Abstract
Objective
Therapeutic hypothermia (TH) improves neurologic outcome in patients resuscitated from ventricular fibrillation. The purpose of this study was to evaluate TH effects on neurologic outcome in patients resuscitated from a non-shockable out-of-hospital cardiac arrest rhythm.
Design and Setting
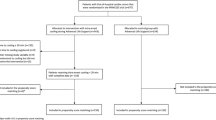
This is a retrospective cohort study of data reported to a registry in an emergency medical system in a large metropolitan region. Patients achieving field return of spontaneous circulation are transported to designated hospitals with TH protocols.
Patients
Patients with an initial non-shockable rhythm were identified. Patients were excluded if awake in the Emergency Department or if TH was withheld due to preexisting coma or death prior to initiation. The decision to initiate TH was determined by the treating physician.
Measurements
The primary outcome was survival with good neurologic outcome defined by a cerebral performance category of 1 or 2.
Main Results
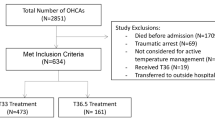
Of the 2772 patients treated for cardiac arrest during the study period, there were 1713 patients resuscitated from cardiac arrest with an initial non-shockable rhythm and 1432 patients met inclusion criteria. The median age was 69 years [IQR 59–82]; 802 (56 %) male. TH was induced in 596 (42 %) patients. Survival with good neurologic outcome was 14 % in the group receiving TH, compared with 5 % in those not treated with TH (risk difference = 8 %, 95 % CI 5–12 %). The adjusted OR for a CPC 1 or 2 with TH was 2.9 (95 % CI 1.9–4.4).
Conclusion
Analyzing the data collected from the registry of the standard practice in a large metropolitan region, TH is associated with improved neurologic outcome in patients resuscitated from initial non-shockable rhythms in a regionalized system for post-resuscitation care.

Similar content being viewed by others
References
Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63.
The Hypothermia After Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56.
Nolan JP, Morley PT, Vanden Hoek TL, et al. Therapeutic hypothermia after cardiac arrest: an advisory statement by the advanced life support task force of the International Liaison Committee on Resuscitation. Circulation. 2003;108:118–21.
Hachimi-Idrissi S, Corne L, Ebinger G, Michotte Y, Huyghens L. Mild hypothermia induced by a helmet device: a clinical feasibility study. Resuscitation. 2001;51:275–81.
Nielsen N, Hovdenes J, Nilsson F, et al. Outcome, timing and adverse events in therapeutic hypothermia after out-of-hospital cardiac arrest. Acta Anaesthesiol Scand. 2009;53:926–34.
Bernard SA, Jones BM, Horne MK. Clinical trial of induced hypothermia in comatose survivors of out-of-hospital cardiac arrest. Ann Emerg Med. 1997;30:146–53.
Busch M, Soreide E, Lossius HM, Lexow K, Dickstein K. Rapid implementation of therapeutic hypothermia in comatose out-of-hospital cardiac arrest survivors. Acta Anaesthesiol Scand. 2006;50:1277–83.
Storm C, Steffen I, Schefold JC, et al. Mild therapeutic hypothermia shortens intensive care unit stay of survivors after out-of-hospital cardiac arrest compared to historical controls. Crit Care. 2008;12:R78.
Don CW, Longstreth WT Jr, Maynard C, et al. Active surface cooling protocol to induce mild therapeutic hypothermia after out-of-hospital cardiac arrest: a retrospective before-and-after comparison in a single hospital. Crit Care Med. 2009;37:3062–9.
Oddo M, Schaller MD, Feihl F, Ribordy V, Liaudet L. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006;34:1865–73.
Vaahersalo J, Hiltunen P, Tiainen M, et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med. 2013;39:826–37.
Dumas F, Grimaldi D, Zuber B, et al. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients? Insights from a large registry. Circulation. 2011;123:877–86.
Bosson N, Kaji AH, Niemann JT, et al. Survival and neurologic outcome after out-of-hospital cardiac arrest: results one year after regionalization of post-cardiac arrest care in a large metropolitan area. Prehosp Emerg Care. 2014;18:217–23.
Newgard CD, Hedges JR, Arthur M, Mullins RJ. Advanced statistics: the propensity score–a method for estimating treatment effect in observational research. Acad Emerg Med. 2004;11:953–61.
Arrich J, Holzer M, Havel C, Mullner M, Herkner H. Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation. Cochrane Database Syst Rev. 2012;9:CD004128.
Kim YM, Yim HW, Jeong SH, Klem ML, Callaway CW. Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms? A systematic review and meta-analysis of randomized and non-randomized studies. Resuscitation. 2012;83:188–96.
Walters JH, Morley PT, Nolan JP. The role of hypothermia in post-cardiac arrest patients with return of spontaneous circulation: a systematic review. Resuscitation. 2011;82:508–16.
Lundbye JB, Rai M, Ramu B, et al. Therapeutic hypothermia is associated with improved neurologic outcome and survival in cardiac arrest survivors of non-shockable rhythms. Resuscitation. 2012;83:202–7.
Sunde K, Pytte M, Jacobsen D, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73:29–39.
Nielsen N, Friberg H, Gluud C, Herlitz J, Wetterslev J. Hypothermia after cardiac arrest should be further evaluated–a systematic review of randomised trials with meta-analysis and trial sequential analysis. Int J Cardiol. 2011;151:333–41.
Fisher GC. Hypothermia after cardiac arrest: feasible but is it therapeutic? Anaesthesia 2008;63:885–6; author reply 6.
Nielsen N, Wetterslev J, Cronberg T, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. 2013;369:2197–206.
Zeiner A, Holzer M, Sterz F, et al. Hyperthermia after cardiac arrest is associated with an unfavorable neurologic outcome. Arch Intern Med. 2001;161:2007–12.
Neumar RW, Nolan JP, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–83.
Testori C, Sterz F, Holzer M, Losert H, Arrich J, Herkner H, et al. The beneficial effect of mild therapeutic hypothermia depends on the time of complete circulatory standstill in patients with cardiac arrest. Resuscitation. 2012;83:596–601.
Isaacs E, Callaham ML. Ability of laypersons to estimate short time intervals in cardiac arrest. Ann Emerg Med. 2000;35:147–54.
Hallstrom AP. Should time from cardiac arrest until call to emergency medical services (EMS) be collected in EMS research? Crit Care Med. 2002;30:S127–30.
Sawyer KN, Kurz MC. Caution when defining prolonged downtime in out of hospital cardiac arrest as extracorporeal cardiopulmonary resuscitation becomes accessible and feasible. Resuscitation. 2014;85:979–80.
Acknowledgments
The authors would like to thank all the cardiac arrest center participants and the Los Angeles County EMS Agency staff, in particular Paula Rashi, Richard Tadeo, and Deidre Gorospe, who contributed to the ROSC registry and whose dedicated work provided the necessary data for this analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sung, G., Bosson, N., Kaji, A.H. et al. Therapeutic Hypothermia After Resuscitation From a Non-Shockable Rhythm Improves Outcomes in a Regionalized System of Cardiac Arrest Care. Neurocrit Care 24, 90–96 (2016). https://doi.org/10.1007/s12028-015-0184-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-015-0184-z