Abstract
Background
Cardiac dysfunction is a well-known complication of subarachnoid hemorrhage (SAH). Our objective was to determine the frequency of troponin abnormalities in SAH and determine its impact on in-hospital mortality.
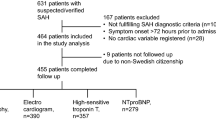
Methods
With IRB approval, we retrospectively reviewed 225 consecutive SAH patients admitted to our institution from August 1, 2006 to June 1, 2009. Traumatic SAH patients were excluded. Data were collected on demographics, Hunt and Hess score (HH), in-hospital mortality, and peak troponin values on admission. CT images were independently reviewed and graded by the study neurologist for Fisher grade (FG) and the presence of intraventricular hemorrhage (IVH).
Results
Among the 225 SAH patients, the mean age was 57.3 years (range, 21–90). The majority of patients were female (67 %), FG 3 (75 %), and had IVH (62 %). Among the 201 patients with troponin I values, the mean troponin level was 0.93 (range, 0.01–25.8 ng/mL) and 47 (23 %) had elevated troponin I levels. In unadjusted analysis, elevated troponin I level was significantly associated with in-hospital mortality. With multivariable logistic regression adjusting for age, HH, FG, and IVH, elevated troponin I level was no longer associated with in-hospital mortality (p. 0.34). In multivariate analysis, the independent predictors of in-mortality were age and severe grade HH (4–5).
Conclusions
Troponin I elevation after SAH is not an independent predictor of in-hospital mortality.

Similar content being viewed by others
References
Brouwers PJ, Wijdicks EF, Hasan D, Vermeulen M, Wever EF, Frericks H, van Gijn J. Serial electrocardiographic recording in aneurysmal subarachnoid hemorrhage. Stroke. 1989;20:1162–7.
Mayer SA, LiMandri G, Homma S, Sherman D, Fink ME, DiTullio M, Lennihan L, Beckford A, Klebanoff LM, Solomon RA. Electrocardiographic markers of abnormal left ventricular wall motion in acute subarachnoid hemorrhage. J Neurosurg. 1995;83:889–96.
Hunt D, McRae C, Zapf P. Electrocardiographic and serum enzyme changes in subarachnoid hemorrhage. Am Heart J. 1969;77:479–88.
Yoshikawa D, Hara T, Takahasi K, Morita T, Goto F. An association between QTc prolongation and left ventricular hypokinesis during sequential episodes of subarachnoid hemorrhage. Anesth Analg. 1999;89:962–4.
Zaroff JG, Rordorf GA, Newell JB, Ogilvy CS, Levinson JR. Cardiac outcome in patients with subarachnoid hemorrhage and electrocardiographic abnormalities. Neurosurgery. 1999;44:34–9.
Parekh N, Venkatesh B, Cross D, Leditschke A, Atherton J, Miles W, Winning A, Clague A, Rickard C. Cardiac troponin I predicts myocardial dysfunction in aneurysmal subarachnoid hemorrhage. J Am Coll Cardiol. 2000;36:1328–35.
Luscher MS, Thygesen K, Ravkilde J, Heickendorff L. Applicability of cardiac troponin T and I for early risk stratification in unstable coronary artery disease. TRIM study group. Thrombin inhibition in myocardial ischemia. Circulation. 1997;96:2578–85.
Deibert E, Barzilai B, Braverman AC, Edwards DR, Aiyagari V, Dacey R, Diringer M. Clinical significance of elevated troponin I levels in patients with non-traumatic subarachnoid hemorrhage. J Neurosurg. 2003;98:741–6.
Mayer SA, Fink ME, Homma S, Sherman D, Lennihan L, Solomon RA, Klebanoff LM, Beckford A, Raps EC. Cardiac injury associated with neurogenic pulmonary edema following subarachnoid hemorrhage. Neurology. 1994;44:815–20.
Tung P, Kopelnik A, Banki N, Ong K, Ko N, Lawton MT, Gress D, Drew B, Foster E, Parmley W, Zaroff J. Predictors of neurocardiogenic injury after subarachnoid hemorrhage. Stroke. 2004;35:548–51.
Ramappa P, Thatai D, Coplin W, Gellman S, Carhuapoma JR, Quah R, Atkinson B, Marsh JD. Cardiac troponin-I: a predictor of prognosis in subarachnoid hemorrhage. Neurocrit Care. 2008;8:398–403.
Naidech AM, Kreiter KT, Janjua N, Ostapkovich ND, Parra A, Commichau C, Fitzsimmons BF, Connolly ES, Mayer SA. Cardiac troponin elevation, cardiovascular morbidity, and outcome after subarachnoid hemorrhage. Circulation. 2005;112:2851–6.
Tanabe M, Crago EA, Suffoletto MS, Hravnak M, Frangiskakis JM, Kassam AB, Horowitz MB, Gorcsan J 3rd. Relation of elevation in cardiac troponin I to clinical severity, cardiac dysfunction, and pulmonary congestion in patients with subarachnoid hemorrhage. Am J Cardiol. 2008;102:1545–50.
Zaroff JG, Rordorf GA, Ogilvy CS, Picard MH. Regional patterns of left ventricular systolic dysfunction after subarachnoid hemorrhage: evidence for neurally mediated cardiac injury. J Am Soc Echocardiogr. 2000;13:774–9.
Kono T, Morita H, Kuroiwa T, Onaka H, Takatsuka H, Fujiwara A. Left ventricular wall motion abnormalities in patients with subarachnoid hemorrhage: neurogenic stunned myocardium. J Am Coll Cardiol. 1994;24:636–40.
Bulsara KR, McGirt MJ, Liao L, Villavicencio AT, Borel C, Alexander MJ, Friedman AH. Use of the peak troponin value to differentiate myocardial infarction from reversible neurogenic left ventricular dysfunction associated with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2003;98:524–8.
Lee VH, Connolly HM, Fulgham JR, Manno EM, Brown RD, Wijdicks EF. Tako-tsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: an under appreciated ventricular dysfunction. J Neurosurg. 2006;105:264–70.
Turck N, Vutskits L, Sanchez-Pena P, Robin X, Hainard A, Gex-Fabry M, Fouda C, Bassem H, Mueller M, Lisacek F, Puybasset L, Sanchez JC. A multiparameter panel method for outcome prediction following aneurysmal subarachnoid hemorrhage. Intensive Care Med. 2010;36:107–15.
Degos V, Apfel CC, Sanchez P, Colonne C, Renuit I, Clarençon F, Nouet A, Boch AL, Pourmohamad T, Kim H, Gourraud PA, Young WL, Puybasset L. An admission bio-clinical score to predict 1 year outcomes in patients undergoing aneurysm coiling. Stroke. 2012;43:1253–9.
van der Bilt IAC, Hasan D, Vandertop WP, Wilde AAM, Algra A, Visser FC, Rinkel GJE. Impact of cardiac complications on outcome after aneurysmal subarachnoid hemorrhage a meta-analysis. Neurology. 2009;72:635–42.
Yarlagadda S, Rajendran P, Miss JC, Banki NM, Kopelnik A, Wu AH, Ko N, Gelb AW, Lawton MT, Smith WS, Young WL, Zaroff JG. Cardiovascular predictors of in-patient mortality after subarachnoid hemorrhage. Neurocrit Care. 2006;05:102–7.
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A. Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke. 1994;25:1342–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupte, M., John, S., Prabhakaran, S. et al. Troponin Elevation in Subarachnoid Hemorrhage Does not Impact In-hospital Mortality. Neurocrit Care 18, 368–373 (2013). https://doi.org/10.1007/s12028-012-9813-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9813-y