Abstract
Background
Global cerebral edema (GCE) with subsequent refractory intracranial hypertension complicates some cases of aneurysmal subarachnoid hemorrhage (aSAH), and typically is associated with poorer outcome. Treatment options for refractory intracranial pressure (ICP) cases are limited to decompressive hemicraniectomy (DHC) and targeted temperature management (TTM) with induced hypothermia (32–34 °C). No outcomes comparison between patients treated with either or both forms of refractory ICP therapy exists, and data on the effect of prolonged hypothermia on ICP and organ function among patients with aSAH are limited.
Methods
This is a retrospective study of aSAH patients who underwent DHC and/or prolonged hypothermia (greater than 48 h) for refractory ICP (i.e., ICP >20 mmHg after osmotherapy) in the intensive care unit of a single, tertiary-care academic center.
Results
Nineteen individuals with aSAH underwent TTM with or without DHC; sixteen patients underwent DHC alone. The patients in TTM group were younger (median age 44 years) than the DHC without TTM population (median age 60 years). TTM was started on median day 2 with a median duration of 7 days. There were no significant group differences in survival to discharge (59 % vs. 69 %) or in the mean modified Rankin score on follow-up (3.6 vs. 3.7), despite the TTM group having longer hospital length of stay (24 vs. 19 days, p = 0.03), longer duration of mechanical ventilation (20 vs. 9 days, p = 0.04), a higher cumulative fluid balance (12.8 vs. 5.1 L, p = 0.01), and higher APACHEII scores. The median maximal ICP decreased from 23.5 to 21 mmHg within 24 h of hypothermia initiation. There were no significant differences in other markers of end-organ function (respiratory, hematologic, renal, liver, and cardiac), infection rate, or adverse events between groups.
Conclusions
Use of prolonged TTM among aSAH patients with GCE and refractory ICP elevations is associated with a longer duration of mechanical ventilation but is not different in terms of neurological outcomes measured by modified Rankin score or organ function outcomes compared to patients who received DHC alone.
Similar content being viewed by others
Introduction
Global cerebral edema (GCE) following aneurysmal subarachnoid hemorrhage (aSAH) portends a poor outcome with a 30-day mortality ranging from 50 to 60 % [1, 2]. The development of GCE, heralded by intracranial hypertension, has been observed in as many as 57 % of all admitted cases [3] and is a major risk factor for cognitive dysfunction [4]. The cause of GCE remains largely unknown but may relate to transient intracranial circulation arrest at aneurysmal rupture with subsequent reflow phenomenon causing global brain edema.
Current strategies for management of intracranial hypertension include osmotherapy with mannitol, hypertonic saline, sedation, neuromuscular paralysis, and decompressive hemicraniectomy (DHC), which is generally employed as a last resort [5, 6]. However, therapeutic hypothermia has been shown to be neuroprotective following cardiac arrest and could possibly mitigate global cerebral edema by control of cerebral hypermetabolism [7] and fever [8]. Targeted temperature management (TTM) with induced hypothermia has also been utilized in patients with refractory elevations of intracranial pressure (ICP) due to aSAH [9, 10] or intraparenchymal hemorrhage [11, 12].
Nonetheless, given heterogeneity of trials examining the use of TTM in brain-injured patients and overall equivocal effect on outcomes, current guidelines do not recommend either for or against its use in patients who develop refractory elevations of ICP [13]. It is not clear whether TTM may reduce the need for DHC and whether one intervention or the other has a more favorable morbidity and mortality profile. Furthermore, because TTM is often considered as a short-term (12–48 h) intervention, the use of prolonged hypothermia (i.e., >48 h) and the adjunctive therapies it requires (e.g., paralysis and mechanical ventilation) rightfully raise questions about the risk–benefit ratio for such a therapy. Some specific concerns regarding prolonged hypothermia include pneumonia, arrhythmias, and coagulopathy [12, 14], in addition to the overall paucity of data on the effect of prolonged hypothermia among patients with refractory intracranial hypertension due to aSAH.
To further clarify the effects of prolonged TTM in patients with aSAH, we identified a cohort of patients who underwent extended hypothermia and compared outcomes of those who were treated with TTM to those who were not. We hypothesized that patients receiving prolonged hypothermia would have comparable outcomes to those having DHC alone, and as such it might be an effective therapeutic modality in patients developing aSAH-related GCE. In particular, we retrospectively reviewed the series of patients who were treated with prolonged hypothermia and/or DHC to explore the safety of TTM with particular attention to neurologic, pulmonary, renal, coagulation, and cardiac effects.
Methods
Study Population
We retrospectively reviewed consecutive aSAH cases admitted to the intensive care unit (ICU) of a single tertiary-care academic center from 2007 to 2012. We included all patients who had aSAH and either underwent DHC or prolonged hypothermia employed for greater than 48 h. Patients who had shorter duration of hypothermia were excluded. The study protocol was approved by the Mayo Clinic Institutional Review Board.
Standard Treatment
All patients received care for aSAH as per a predefined institutional protocol in accordance with current guidelines [15], including nimodipine, maintenance of euvolemia until vasospasm was detected, and normotension or permissive hypertension once the aneurysm was secured by coiling or aneurysm clipping. Transcranial Doppler ultrasound monitoring was performed daily to monitor for vasospasm, and when clinical suspicion existed by the neurosurgeon, computed tomography (CT) perfusion imaging with angiography was performed. Noncontrast CT and/or magnetic resonance imaging (MRI) was performed when clinically indicated to evaluate for ventricular catheter position, postoperatively, and to address clinical questions related to neurologic deficits or changes, and neurological prognosis consistent with current guidelines [15]. When vasospasm was identified clinically, fluids and vasopressors were administered to raise cerebral perfusion pressure (CPP) above 70 mmHg [16] with specific values individualized depending on the clinical situation. Patients had an indwelling external ventricular drain (EVD) placed as a standard of care for cerebrospinal fluid drainage for hydrocephalus (communicating or non-communicating), or concerns about elevated ICP or cerebral perfusion. The ICP, central venous pressure (when available), urine output, and the CPP were monitored continuously and recorded at hourly intervals in the electronic medical record.
Targeted Temperature Management
Patients received hypothermia in accordance with an institutionally defined TTM-management protocol to a target of 32–34 °C. To qualify, patients needed to have documentation of sustained ICP >20 mmHg despite sedation, analgesia, and osmotherapy (23.4 % hypertonic saline and/or mannitol). Patients were required to be intubated, mechanically ventilated, and receiving neuromuscular paralysis. Duration of hypothermia depended on daily reassessment of ICP and intracranial compliance. The need for DHC was discussed daily with attending neurosurgeon in multidisciplinary rounds. As a result, some patients underwent TTM following DHC and others underwent DHC following implementation of TTM.
All TTM patients were monitored per ICU protocol that included serial electrocardiography, blood gas analysis, assessments of renal function, coagulation profile, complete blood counts, surveillance cultures, and vital signs. Induction of hypothermia was achieved by rapid infusion of cold saline and further controlled by an external cooling device using two water-circulating blankets (Arctic Sun, Bard Medical, Medivance, Inc., Louisville, CO). The target core temperature of 32–34 °C (as measured by a bladder probe) was maintained until the clinician made a decision to initiate controlled rewarming per protocol (no more than 0.5 °C/h).
Decompressive Hemicraniectomy
DHC for intracranial hypertension was performed after weighing prognosis, operative risks, as well as neurologic status in multidisciplinary rounds. As previously noted, some patients underwent DHC with or without TTM for the management of intracranial hypertension. The non-TTM (DHC-only) group is comprised aSAH patients who underwent DHC only without any TTM during the hospital course versus the TTM group who may or may not also have required DHC.
Data Collection
All data were collected from the clinical records. Demographic and clinical information obtained at the time of admission were used to calculate Acute Physiology and Chronic Health Evaluation (APACHE) II score as a measure of overall disease severity and World Federation of Neurosurgeons (WFNS) grade as a measure of neurologic symptom severity.
Specific respiratory parameters obtained included blood gases, ventilator settings, and airway pressures at baseline then daily. The baseline assessments were immediately post-intubation; for those receiving TTM, we evaluated changes in respiratory parameters up to 10 days of hypothermia [17]. We assessed effect of hypothermia on indices of oxygenation and ventilation compared at the time of hypothermia initiation to the last day or day 10 of hypothermia whichever came first: PaO2/FiO2, positive end expiratory pressure (PEEP), pH, PaCO2, peak inspiratory pressure, tidal volume, and dynamic compliance (calculated as tidal volume/[peak inspiratory pressure—PEEP]). Using the PaO2/FiO2 as a measure of severity of hypoxia and the traditional cutoff of 300 extrapolated from acute respiratory distress syndrome (ARDS) literature [18], we evaluated both the raw and adjusted (proportion of the total mechanical ventilation (MV) days) number of days when the PaO2/FiO2 was below 300 in each group. To further examine TTM safety in patients who were already severely hypoxic prior to cooling (PaO2/FiO2 <300), we separately evaluated the effect of hypothermia on PaO2/FiO2 changes in those patients over time. Other parameters pertinent for pulmonary function, such as cumulative fluid status and units of transfused blood products, were also collected.
We have also explored ICP and CPP changes in the TTM group, documenting the highest ICP and the lowest CPP values for up to 3 days prior to hypothermia and up to 10 days of hypothermia [17].
To assess the effects of prolonged hypothermia on other organ systems, we documented the initial and the worst values for the hematologic, renal, and liver function parameters and compared these between the two groups. We reviewed charts for documentation of cardiac adverse events of TTM including bradycardia (heart rate <40) and QTc changes. To assess potential infectious adverse events, we documented new positive cultures for both groups.
Outcome Variables
Primary clinical outcome was survival to discharge. Secondary outcomes included post-discharge modified Rankin Score (mRS), ICU and hospital lengths of stay (LOS), and duration of MV.
Additional outcomes involved organ function parameters such as indices of oxygenation and ventilation during hypothermia, effect of TTM on ICP and CPP, and comparison of organ system data and documented adverse events between the groups.
Statistical Analyses
Groups were comprised on the basis of whether patients received TTM (TTM group) or not (comparison group who underwent DHC alone). Descriptive variables reported include medians with their interquartile ranges (IQR), or means with their standard deviations (±SD) where appropriate. Univariate analyses were performed to compare demographics, comorbidities, and in-hospital medications between the groups. The Chi-square test and the t test were used to evaluate for group differences in nominal and continuous variables, respectively. If parametric assumptions could not be met, then the Fisher’s Exact and/or Mann–Whitney tests were used. For matched or paired data (e.g., change in a parameter at day 10 compared to baseline for the individual subject), the changes or differences are expressed as their mean with 95 % confidence intervals (95 % CI).
A p value of less than 0.05 was considered statistically significant. All analyses were performed using JMP Pro 10.0.2 statistical software (SAS Institute Inc., Cary, NC).
Results
Patient Selection
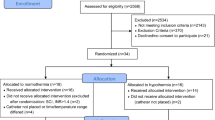
Twenty-five individuals with aSAH underwent TTM between March 2008 and December 2012. Six patients had hypothermia of less than 48 h duration and were excluded. Among the remaining 19 patients who comprised the prolonged TTM group, five did not require DHC. A total of 16 patients who underwent DHC alone without hypothermia were identified for the comparison group.
Group Characteristics
There were no baseline between-group differences in sex, body mass index (BMI), or WFNS scores on admission (Table 1). However, the patients in TTM group were younger and had higher APACHE II scores. All patients were modified Fisher SAH grade 3 or 4. There were no group differences in documented history of hypertension, renal disease, headaches/migraines, or daily alcohol use. Regarding other medical comorbidities, one patient in the TTM group had a diagnosis of asthma. In the DHC-only group, two patients had diabetes, one had history of congestive heart failure, one had a diagnosis of chronic obstructive pulmonary disease, two patients had documented history of coronary artery disease, and one patient had a history of stroke.
Clinical Outcomes
There were no significant TTM versus DHC-only group differences in survival to discharge (59 vs. 69 %) or in the mean modified Rankin score on follow-up (3.6 vs. 3.7); follow-up ranged between 1 and 6 months. TTM group had longer ICU length of stay (22 vs. 16 days, p = 0.03) as well as hospital length of stay (24 vs. 19 days, p = 0.03). Please see Table 2 for details on clinical outcomes of the TTM patients per category.
Decompressive Hemicraniectomy, Intracranial Pressure, and Cerebral Perfusion Pressure
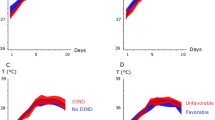
On the day of hypothermia initiation, median maximal ICP was 23.5 mmHg (IQR 18.5-27.5), decreasing to 21 mmHg (IQR 16-24.5) within 24 h of hypothermia initiation. Median lowest CPP on the day of hypothermia was 61 mmHg (IQR 54-64), increasing to 63 mmHg (IQR 60-71.25) within 24 h of hypothermia. Please see Fig. 1 for the course of ICP and CPP variation over duration of hypothermia treatment. All patients in the TTM group and 13 in the DHC-only group had EVDs placed.
DHC in the group without TTM was performed on a median hospital stay day 2 (IQR 1-3). Fourteen of the 19 TTM patients underwent DHC on a median day 5 (IQR 3-10). Median day of hypothermia initiation was day 2 (IQR 2-4), and median duration of TTM, including cooling and rewarming, was 7 days (IQR 4-12). Five of the TTM patients had DHC prior to initiation of hypothermia and one had it on the same day as hypothermia initiation. The remaining eight patients who underwent DHC did so after the initiation of hypothermia.
With regard to medications administered for ICP management (Table 3), the TTM group received significantly more hypertonic saline and mannitol and half of these patients required barbiturates, while no patients in the DHC-only group received barbiturates. The TTM group received significantly more paralytics (100 vs. 69 %).
Organ Systems Parameters
Respiratory
Patients in the TTM group were on MV support significantly longer than the DHC-only group (16 vs. 9 days, p = 0.04). They had significantly higher cumulative fluid balance (12.8 vs. 5.1 L, p = 0.009) and more days with severe hypoxemia (PaO2/FiO2 <300), 10 vs. 6 (Table 3). Since duration of MV support was significantly different between the two groups and since MV is a risk for lung injury, we examined whether the proportion of days with severe hypoxemia (PaO2/FiO2 <300) differed. We found that the proportion of days on MV with severe hypoxemia was comparable between groups (57 % of MV days for the TTM group vs. 47 % of MV days for the DHC-only group). Notably, radiographic evidence of aspiration (either via chest X-ray (CXR) or CT) was present on admission in three patients in TTM, and in one patient in the DHC-only group. Two more patients in the TTM group had evidence of aspiration during their hospital course; one during hypothermia and another following rewarming. In the subgroup of TTM patients with severe hypoxemia (n = 6, 32 %) prior to hypothermia, there was a median improvement in oxygenation (increase in PaO2/FiO2 by 17) by day 10 or the last day of hypothermia compared to a median decline in PaO2/FiO2 by 150 in those without initial hypoxemia (p = 0.03).
Overall, within the TTM group, there were little fluctuations in the surrogate measures of oxygenation (PEEP, PaO2), ventilation (PaCO2, pH), and lung protective ventilation (ideal VT, dynamic compliance) as illustrated in Figs. 2, 3, and 4.
Hematologic
Among patients who received hypothermia, there was an increase in the aPTT values during hypothermia (Fig. 5). Notably, almost half of these patients received subcutaneous heparin after the aneurysm was secured. Despite this, there was no increase in the development of intracerebral or other hemorrhage; nor were there any statistical differences in the amount of red blood cells or other blood products transfused (Table 3) between groups. In addition, the lowest documented hemoglobin and platelet counts did not differ.
Renal and Liver Function
There were no group differences for the highest documented creatinine during the hospital course, and no patients required dialysis. With regard to indices of liver function, no differences in the highest INR values were observed between groups, nor in the worst values of albumin, bilirubin, alkaline phosphatase, alanine transaminase, or aspartate transaminase, during the hospital course (Table 3).
Cardiac
There were no baseline group differences in systolic or diastolic function (Table 1). Of the 19 TTM patients, one patient developed bradycardia (defined as heart rate <40) on 2 occasions in 1 day but remained hemodynamically unaffected by these episodes. Of note, the patient received two doses of labetalol prior to episodes of bradycardia. One other patient developed Torsades de Pointes on day 13 of hypothermia while receiving 0.45 mcg/kg/min of norepinephrine and 15 mcg/kg/min of dopamine for CPP augmentation for symptomatic vasospasm that responded to magnesium and decrease in pressor doses by half. This same patient had Takotsubo cardiomyopathy and documented episodes of bradycardia prior to hypothermia on admission. The mean QTc prior to hypothermia was 477 (SD 29); it increased to 501 (SD 40) within the first 24 h of hypothermia, then decreased to 476 (SD 33) by day two and remained essentially unchanged throughout the remaining 8 days (Fig. 6).
Microbiology
Eighteen patients who had TTM protocol-driven (i.e., scheduled) blood cultures performed (from pre-hypothermia and up to the 10 days of hypothermia) remained with negative cultures, while 2 of the 14 control patients who had blood cultures drawn (up to hospital day 14) on a clinical basis proved to be positive. There were no differences in frequency of positive sputum cultures between groups, 85 % (n = 13) versus 78 % (n = 9) (Table 3).
Adverse Events
There were no group differences with regard to the following documented adverse events throughout hospital stay: critical illness myopathy, gastro-intestinal bleed, rebleeding, shock, supraventricular tachycardia, Torsades de Pointes, cardiomyopathy, vasospasm, Terson’s syndrome, dysautonomia, and seizures.
Discussion
Despite worse severity of illness and predicted prognosis for the TTM group, survival and neurologic outcomes were similar between patients who required TTM versus those who did not receive TTM (but required DHC) among our cohort patients with refractory intracranial hypertension due to aSAH. Regarding the respiratory system, TTM patients who were severely hypoxemic initially with a PaO2/FiO2 <300 improved their oxygenation following TTM, despite overall longer MV days. Indices of hematologic, renal, liver, and cardiac function were also similar between the two groups, indicating no significant injury to these organ systems resulting from TTM. We did not confirm a significant increase in microbiologic complications with prolonged hypothermia.
With a mortality of 92.5 % among aSAH patients complicated by GCE refractory to mannitol therapy [19], both DHC and TTM are often attempted to reduce ICP. DHC has been shown to significantly reduce ICP and improve survival (69–88 %) and neurologic outcomes (63–64 %) in some studies [20, 21], while others reported either death or severe disability [22] with an overall poor quality of life [23].
The benefit of TTM is potentially twofold: (1) management of ICP during GCE [9–12, 24–26], and (2) to protect against ongoing brain injury including from vasospasm pertinent to patients with aSAH [27]. The net clinical benefit, however, remains unknown. [28, 29]. The mechanisms in which hypothermia may confer these benefits may include a reduction in cerebral metabolism and cerebral metabolic consumption of oxygen (CMRO2), improvement in brain glucose utilization, a decrease in glutamate release and resultant neuronal excitotoxicity, and mitigation of reperfusion injury from free radical formation, hyperemia, inflammation, and cellular apoptosis [30].
No clinical trials have explored the role of TTM as a potential intervention to reduce DHC and whether its routine application in refractory intracranial hypertension in the setting of aSAH may improve survival and functional outcomes. Our findings provide some pilot data to indicate that such a trial may be indicated. Although survival in our cohort is comparable to other reports, the decrease in the ICP from TTM appears to be less [26], partly due to a quarter of our TTM patients having already underwent DHC. This raises the question of not just the efficacy of TTM in general for this patient population, but also what the timing of TTM should be. Should it be implemented early as a “bridge” to DHC, in lieu of DHC, or when refractory to DHC? Although our cohort is too small to compare these three subgroups with adequate power as an important limitation of the study, it appears to provide some reassurance that formal prospective investigations should be considered. It is important to note that TTM was employed as an adjunct therapy in refractory cases in our observational cohort, i.e., it was not instituted unless other measures failed accounting for more osmotherapy and barbiturate use in our cohort as an additional important confounder.
There were two primary safety concerns in our cohort associated with the use of TTM: infection and lung injury. Prior reports have raised concerns with regard to pneumonia with the use of hypothermia. Ventilator-associated pneumonia (VAP) is a well-recognized complication of mechanical ventilation, but recent advances have led to significant reduction of this complication at many centers, including our own, where implementation of the “vent bundle” led to near elimination of VAP [31]. Given this, and due to suppression of fevers, we routinely check surveillance cultures. Despite higher microbiologic findings from respiratory secretions, there was no increased incidence of shock, bacteremia, or antibiotic use, suggesting more colonization rather than infection. Others reported that in patients with traumatic brain injury (TBI) undergoing hypothermia managed with selective digestive tract decontamination, overall risk of infection was significantly lower compared to the normothermia group [32]. There are certain challenges in diagnosing a VAP in a hypothermic patient; our previous observational data suggest radiographic evidence of aspiration in 85 % of patients admitted with brain injury by noncontrast chest CT compared to 31 % by CXR alone [33]. Furthermore, aSAH frequently elicits a systemic inflammatory response syndrome [34, 35], which makes the diagnosis of infection more difficult. Since the TTM protocol prevents patients from manifesting fever, we focused on respiratory physiological variables and sputum cultures as surrogate exploratory outcomes. With regard to ARDS which can complicate hypothermia in 16–17 % [9, 10], compared to the reported rate of 30 % in TBI patients [36–39], the TTM group were more hypoxic, but TTM appeared to potentially be lung protective among those who initially presented with severe hypoxemia in the range typically seen with ARDS. This is consistent with other studies that have suggested that prolonged hypothermia may play a therapeutic role in ARDS [40, 41].
Despite safety concerns of other organs with prolonged hypothermia [9, 10, 17, 28], our study did not demonstrate significant hematologic, cardiac, liver, or renal concerns. A small increase in the aPTT likely due to ongoing subcutaneous heparin was noted, but did not translate to more transfusion requirements or bleeding complications. We observed heart rate <40 beats/minute [14] in one patient without any clinical consequence who also received beta blockade. Despite no significant effects on QTc, one patient in the TTM group did develop Torsades de Pointes but in the context of Takotsubo cardiomyopathy and pressors.
Our study has several important limitations, and our findings should be evaluated with significant caution. Most importantly, even with a cohort collected over 5 years in a busy dedicated neuro-critical care unit, the sample size limits our ability to draw definitive inferences regarding the differences between the two groups, both in terms of potential efficacy and safety. Although much of the data for the TTM group was obtained systematically based on a rigid clinical protocol, our results are still significantly limited by the inherent retrospective design and the dependency on predominantly clinically obtained variables, particularly the heightened dependence of DHC on surgical and patient preferences. We suspect that the modest achievements of hypothermia could be also due to the fact that it was started at the time when ICP was already refractory whereas in many DHC cases, patients went straight to surgery, and we do not have ICP data pre-procedure. Additionally, a quarter of our patients already had a DHC prior to implementation of TTM possibly reducing its efficacy from what has been reported previously. Additionally, although the ICPs are monitored continuously, they are recorded hourly which limits in this retrospective analysis, identification of important ICP spikes, or an assessment of compliance that is not typically charted. Finally, an important consideration is the different levels of care required when TTM is implemented, including the frequent need for paralytics, heavier sedation, longer mechanical ventilatory support requirements, and a higher use of standard interventions (osmotic therapy, fluids) prior to the implementation of TTM. These factors may affect some of the outcome variables potentially for and in some cases against the use of TTM. The strength of our findings is that the TTM group was sicker than the non-TTM patients (i.e., higher APACHE 2 scores, longer duration of mechanical ventilation, more evidence of aspiration particularly on admission, longer length of stay), and although this should bias the findings toward worse outcomes in the TTM group, there were no significant differences in survival and neurologic outcomes.
The clinical implications of our findings add to the existing body of literature that prolonged hypothermia should be considered for a systematic investigation as a potential adjunctive therapy for patients with refractory ICP elevation. As advanced care becomes more and more compartmentalized to tertiary centers, TTM may be a bridge intervention that could be considered and implemented at any hospital, without the concern for prolonged sedative effects such as barbiturates that may affect neurologic assessment. Indeed, most hospitals are already familiar with TTM for cardiac arrest patients. At least one trial is underway to examine the effect of therapeutic hypothermia after TBI [5], but a similar study in aSAH patients also appears reasonable and feasible based on our findings. Such a study should investigate not just the efficacy of TTM in the management of refractory ICP in patients with aSAH, but the timing and sequence relative to the need for DHC.
Conclusions
Use of prolonged hypothermia among aSAH patients with refractory ICP elevations is associated with higher resource utilization but appears to have comparable effects on hospital survival, neurological outcomes, and organ function compared to those who received DHC alone. A prospective study should be considered to further investigate the efficacy and safety of prolonged hypothermia as well as the timing of TTM relative to DHC in patients with refractory intracranial hypertension due to aSAH.
References
Claassen J, Carhuapoma JR, Kreiter KT, Du EY, Connolly ES, Mayer SA. Global cerebral edema after subarachnoid hemorrhage: frequency, predictors, and impact on outcome. Stroke. 2002;33(5):1225–32.
le Roux AA, Wallace MC. Outcome and cost of aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am. 2010;21(2):235–46.
Zetterling M, Hallberg L, Ronne-Engström E. Early global brain oedema in relation to clinical admission parameters and outcome in patients with aneurysmal subarachnoid haemorrhage. Acta Neurochir (Wien). 2010;152(9):1527–33.
Kreiter KT, Copeland D, Bernardini GL, et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke. 2002;33(1):200–8.
Andrews PJ et al; Eurotherm3235Trial collaborators. European society of intensive care medicine study of therapeutic hypothermia (32–35 °C) for intracranial pressure reduction after traumatic brain injury (the Eurotherm3235Trial). Trials. 2011;12:8.
Dorfer C, Frick A, Knosp E, Gruber A. Decompressive hemicraniectomy after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2010;74(4–5):465–71.
Zetterling M, Hallberg L, Hillered L, et al. Brain energy metabolism in patients with spontaneous subarachnoid hemorrhage and global cerebral edema. Neurosurgery. 2010;66(6):1102–10.
Scaravilli V, Tinchero G, Citerio G. Participants in the international multi-disciplinary consensus conference on the critical care management of subarachnoid hemorrhage. Fever management in SAH. Neurocrit Care. 2011;15(2):287–94.
Gasser S, Khan N, Yonekawa Y, Imhof HG, Keller E. Long-term hypothermia in patients with severe brain edema after poor-grade subarachnoid hemorrhage: feasibility and intensive care complications. J Neurosurg Anesthesiol. 2003;15(3):240–8.
Seule MA, Muroi C, Mink S, Yonekawa Y, Keller E. Therapeutic hypothermia in patients with aneurysmal subarachnoid hemorrhage, refractory intracranial hypertension, or cerebral vasospasm. Neurosurgery. 2009;64(1):86–92.
Kollmar R, Staykov D, Dörfler A, Schellinger PD, Schwab S, Bardutzky J. Hypothermia reduces perihemorrhagic edema after intracerebral hemorrhage. Stroke. 2010;41(8):1684–9.
Staykov D, Wagner I, Volbers B, Doerfler A, Schwab S, Kollmar R. Mild prolonged hypothermia for large intracerebral hemorrhage. Neurocrit Care. 2013;18(2):178–83.
Nunnally ME, Jaeschke R, Bellingan GJ, et al. Targeted temperature management in critical care: a report and recommendations from five professional societies. Crit Care Med. 2011;39(5):1113–25.
Polderman KH, Herold I. Therapeutic hypothermia and controlled normothermia in the intensive care unit: practical considerations, side effects, and cooling methods. Crit Care Med. 2009;37(3):1101–20.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711–37.
Pillai S, Praharaj SS, Rao GS, Kolluri VR. Cerebral perfusion pressure management of severe diffuse head injury: effect on brain compliance and intracranial pressure. Neurol India. 2004;52(1):67–71.
Mourand I, Escuret E, Héroum C, et al. Feasibility of hypothermia beyond 3 weeks in severe ischemic stroke: an open pilot study using γ-hydroxybutyrate. J Neurol Sci. 2012;316(1–2):104–7.
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33.
Heuer GG, Smith MJ, Elliott JP, Winn HR, LeRoux PD. Relationship between intracranial pressure and other clinical variables in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2004;101(3):408–16.
Smith ER, Carter BS, Ogilvy CS. Proposed use of prophylactic decompressive craniectomy in poor-grade aneurysmal subarachnoid hemorrhage patients presenting with associated large sylvian hematomas. Neurosurgery. 2002;51(1):117–24.
Schirmer CM, Hoit DA, Malek AM. Decompressive hemicraniectomy for the treatment of intractable intracranial hypertension after aneurysmal subarachnoid hemorrhage. Stroke. 2007;38(3):987–92.
Ziai WC, Port JD, Cowan JA, Garonzik IM, Bhardwaj A, Rigamonti D. Decompressive craniectomy for intractable cerebral edema: experience of a single center. J Neurosurg Anesthesiol. 2003;15(1):25–32.
D’Ambrosio AL, Sughrue ME, Yorgason JG, et al. Decompressive hemicraniectomy for poor-grade aneurysmal subarachnoid hemorrhage patients with associated intracerebral hemorrhage: clinical outcome and quality of life assessment. Neurosurgery. 2005;56(1):12–20.
Murakami M, Tsukahara T, Ishikura H, et al. Successful use of prolonged mild hypothermia in a patient with severe head injury and diffuse brain swelling. Case report. Neurol Med Chir (Tokyo). 2007;47(3):116–20.
Ng HK, Hanel R, Freeman W. Prolonged mild-to-moderate hypothermia for refractory intracranial hypertension. J Vasc Interv Neurol. 2009;2(1):142–6.
Polderman KH, Tjong Tjin Joe R, Peerdeman SM, Vandertop WP, Girbes AR. Effects of therapeutic hypothermia on intracranial pressure and outcome in patients with severe head injury. Intensive Care Med. 2002;28(11):1563–73.
Nagao S, Irie K, Kawai N, et al. Protective effect of mild hypothermia on symptomatic vasospasm: a preliminary report. Acta Neurochir Suppl. 2000;76:547–50.
Anei R, Sakai H, Iihara K, Nagata I. Effectiveness of brain hypothermia treatment in patients with severe subarachnoid hemorrhage: comparisons at a single facility. Neurol Med Chir (Tokyo). 2010;50(10):879–83.
Clifton GL, Valadka A, Zygun D, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet Neurol. 2011;10:131–9.
Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009;37(7 Suppl):S186–202.
Burger CD, Resar RK. “Ventilator bundle” approach to prevention of ventilator-associated pneumonia. Mayo Clin Proc. 2006;81(6):849–50.
Kamps M, Bisschops LA, van der Hoeven JG, Hoedemaekers CW. Hypothermia does not increase the risk of infection: a case control study. Crit Care. 2011;15(1):R48.
Ramsey, D, Hurst, R, Soto Soto, J, Freeman, M, Divertie, G, Freeman, WD. The “NAP-VAP” Study: CT chest is strongly predictive of neurologic aspiration pneumonia when compared to chest X ray on admission.In: 9th Annual Neurocritical Care Society Meeting, 2011. Poster #233.
Young AB, Ott LG, Beard D, Dempsey RJ, Tibbs PA, McClain CJ. The acute-phase response of the brain-injured patient. J Neurosurg. 1988;69(3):375–80.
Rodling-Wahlström M, Olivecrona M, Koskinen LO, Naredi S, Hultin M. Subarachnoid haemorrhage induces an inflammatory response followed by a delayed persisting increase in asymmetric dimethylarginine. Scand J Clin Lab Invest. 2012;72(6):484–9.
Hoesch RE, Lin E, Young M, et al. Acute lung injury in critical neurological illness. Crit Care Med. 2012;40(2):587–93.
Bratton SL, Davis RL. Acute lung injury in isolated traumatic brain injury. Neurosurgery. 1997;40(4):707–12.
Salim A, Martin M, Brown C, et al. The presence of the adult respiratory distress syndrome does not worsen mortality or discharge disability in blunt trauma patients with severe traumatic brain injury. Injury. 2008;39(1):30–5.
Petridis AK, Doukas A, Kienke S, et al. The effect of lung-protective permissive hypercapnia in intracerebral pressure in patients with subarachnoid haemorrhage and ARDS. A retrospective study. Acta Neurochir (Wien). 2010;152(12):2143–5.
Duan M, Berra L, Kumar A, et al. Use of hypothermia to allow low-tidal-volume ventilation in a patient with ARDS. Respir Care. 2011;56(12):1956–8.
Villar J, Slutsky AS. Effects of induced hypothermia in patients with septic adult respiratory distress syndrome. Resuscitation. 1993;26(2):183–92.
Conflict of interest
Lioudmila V Karnatovskaia, Augustine S Lee, Emir Festic, Christopher L Kramer, William D Freeman declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karnatovskaia, L.V., Lee, A.S., Festic, E. et al. Effect of Prolonged Therapeutic Hypothermia on Intracranial Pressure, Organ Function, and Hospital Outcomes Among Patients with Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care 21, 451–461 (2014). https://doi.org/10.1007/s12028-014-9989-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-9989-4