Abstract
Background
Neurointensive care of traumatic brain injury (TBI) patients is currently based on intracranial pressure (ICP) and cerebral perfusion pressure (CPP) targeted protocols. Monitoring brain tissue oxygenation (BtipO2) is of considerable clinical interest, but the exact threshold level of ischemia has been difficult to establish due to the complexity of the clinical situation. The objective of this study was to use the Neurovent-PTO (NV) probe, and to define critical cerebral oxygenation- and CPP threshold levels of cerebral ischemia in a standardized brain death model caused by increasing the ICP in pig. Ischemia was defined by a severe increase of cerebral microdialysis (MD) lactate/pyruvate ratio (L/P ratio > 30).
Methods
BtipO2, L/P ratio, Glucose, Glutamate, Glycerol and CPP were recorded using NV and MD probes during gradual increase of ICP by inflation of an epidural balloon catheter with saline until brain death was achieved.
Results
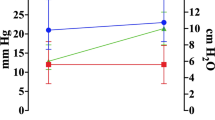
Baseline level of BtipO2 was 22.9 ± 6.2 mmHg, the L/P ratio 17.7 ± 6.1 and CPP 73 ± 17 mmHg. BtipO2 and CPP decreased when intracranial volume was added. The L/P ratio increased above its ischemic levels, (>30) when CPP decreased below 30 mmHg and BtipO2 to <10 mmHg.
Conclusions
A severe increase of ICP leading to CPP below 30 mmHg and BtipO2 below 10 mmHg is associated with an increase of the L/P ratio, thus seems to be critical thresholds for cerebral ischemia under these conditions.




Similar content being viewed by others
References
Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25:719–38.
Maas AI, Marmarou A, Murray GD, Teasdale SG, Steyerberg EW. Prognosis and clinical trial design in traumatic brain injury: the IMPACT study. J Neurotrauma. 2007;24:232–8.
Maas AI, Dearden M, Teasdale GM, et al. EBIC-guidelines for management of severe head injury in adults. European Brain Injury Consortium. Acta Neurochir (Wien). 1997;139:286–94.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. VI. Indications for intracranial pressure monitoring. J Neurotrauma. 2007;24(Suppl 1):S37–44.
Hillered L, Vespa PM, Hovda DA. Translational neurochemical research in acute human brain injury: the current status and potential future for cerebral microdialysis. J Neurotrauma. 2005;22:3–41.
Meixensberger J, Jaeger M, Vath A, Dings J, Kunze E, Roosen K. Brain tissue oxygen guided treatment supplementing ICP/CPP therapy after traumatic brain injury. J Neurol Neurosurg Psychiatry. 2003;74:760–4.
Vespa PM, McArthur D, O’Phelan K, et al. Persistently low extracellular glucose correlates with poor outcome 6 months after human traumatic brain injury despite a lack of increased lactate: a microdialysis study. J Cereb Blood Flow Metab. 2003;23:865–77.
Purins K, Sedigh A, Molnar C, et al. Standardized experimental brain death model for studies of intracranial dynamics, organ preservation, and organ transplantation in the pig. Crit Care Med. 2011;39:512–7.
Purins K, Enblad P, Sandhagen B, Lewen A. Brain tissue oxygen monitoring: a study of in vitro accuracy and stability of Neurovent-PTO and Licox sensors. Acta Neurochir (Wien). 2010;152:681–8.
Reinstrup P, Stahl N, Mellergard P, Uski T, Ungerstedt U, Nordstrom CH. Intracerebral microdialysis in clinical practice: baseline values for chemical markers during wakefulness, anesthesia, and neurosurgery. Neurosurgery. 2000;47:701–9. discussion 9–10.
Zoremba N, Schnoor J, Berens M, Kuhlen R, Rossaint R. Brain metabolism during a decrease in cerebral perfusion pressure caused by an elevated intracranial pressure in the porcine neocortex. Anesth Analg. 2007;105:744–50.
Persson L, Hillered L. Chemical monitoring of neurosurgical intensive care patients using intracerebral microdialysis. J Neurosurg. 1992;76:72–80.
Enblad P, Valtysson J, Andersson J, et al. Simultaneous intracerebral microdialysis and positron emission tomography in the detection of ischemia in patients with subarachnoid hemorrhage. J Cereb Blood Flow Metab. 1996;16:637–44.
Hutchinson PJ, Gupta AK, Fryer TF, et al. Correlation between cerebral blood flow, substrate delivery, and metabolism in head injury: a combined microdialysis and triple oxygen positron emission tomography study. J Cereb Blood Flow Metab. 2002;22:735–45.
Persson L, Valtysson J, Enblad P, et al. Neurochemical monitoring using intracerebral microdialysis in patients with subarachnoid hemorrhage. J Neurosurg. 1996;84:606–16.
Schulz MK, Wang LP, Tange M, Bjerre P. Cerebral microdialysis monitoring: determination of normal and ischemic cerebral metabolisms in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2000;93:808–14.
Stiefel MF, Spiotta A, Gracias VH, et al. Reduced mortality rate in patients with severe traumatic brain injury treated with brain tissue oxygen monitoring. J Neurosurg. 2005;103:805–11.
Meixensberger J, Kunze E, Barcsay E, Vaeth A, Roosen K. Clinical cerebral microdialysis: brain metabolism and brain tissue oxygenation after acute brain injury. Neurol Res. 2001;23:801–6.
Valadka AB, Hlatky R, Furuya Y, Robertson CS. Brain tissue pO2: correlation with cerebral blood flow. Acta Neurochir Suppl. 2002;81:299–301.
Hemphill JC 3rd, Knudson MM, Derugin N, Morabito D, Manley GT. Carbon dioxide reactivity and pressure autoregulation of brain tissue oxygen. Neurosurgery. 2001;48:377–83. discussion 83–4.
Dings J, Jager A, Meixensberger J, Roosen K. Brain tissue pO2 and outcome after severe head injury. Neurol Res. 1998;20(Suppl 1):S71–5.
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS. Relationship of brain tissue pO2 to outcome after severe head injury. Crit Care Med. 1998;26:1576–81.
van den Brink WA, van Santbrink H, Steyerberg EW, et al. Brain oxygen tension in severe head injury. Neurosurgery. 2000;46:868–76. discussion 76–8.
Orakcioglu B, Sakowitz OW, Neumann JO, Kentar MM, Unterberg A, Kiening KL. Evaluation of a novel brain tissue oxygenation probe in an experimental swine model. Neurosurgery. 2010;67:1716–22. discussion 22–3.
Hoffman WE, Charbel FT, Edelman G. Brain tissue oxygen, carbon dioxide, and pH in neurosurgical patients at risk for ischemia. Anesth Analg. 1996;82:582–6.
Pennings FA, Schuurman PR, van den Munckhof P, Bouma GJ. Brain tissue oxygen pressure monitoring in awake patients during functional neurosurgery: the assessment of normal values. J Neurotrauma. 2008;25:1173–7.
Maas AI, Fleckenstein W, de Jong DA, van Santbrink H. Monitoring cerebral oxygenation: experimental studies and preliminary clinical results of continuous monitoring of cerebrospinal fluid and brain tissue oxygen tension. Acta Neurochir Suppl (Wien). 1993;59:50–7.
Manley GT, Pitts LH, Morabito D, et al. Brain tissue oxygenation during hemorrhagic shock, resuscitation, and alterations in ventilation. J Trauma. 1999;46:261–7.
Cavus E, Bein B, Dorges V, et al. Brain tissue oxygen pressure and cerebral metabolism in an animal model of cardiac arrest and cardiopulmonary resuscitation. Resuscitation. 2006;71:97–106.
Vespa PM, O’Phelan K, McArthur D, et al. Pericontusional brain tissue exhibits persistent elevation of lactate/pyruvate ratio independent of cerebral perfusion pressure. Crit Care Med. 2007;35:1153–60.
Clifton GL, Allen S, Barrodale P, et al. A phase II study of moderate hypothermia in severe brain injury. J Neurotrauma. 1993;10:263–71. discussion 73.
Fortune JB, Feustel PJ, Weigle CG, Popp AJ. Continuous measurement of jugular venous oxygen saturation in response to transient elevations of blood pressure in head-injured patients. J Neurosurg. 1994;80:461–8.
Marion DW, Penrod LE, Kelsey SF, et al. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997;336:540–6.
Rosner MJ, Daughton S. Cerebral perfusion pressure management in head injury. J Trauma. 1990;30:933–40. discussion 40–1.
Nielsen TH, Engell SI, Johnsen RA, et al. Comparison between cerebral tissue oxygen tension and energy metabolism in experimental subdural hematoma. Neurocrit Care. 2011;15(3):585–92.
Baron JC. Perfusion thresholds in human cerebral ischemia: historical perspective and therapeutic implications. Cerebrovasc Dis. 2001;11(Suppl 1):2–8.
Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR. Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue pO2 versus jugular vein oxygen saturation. J Neurosurg. 1996;85:751–7.
Bardt TF, Unterberg AW, Hartl R, Kiening KL, Schneider GH, Lanksch WR. Monitoring of brain tissue pO2 in traumatic brain injury: effect of cerebral hypoxia on outcome. Acta Neurochir Suppl. 1998;71:153–6.
Hlatky R, Valadka AB, Goodman JC, Contant CF, Robertson CS. Patterns of energy substrates during ischemia measured in the brain by microdialysis. J Neurotrauma. 2004;21:894–906.
Doppenberg EM, Zauner A, Watson JC, Bullock R. Determination of the ischemic threshold for brain oxygen tension. Acta Neurochir Suppl. 1998;71:166–9.
Nordstrom CH, Reinstrup P, Xu W, Gardenfors A, Ungerstedt U. Assessment of the lower limit for cerebral perfusion pressure in severe head injuries by bedside monitoring of regional energy metabolism. Anesthesiology. 2003;98:809–14.
Acknowledgments
The study was supported by The Swedish Research Council. Lars Berglund, Ph.D., Uppsala Clinical Research Center, Uppsala University is acknowledged for statistical analysis. We thank Anders Nordgren, Monica Hall, and Inger Ståhl Myllyaho for their excellent laboratory assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Purins, K., Enblad, P., Wiklund, L. et al. Brain Tissue Oxygenation and Cerebral Perfusion Pressure Thresholds of Ischemia in a Standardized Pig Brain Death Model. Neurocrit Care 16, 462–469 (2012). https://doi.org/10.1007/s12028-012-9675-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9675-3