Abstract
Introduction
Discrepant data exist regarding the incidence and severity of clinical problems related to intra-hospital transport of brain-injured patients and no consensus exists whether modern-day intra-hospital transport represents a safe or potentially problematic environment for neurointensive care unit (NICU) patients.
Methods
We examined the incidence of clinical complications and physiological derangements that occurred in 160 neurologically injured patients (90 males, 70 females, mean age 57 ± 17 years) who underwent intra-hospital transport (288 cases, 237 scheduled, 51 unscheduled) for computed tomography scans.
Results
Our findings indicate that (1) at least one significant complication (predominantly hemodynamic) occurred in over one-third (36 %) of all transports (p = n.s scheduled vs. unscheduled) necessitating the deployment of interventions designed to treat changes in arterial pressure (2) despite the presence of trained medical personnel and availability of specialized equipment, intra-cranial pressure was not adequately monitored during transports (especially in patients with intra-cranial hypertension prior to transport) (3) intra-hospital transfer was associated with minor but statistically significant clinical changes, including a reduction in arterial partial pressure of oxygen (\( {\text{Pa}}_{{{\text{O}}_{ 2} }} \))/inspired oxygen fraction (\( {\text{Fi}}_{{{\text{O}}_{ 2} }} \)) (only in the scheduled transport population), decreased arterial lactate levels (scheduled transport population), lowered body temperature (scheduled transport population), and increased arterial partial pressure of carbon dioxide (\( {\text{Pa}}_{{{\text{CO}}_{ 2} }} \)) (scheduled transport population).
Conclusions
Intra-hospital transport of brain-injured NICU patients may present some hazards even if performed by skilled personnel with specialized equipment. In Trauma Centers such as ours, an improvement in the frequency of neuromonitoring [intra-cranial pressure (ICP) and end-tidal CO2 (\( {\text{ET}}_{{{\text{CO}}_{ 2} }} \))] during transport is recommended.
Similar content being viewed by others
Introduction
Neurointensive care unit (NICU) patients, with differing cerebral injuries, undergo intra-hospital transport for therapeutic and diagnostic reasons that expose those patients to various hazards [1–15]. A number of problems have been previously associated with NICU patient transport, including a worsening of the patient’s clinical condition, loss or failure of the instruments required for patient monitoring and treatment, depletion of oxygen and battery power, etc. [1–15]. These unforeseen events can lead to additional hemodynamic (hypo/hypertension, arrhythmias, etc.), respiratory (hypoxia, hypo/hypercapnia, etc.), and neurologic (intra-cranial hypertension, etc.) complications. As one of the primary goals of NICU care is to prevent the development of secondary insults (hypoxia, hypotension, intra-cranial hypertension, etc.) to the injured brain [16–19], the thoroughness of clinical care during transports should approximate that found in NICU. However, previous studies provide discrepant data regarding the incidence and severity of clinical problems related to intra-hospital transports [1–15] and no consensus exists whether modern-day intra-hospital transport represents a safe or potentially dangerous environment for NICU patients. The objective of this study was to prospectively analyze the incidence of technical and clinical problems related to intra-hospital transport of 160 neurologically injured NICU patients and to evaluate the contribution of the transport to physiological derangements observed in this patient population.
Methods
This study was reviewed by the Ethics Committee of the Parma Hospital and the need for informed consent was waived, as our prospective cohort observational study did not necessitate modification of standard intensive care unit (ICU) practice related to intra-hospital transports. Of 670 patients admitted to our ICU, 230 received a diagnosis of neurological injury or disease. Of these 230 patients, 160 who required a computed tomography (CT) scan over a 1-year period were enrolled (see Table 1). In general, in our department, a patient is brought to the CT scan for diagnostic reasons due to a worsening of the clinical picture (e.g., neurological worsening or increased intra-cranial pressure (ICP)] or as a control (e.g., postoperative period). Inclusion criteria were: age over 18 years, established catheters for blood pressure monitoring, confirmed diagnosis of neurological injury or disease, and need for an intra-hospital transport for CT scan. During the ICU stay, patients were treated according to published guidelines related to traumatic brain injury (TBI) [20], subarachnoid hemorrhage (SAH) [21], intra-cerebral hemorrhage (ICH) [22, 23], and acute ischemic stroke [24]. ICP monitoring was performed using subdural, intra-ventricular, or intra-parenchymal probes (Codman, Johnson & Johnson, Raynham, MA, USA). Monitoring of ICP during the transfer was performed at the discretion of the physician involved in the transport. Personnel involved in the transport included an ICU physician and two members of the intra-hospital transport staff. The transport team travels with a backpack containing an emergency kit of airway supplies and medications. During transportation, when indicated, the patient’s head was kept at midline in a neutral position and elevated to 25–30°. Transports were classified as (1) scheduled or (2) unscheduled. Scheduled transports were arranged a minimum of 1 h before, while unscheduled transports typically organized immediately following the decision to obtain the CT scan. Five minutes before the transport, an arterial blood gas analysis (ABL 800 Flex, Radiometer Medical, Brønshøj, Denmark, Europe) was obtained and a measurement of body temperature through a tympanic device (Genius II, Covidien, Mansfield, MA, USA) was recorded. The same measurements were repeated 5 min following the end of the transport. All patients were transported on a stretcher (Translife, Maquet, Rastatt, Germany, Europe) and the bedside monitor (Infinity Delta, Draeger, Lubeck, Germany, Europe) followed the patient allowing for monitoring of cardiac rhythm, heart rate, invasive blood pressure, arterial blood oxygen saturation (\( {\text{Sp}}_{{{\text{O}}_{ 2} }} \)) and ICP. A portable mechanical ventilator (Oxilog 2000 Plus, Draeger, Lubeck, Germany, Europe) was utilized, when necessary, with identical respiratory settings (inspired oxygen fraction, positive end expiratory pressure and minute ventilation) as the NICU bedside mechanical ventilator. During CT scan examination, an anesthesia machine ventilator was utilized (Primus, Draeger, Lubeck, Germany, Europe).
The following data were recorded:
-
Type of transport (scheduled or unscheduled)
-
Transport time (min)—the transport began (T = 0) when the patient was placed on the stretcher and ended when the patient was returned to the NICU bed
-
The requirement for sedatives, analgesics, and muscle relaxants
-
Blood gas analysis parameters (pH, \( {\text{Pa}}_{{{\text{O}}_{ 2} }} \), \( {\text{Pa}}_{{{\text{CO}}_{ 2} }} \), arterial lactate) prior to, and after the transport
-
\( {\text{Pa}}_{{{\text{O}}_{ 2} }} \)/\( {\text{Fi}}_{{{\text{O}}_{ 2} }} \) ratio prior to, and after the transport
-
Any occurrence of arterial oxygen desaturation (\( {\text{Sp}}_{{{\text{O}}_{ 2} }} \) < 90 %) immediately prior to, and during the transport
-
Any type of intervention for respiratory problems during the transport
-
The occurrence of hypotension (systolic arterial pressure < 90 mmHg) immediately before and during the transport
-
The types of interventions utilized for hemodynamic problems during the transport
-
The presence of intra-cranial hypertension (ICP > 20 mmHg) and low cerebral perfusion pressure (CPP < 60 mmHg) immediately before and during the transport
-
The type of ICP monitoring
-
The type of interventions utilized for neurologic problems during the transport
-
The occurrence of technical problems during the transport such as: accidental extubation, loss of chest tubes, mechanical ventilator malfunctioning, depletion of oxygen cylinders, monitor malfunction, loss of intra-vascular devices (peripheral venous catheters, arterial catheters, central venous catheters), infusion pumps malfunctioning, loss of ICP probes, ICP monitor malfunction, loss of gastric tubes and loss of urinary catheters
-
Any need to cancel the transport and its causes.
Statistical Analysis
Continuous variables are expressed as mean ± standard deviation or as median and interquartile ranges (Q1–Q3). Categorical variables are expressed as proportions. The Shapiro–Wilks test was used for normality assessment. The continuous variables were found to follow a non-normal distribution; therefore, a non-parametric test was used for comparison of continuous variables measured before and after transport (Wilcoxon signed-rank test). Categorical variables were compared with Chi-squared test or Fisher's exact test, as appropriate. A “p” value lower than 0.05 was considered as significant. To take into account the effect of multiple comparison when analyzing the overall population and the two sub-group of patients submitted to scheduled or unscheduled transport, a Bonferroni correction was introduced and a “p” value lower than 0.0167 was considered as significant. Data analysis was performed using STATA (Version 9.1, StataCorp. College Station, Texas, USA) software package.
Results
The median SAPS II and GCS at ICU admission for all 160 patients enrolled in the present study were 43 (range = 31–54) and 5.5 (range = 3–10), respectively. Of the 288 total intra-hospital transports, 237 (83 %) were scheduled and 51 (17 %) were unscheduled. The mean duration of all intra-hospital transports was 31 ± 13 min. In 236 (82 %) of all 288 transports, the patients were intubated and mechanically ventilated. An artificial airway was present during 264 transports (185 endotracheal tubes, 79 tracheostomies). In 28 transports, the patients have a tracheostomy and breathed spontaneously. The average number of transports for each patient was 2 (range 1–10). Thirty-six percent (103) of all 288 transports was found to be associated with at least one complication, including 20 (40 %) in the unscheduled transport group and 83 (35 %) in the scheduled transport group (p = n.s. between transport groups). Further analysis revealed that over 50 % of all patients enrolled in our study (82 of 160) had, during their ICU stay, at least one transport associated with one or more complications.
The utilization of sedatives, analgesics, and muscle relaxants during all transports is outlined in Table 2. Seventy (44 %) study patients received bedside ICP monitoring during their ICU stay that included the use of ventricular (92 cases), subdural (20 cases), or intra-parenchymal [15] probes. ICP monitoring was performed “en route” in only 32 (11 %) transports (21 scheduled, 11 unscheduled), using ventricular (24 cases), subdural (2 cases), or intra-parenchymal probes (6 cases). Twenty-five percent of the patients requiring bedside ICP monitoring also required ICP monitoring during transport. Forty percent of patients with an intra-parenchymal ICP probe at bedside required ICP monitoring during transport (p = n.s. when compared to those patients with an intra-ventricular (26 %) or a subdural (10 %) probe).
Neurologic Complications
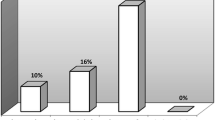
Intra-cranial hypertension during transport was observed during 21 transports (16 scheduled vs. 5 unscheduled; p = n.s; Fig. 1). In nine of these transports, intra-cranial hypertension was documented before the transport was initiated. In the 12 cases, who developed elevated ICP during transport, who did not display intra-cranial hypertension at the bedside, the treatment was as follows: sedation (7 cases), cerebrospinal fluid (CSF) drainage (1 case), CSF drainage + sedation (1 case), reduction of PEEP and sedation (1 case), sedation + osmotherapy + increase in minute volume ventilation (1 case), and rapid replacement of a malfunctioning portable mechanical ventilator (1 case). As no episodes of low CPP were observed either prior to or during transport, treatments aimed at increasing CPP were not employed. Although intra-cranial hypertension (ICP > 20 mmHg) prior to transport was present in 24 cases, ICP was monitored only during 9 (37 %) transports.
With the exception of the nine cases with documented intra-cranial hypertension before and during transport, the increase of ICP was transient and the patients returned to the ward with a normal ICP. In eight of the nine patients who have returned with intra-cranial hypertension, the level of medical care was increased and in one case a surgical intervention to remove a cerebral hematoma was performed.
Combining the data from our database with the records of the operating room, we find that in seven cases after transport, a catheter to monitor ICP was inserted because the CT scan has shown a progression of the lesion. Moreover, in nine cases, a surgical procedure was performed because the CT scan has shown an enlarging hematoma.
Respiratory Complications
During intra-hospital transport, a \( {\text{Sp}}_{{{\text{O}}_{ 2} }} \) lower than 90 % developed in 14 cases (5 %). The treatment for this respiratory complication varied between: manual positive pressure ventilation with 100 % oxygen (eight cases), broncoaspiration (five cases), and withdrawal of endotracheal tube (one case). One patient developed bronchospasm that resolved following administration of salbutamol. A second patient developed ventilatory dyssynchrony that required a supplementary dose of neuromuscular blocking drug. No significant statistical differences were observed in the incidence of arterial oxygen desaturations between scheduled and unscheduled transports (Table 3). The respiratory parameters (\( {\text{Pa}}_{{{\text{O}}_{ 2} }} \)/\( {\text{Fi}}_{{{\text{O}}_{ 2} }} \) and \( {\text{Pa}}_{{{\text{CO}}_{ 2} }} \)) before and after scheduled and unscheduled transports are outlined in Table 4.
Hemodynamic Complications
During 50 transports (17 %), a supplemental dose of sedative drugs was required to treat an increase in blood pressure (42 incidents during scheduled transports vs. 8 during unscheduled transports; p = n.s. Table 3). In 22 transports (7 %), a reduction in blood pressure required clinical intervention (17 incidents during scheduled transports vs. 5 during unscheduled transports, p = n.s. Table 3); in 11 of these, systolic blood pressure was lower than 90 mmHg (8 incidents during scheduled transports vs. 3 during unscheduled transports, p = n.s., Table 3). The interventions required for reduction in blood pressure were noradrenaline administration (11 cases), ephedrine (9 cases), ephedrine plus noradrenaline (1 case), or ephedrine plus cristalloids infusion (1 case). Arterial lactate levels before and after scheduled and unscheduled transports are presented in Table 4.
Body Temperature
Before intra-hospital transport, the mean body temperature of all patients was 36.8 ± 0.8 °C; after the transport, the mean temperature was 36.6 ± 0.8 °C (p < 0.0001). Further analysis revealed that mean body temperature before and after scheduled transports was significantly different in the scheduled transport group (36.8 ± 0.8 vs. 36.7 ± 0.8 °C; (p < 0.0001). While the mean body temperature before and after unscheduled transports remained relatively unchanged 36.6 ± 1.0 vs. 36.5 ± 0.9 °C, p = n.s.). The variations of body temperature before and after scheduled and unscheduled transports are described in Table 4.
Technical Complications
Technical complications occurred during only 17 transports (6 %) and included malfunction of ICP monitor (6 cases), loss of ICP probe (1 case), malfunction of portable mechanical ventilator (3 cases), depletion of oxygen cylinder (1 case), monitor malfunction (2 cases), arterial line malfunction (2 cases), loss of peripheral vein (1 case), and infusion pump malfunction (1 case). 11 complications occurred during scheduled transports versus 6 during unscheduled transports (p = n.s.). We determined that, in only one case, was a technical problem associated with a clinical complication: a malfunction of the portable mechanical ventilator, causing an increase of the ICP that was resolved with a quick replacement of the ventilator.
Discussion
The movement of critically ill patients from NICU for diagnostic purposes represents a daily practice and it is important for the care of patients with neurological damage. Our findings indicate that (1) in 36 % of all intra-hospital transports (both scheduled and unscheduled), at least one significant (predominantly hemodynamic), clinical complication arises during transport, necessitating the deployment of interventions designed to treat changes in arterial pressure; (2) infrequent ICP monitoring occurs during transport, particularly in patients exhibiting intra-cranial hypertension prior to transport; (3) scheduled intra-hospital transfers was associated with statistically significant reductions in \( {\text{Pa}}_{{{\text{O}}_{ 2} }} \)/\( {\text{Fi}}_{{{\text{O}}_{ 2} }} \), decreased arterial lactate levels, lowered body temperature and increased \( {\text{Pa}}_{{{\text{CO}}_{ 2} }} \).
Andrews et al. [4] prospectively evaluated secondary insults in head-injured patients who required intra-hospital transport in 35 patients who were transported from the ICU to CT scan suite or operating room and 15 patients transported from the emergency department to CT scan suite. The most common insults observed in this study were arterial hypertension (14 %), hypotension (8 %), and intra-cranial hypertension (17 %). Our results concerning hemodynamic complications during intra-hospital transport directly support these previous observations. We observed an increase in blood pressure requiring intervention that occurred during 50 transports (17 %) that could consistently be attributed to an insufficient level of sedation. When transporting a patient, it is therefore important to closely monitor levels of sedation that may change during the differing phases of transport.
We observed a marked incidence of intra-cranial hypertension during intra-hospital transport (66 %), particularly in patients who had previously exhibited intra-cranial hypertension at the NICU bedside. Based on these observations, we suggest that ICP monitoring during all transports should be mandatory in this ICU patient population. Somewhat surprisingly, we did not observe a statistically significant difference in the incidence of complications during scheduled versus unscheduled transports. We believe that the lack of differences between these groups may be related to not only lower number of unscheduled transports with respect to those that were scheduled but also heightened level of alertness and attention by the transport team to a more unstable patient population that comprised the unscheduled, emergent transport group. The lack of clinically significant changes in arterial lactate levels or decrease in body temperature suggests us that the level of patient scrutiny and clinical care during transport was comprehensive. Swanson et al. [15] retrospectively examined 100 transfers of 45 NICU patients (26 TBI, 19 SAH), comparing mean \( {\text{Pbt}}_{{{\text{O}}_{ 2} }} \) before and after transport. These authors report that intra-hospital transport negatively affected brain oxygen levels that was related to a derangement in respiratory function. A significant decrease in respiratory function (\( {\text{Pa}}_{{{\text{O}}_{ 2} }} \)/\( {\text{Fi}}_{{{\text{O}}_{ 2} }} \)) was observed during in our scheduled transport population (311 ± 137 before transport vs. 301 ± 130 after transport; p = 0.0112). However, we believe that this small worsening can be explained by the fact that our patients were not manually ventilated as in the study of Swanson et al. During all transports, we utilized a portable mechanical ventilator that allowed us to ventilate patients in as similar a manner as possible to the bedside. We suggest that the use of specialized equipment is essential to minimize potential respiratory problems related to intra-hospital transports. In addition, we observed a statistically significant elevation in mean \( {\text{Pa}}_{{{\text{CO}}_{ 2} }} \) immediately following transport (38.4 mmHg vs. 37.1 mmHg pre-transport, p < 0.0001 for all transports and 38.6 mmHg post-transport vs. 37.2 mmHg, p < 0.0001 in those patients in the scheduled transport group). Yoshihara et al. [25] have reported that in head-injured patients, a blood volume change of 0.5 ml was sufficient to produce an ICP change of as little as 1 mmHg. Additionally, Stocchetti et al. [26] observed a mean (±SD) blood volume change of 0.72 ± 0.42 ml for each mmHg change in \( {\text{Pa}}_{{{\text{CO}}_{ 2} }} \) in TBI patients. We therefore consider the rise of CO2 observed in our study to be of little clinical significance except in patients with severely impaired cerebral compliance.
Although only one negative clinical consequence related to a technical complication was observed in our study population, we believe that an elevated level of vigilance must be maintained, as previously advocated [10, 27, 28–30], concerning the proper maintenance of all devices used in intra-hospital transportation of ICU patients (mechanical ventilator, monitors, infusion pumps, etc.). Other factors that should be considered are represented by an adequate education and training of the personnel involved in the transfer of the critically ill [29, 31].
Several important limitations may be associated with our study, including its single-center design (a multicenter study might have provided broader and more widely applicable results). Additionally, our study design did not require any changes in our normal clinical practice; for example, we did not use capnography during transfers despite the fact that this monitoring technique is recommended by the ESICM (European Society of Intensive Care Medicine) in the monitoring of TBI patients [25]. It is possible, therefore, that we could not detect small changes in CO2 during transports. Differently from other papers [4, 9, 15], in our study we analyzed only the problems that may be encountered during the transport without considering a wide range of time before and after the transfer.
Despite significant recent advances in patient monitoring in the critical care setting and the publication of new guidelines [25, 30] many patients do not receive ICP monitoring during transportation. It is possible, therefore, that significant episodes of intra-cranial hypertension during intra-hospital transport may go unnoticed. The fact that ICP is monitored more frequently in those patients who have an intra-parenchymal probe may be related to its ease of use. Considering the importance of a proper control of ICP in neurological patients at risk of secondary damage, the results of our study suggest that the quality of intra-hospital transport could be improved if ICP monitoring was maintained during transport, regardless of the system used. If ICP monitoring is unavailable during transport, the risks and dangers of intra-hospital transports should be carefully weighed against the necessity of potentially lifesaving radiological scans. In this regard, it is important to note that in our population only 5.5 % of CT scan examination has led to a new surgical decision (e.g., ICP monitoring, hematoma evacuation). Futile CT scan examinations make the dangers of transport, although rare, unacceptable while some hazards are justified in case of lifesaving exams.
One possible solution to avoid uncalculated risks of intra-hospital transfers is to perform bedside CT diagnostic procedures [32]. Gunnarsson et al. [33] performed a study related to the utilization of a mobile CT scanning in a NICU setting and reported that its use minimizes the risk of secondary injury to the brain, decreased the patient’s time spent outside the ICU and reduced staff workload. However, we must also consider that patients receive twice the radiation dose of conventional CT scanning and that image resolution of larger CT scanners is somewhat superior to the mobile system for the detection of subtle alterations in attenuation [33].
Future studies should be dedicated to differentiate between true transport related events and interventions which would also be necessary if the patient is treated in the NICU; this could be done comparing patients during transport with a matched cohort of patients that remain in NICU during the same time period.
Conclusions
The results of this study suggest that intra-hospital transports of NICU patients may present some hazards even if performed by skilled personnel and specific equipment. Whenever possible, more rigorous neuromonitoring (ICP and \( {\text{ET}}_{{{\text{CO}}_{ 2} }} \)) during transport is warranted.
References
Insel J, Weissman C, Kemper M, et al. Cardiovascular changes during transport of critically ill and postoperative patients. Crit Care Med. 1986;14(6):539–42.
Braman SS, Dunn SM, Amico CA, et al. Complications of intrahospital transport in critically ill patients. Ann Intern Med. 1987;107:469–73.
Smith I, Fleming S, Cernaianu A. Mishaps during transport from the intensive care unit. Crit Care Med. 1990;18(3):278–81.
Andrews PJD, Piper IR, Deaden NM, et al. Secondary insults during intrahospital transport of head-injured patients. Lancet. 1990;335:327–30.
Hurst JM, Davis K, Johnson DJ, et al. Cost and complications during in-hospital transport of critically ill patients: a prospective cohort study. J Trauma. 1992;33(4):582–5.
Szem JW, Hydo LJ, Fischer E, et al. High-risk intrahospital transport of critically ill patients: safety and out come of the necessary “road trip”. Crit Care Med. 1995;23(10):1660–6.
Waydhas C, Schneck G, Duswald KH. Deterioration of respiratory function after intra-hospital transport of critically ill surgical patients. Intensive Care Med. 1995;21:784–9.
Wallen E, Venkataraman ST, Grosso MJ, et al. Intrahospital transport of critically ill pediatric patients. Crit Care Med. 1995;23(9):1588–95.
Bekar A, Ipekoglu Z, Tureyen K, et al. Secondary insults during intrahospital transport of neurosurgical intensive care patients. Neurosurg Rev. 1998;21:98–101.
Beckmann U, Gillies DM, Berenholtz SM, et al. Incidents relating to the intra-hospital transfer of critically ill patients. Intensive Care Med. 2004;30:1579–85.
Damm C, Vandelet P, Petit J, et al. Complications during the intrahospital transport in critically ill patients. Ann Fr Anesth Reanim. 2005;24(1):24–30.
Gillman L, Leslie G, Williams T, et al. Adverse events experienced while transferring the critically ill patient from the emergency department to the intensive care unit. Emerg Med J. 2006;23:858–61.
Papson JPN, Russell KL, Taylor D. Unexpected events during the intrahospital transport of critically ill patients. Acad Emerg Med. 2007;14(6):574–7.
Lahner D, Nikolic A, Marhofer P, et al. Incidence of complications in intrahospital transport of critically ill patients—experience in an Austrian university hospital. Wien Klin Wochenschr. 2007;119(13–14):412–6.
Swanson EW, Mascitelli J, Stiefel M, et al. Patient transport and brain oxygen in comatose patients. Neurosurgery. 2010;66:925–32.
Chesnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34(2):216–22.
Jones PA, Andrews PJ, Midgley S, et al. Measuring the burden of secondary insults in head-injured patients during intensive care. J Neurosurg Anesthesiol. 1994;6(1):4–14.
Teasdale GM, Graham DI. Craniocerebral trauma: protection and retrieval of the neuronal population after injury. Neurosurgery. 1998;42:723–38.
Marshall LF. Head injury: recent past, present and future. Neurosurgery. 2000;47:546–61.
Brain Trauma Foundation, American Association of Neurological Surgeons (AANS), Congress of Neurological Surgeons (CNS), AANS/CNS Join Section on Neurotrauma and Critical Care. Guidelines for the management of severe traumatic brain injury, 3rd edition. J Neurotrauma. 2007;24(suppl 1):S1–106.
Bederson JB, Sander Connolly E Jr, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage. Stroke. 2009;40:994–1025.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults. Stroke. 2007;38:2001–23.
Morgenstern LB, Hemphill JC III, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke. 2012;41:2108–29.
Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke. Stroke. 2007;38:1665–711.
Yoshihara M, Bandoh K, Marmarou A. Cerebrovascular carbon dioxide reactivity assessed by intracranial pressure dynamics in severely head injured patients. J Neurosurg. 1995;82:386–93.
Stocchetti N, Mattioli C, Paparella A, et al. Bedside assessment of CO2 reactivity in head injury: changes in CBF estimated by changes in ICP and cerebral extraction of oxygen [abstract]. J Neurotrauma. 1993;10(suppl):187.
Ferdinande P. Recommendations for intra-hospital transport of the severely head injured patient. Working Group on Neurosurgical Intensive Care of the European Society of Intensive Care Medicine. Intensive Care Med. 1999;25:1441–3.
Waydhas C. Intrahospital transport of critically ill patients. Crit Care. 1999;3:R83–9.
Shirley PJ, Bion JF. Intra-hospital transport of critically ill patients: minimising risk. Intensive Care Med. 2004;30:1508–10.
Warren J, Fromm RE Jr, Orr RA, et al. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–62.
Crommett JW, McCabe D, Holcomb JB. Training for the transport of mechanically ventilated patients. Respir Care Clin. 2002;8:105–18.
Haupt MT, Rehm CG. Bedside procedures. Solutions to the pitfalls of intrahospital transport. Crit Care Clin. 2000;16(1):1–6.
Gunnarsson T, Theodorsson A, Karlsson P, et al. Mobile computerized tomography scanning in the neurosurgery intensive care unit: increase in patient safety and reduction of staff workload. J Neurosurg. 2000;93:432–6.
Acknowledgments
We would like to thank Luca Longhi MD, Tracy K. McIntosh PhD and Nino Stocchetti MD for their valuable suggestions. This study would not have been possible without the exceptional commitment and contribution of the Nurses of our ICU.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Picetti, E., Antonini, M.V., Lucchetti, M.C. et al. Intra-hospital Transport of Brain-Injured Patients: A Prospective, Observational Study. Neurocrit Care 18, 298–304 (2013). https://doi.org/10.1007/s12028-012-9802-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9802-1