg 1988; 68:985–986.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28:14–20.
Oshiro EM, Walter KA, Piantadosi S, Witham TF, Tamargo RJ. A new subarachnoid hemorrhage grading system based on the Glasgow coma scale: a comparison with the Hunt and Hess and world federation of neurological surgeons scales in a clinical series. Neurosurgery. 1997;41(1):140–8.
Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: the FOUR score. Ann Neurol. 2005;58(4):585–93.
Sadaka F, Patel D, Lakshmanan R. The FOUR score predicts outcome in patients after traumatic brain injury. Neurocrit Care. 2012;16:95–101.
Kramer AA, Wijdicks EF, Snavely VL, Dunivan JR, Naranjo LL, Bible S, et al. A multicenter prospective study of interobserver agreement using the Full Outline of Unresponsiveness score coma scale in the intensive care unit. Crit Care. 2012;40(9):2671–6.
Okasha AS, Fayed AM, Saleh AS. The FOUR score predicts mortality, endotracheal intubation and ICU length of stay after traumatic brain injury. Neurocrit Care. 2014;21(3):496–504.
Akavipat P, Sookplung P, Kaewsingha P, Maunsaiyat P. Prediction of discharge outcome with the full outline of unresponsiveness (FOUR) score in neurosurgical patients. Acta Med Okayam. 2011;65(3):205–10.
Bruno MA, Ledoux D, Lambermont B, et al. Comparison of the full outline in unresponsiveness and Glasgow Liege scale/Glasgow coma scale in an intensive care unit population. Neurocrit Care. 2011;15:447–53.
Chen B, Grothe C, Schaller K. Validation of a new neurological score (FOUR Score) in the assessment of neurosurgical patients with severely impaired consciousness. Acta Neurochir (Wein). 2013;155:2133–9.
Xiao G, Wei J, Yan W, Wang W, Lu Z. Improved outcomes form the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial. Crit Care. 2008;12(2):R61.
Fischer M, Ruegg S, Czaplinski A, et al. Inter-rater reliability of the Full Outline of Unresponsiveness score and the Glasgow Coma Scale in critical ill patients: a prospective observational study. Crit Care. 2010;14(2):R64.
Acknowledgments
This work was made possible through salary support through the Cambridge Commonwealth Trust Scholarship, the Royal College of Surgeons of Canada—Harry S. Morton Travelling Fellowship in Surgery, the University of Manitoba Clinician Investigator Program, R. Samuel McLaughlin Research and Education Award, the Manitoba Medical Service Foundation, and the University of Manitoba Faculty of Medicine Dean’s Fellowship Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAZ has received salary support for dedicated research time, during which this project was partially completed. Such salary support came from: the Cambridge Commonwealth Trust Scholarship, the Royal College of Surgeons of Canada—Harry S. Morton Travelling Fellowship in Surgery, the University of Manitoba Clinician Investigator Program, R. Samuel McLaughlin Research and Education Award, the Manitoba Medical Service Foundation, and the University of Manitoba - Faculty of Medicine Dean’s Fellowship Fund.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zeiler, F.A., Lo, B.W.Y., Akoth, E. et al. Predicting Outcome in Subarachnoid Hemorrhage (SAH) Utilizing the Full Outline of UnResponsiveness (FOUR) Score. Neurocrit Care 27, 381–391 (2017). https://doi.org/10.1007/s12028-017-0396-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0396-5