Abstract
Purpose
The aim of our study was to evaluate the relationship between the 24-h blood pressure (BP) profile, plasma NT-proBNP levels and left ventricular hypertrophy (LVH) in subjects with primary aldosteronism (PA) compared to patients with essential hypertension (EH).
Methods
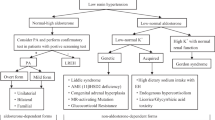
A total of 385 consecutive patients with PA [187 with aldosterone producing adenoma (APA) and 198 with idiopathic hyperaldosteronism (IHA)] and 385 patients with EH were matched based on age, sex, body mass index (BMI), BP values and duration of hypertension. Twenty-four-hour ambulatory BP monitoring (ABPM), plasma levels of NT-proBNP, left ventricular mass index (LVMI), and other clinical medical data were assessed in all patients.
Results
No differences in age, sex, BMI, clinical BP, 24-h mean BP, daytime BP, or duration of hypertension were found between groups. Nighttime systolic BP (130 ± 16 vs. 127 ± 17 mmHg, p < 0.05) and diastolic BP (82 ± 10 vs. 79 ± 11 mmHg, p < 0.01) were higher in PA patients than in EH patients. In addition, nocturnal BP decline was reduced, while median NT-proBNP (53.7 vs. 33.2 pg/ml, P < 0.001) and LVMI (113 ± 25 vs. 102 ± 26 g/m2, P < 0.001) were higher in PA patients than in EH patients. Moreover, the median NT-proBNP level was higher in APA patients than in IHA patients (68.0 vs. 42.4 pg/ml, P < 0.001). In stepwise multivariate regression analysis, LVMI was correlated with NT-proBNP, nighttime systolic BP and sex in PA patients.
Conclusions
Patients with PA show higher nighttime BP and NT-proBNP levels and lower nocturnal BP decline than those with EH. In addition, higher nocturnal systolic BP has been shown to be strongly associated with cardiac damage in PA patients.



Similar content being viewed by others
References
G. Jaffe, Z. Gray, G. Krishnan, M. Stedman, Y. Zheng, J. Han, G.M. Chertow, J.T. Leppert, V. Bhalla, Screening rates for primary aldosteronism in resistant hypertension: a cohort study. Hypertension. 75, 650–659 (2020)
P. Milliez, X. Girerd, P.F. Plouin, J. Blacher, M.E. Safar, J.J. Mourad, Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J. Am. Coll. Cardiol. 45, 1243–1248 (2005)
S. Savard, L. Amar, P.F. Plouin, O. Steichen, Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 62, 331–336 (2013)
P. Verdecchia, G. Carini, A. Circo, E. Dovellini, E. Giovannini, M. Lombardo, P. Solinas, M. Gorini, A.P. Maggioni, Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J. of the Am. Coll. of Cardiol. 38, 1829–1835 (2001)
K. Matsumura, K. Fujii, H. Oniki, M. Oka, M. Iida, Role of aldosterone in left ventricular hypertrophy in hypertension. Am. J. Hypertens. 19, 13–18 (2006)
G.P. Rossi, V. Di Bello, C. Ganzaroli, A. Sacchetto, M. Cesari, A. Bertini, D. Giorgi, R. Scognamiglio, M. Mariani, A.C. Pessina, Excess aldosterone is associated with alterations of myocardial texture in primary aldosteronism. Hypertension. 40, 23–27 (2002)
G.P. Rossi, A. Sacchetto, P. Visentin, C. Canali, G.R. Graniero, P. Palatini, A.C. Pessina, Changes in left ventricular anatomy and function in hypertension and primary aldosteronism. Hypertension. 27, 1039–1045 (1996)
M.L. Muiesan, M. Salvetti, A. Paini, C. Agabiti-Rosei, C. Monteduro, G. Galbassini, E. Belotti, C. Aggiusti, D. Rizzoni, M. Castellano, E. Agabiti-Rosei, Inappropriate left ventricular mass in patients with primary aldosteronism. Hypertension. 52, 529–534 (2008)
Y. Shigematsu, M. Hamada, H. Okayama, Y. Hara, Y. Hayashi, K. Kodama, K. Kohara, K. Hiwada, Left ventricular hypertrophy precedes other target-organ damage in primary aldosteronism. Hypertension. 29, 723–727 (1997)
K.L. Baughman, B-type natriuretic peptide - a window to the heart. N. Engl. J. Med. 347, 158–159 (2002)
O.A. Sanchez, D.R. Jacobs Jr., H. Bahrami, C.A. Peralta, L.B. Daniels, J.A. Lima, A. Maisel, D.A. Duprez, Increasing aminoterminal-pro-B-type natriuretic peptide precedes the development of arterial hypertension: the multiethnic study of atherosclerosis. J. Hypertens. 33, 966–974 (2015)
J.K. Bower, M. Lazo, K. Matsushita, J. Rubin, R.C. Hoogeveen, C.M. Ballantyne, E. Selvin, N-Terminal pro-brain natriuretic peptide (NT-proBNP) and risk of hypertension in the atherosclerosis risk in communities (ARIC) study. Am. J. Hypertens. 28, 1262–1266 (2015)
J. Xu, C. Sheng, M. Li, W. Shen, X. Tang, L. Zhu, P. Gao, J. Wang, A feasibility study on percutaneous forearm vein access for adrenal venous sampling. J. Hum. Hypertens. 31, 76–78 (2017)
S.X. Chen, Y.L. Du, J. Zhang, Y.C. Gong, Y.R. Hu, S.L. Chu, Q.B. He, Y.Y. Song, D.L. Zhu, [Aldosterone-to-renin ratio threshold for screening primary aldosteronism in Chinese hypertensive patients]. Zhonghua Xin Xue Guan Bing Za Zhi. 34, 868–872 (2006)
R.B. Devereux, M.J. Koren, G. de Simone, P.M. Okin, P. Kligfield, Methods for detection of left ventricular hypertrophy: application to hypertensive heart disease. Eur. Heart J. 14(Suppl D), 8–15 (1993)
B. Williams, G. Mancia, W. Spiering, E. Agabiti Rosei, M. Azizi, M. Burnier, D.L. Clement, A. Coca, G. de Simone, A. Dominiczak, T. Kahan, F. Mahfoud, J. Redon, L. Ruilope, A. Zanchetti, M. Kerins, S.E. Kjeldsen, R. Kreutz, S. Laurent, G.Y.H. Lip, R. McManus, K. Narkiewicz, F. Ruschitzka, R.E. Schmieder, E. Shlyakhto, C. Tsioufis, V. Aboyans, I. Desormais, 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 39, 3021–3104 (2018)
A. Grillo, S. Bernardi, A. Rebellato, B. Fabris, M. Bardelli, J. Burrello, F. Rabbia, F. Veglio, F. Fallo, R. Carretta, Ambulatory blood pressure monitoring-derived short-term blood pressure variability in primary aldosteronism. J. Clin. Hypertens. 17, 603–608 (2015)
G.A. Mansoor, W.B. White, Circadian blood pressure variation in hypertensive patients with primary hyperaldosteronism. Hypertension. 31, 843–847 (1998)
Y. Kimura, M. Kawamura, S. Onodera, K. Hiramori, Controlled study of circadian rhythm of blood pressure in patients with aldosterone-producing adenoma compared with those with essential hypertension. J. Hypertens. 18, 21–25 (2000)
C. Spieker, M. Barenbrock, K.H. Rahn, W. Zidek, Circadian blood pressure variations in endocrine disorders. Blood Press. 2, 35–39 (1993)
S. Zacharieva, M. Orbetzova, A. Elenkova, A. Stoynev, M. Yaneva, R. Schigarminova, K. Kalinov, E. Nachev, Diurnal blood pressure pattern in patients with primary aldosteronism. J. Endocrinol. Invest. 29, 26–31 (2006)
T. Zelinka, J. Widimsky, Twenty-Four hour blood pressure profile in subjects with different subtypes of primary aldosteronism. Physiol. Res. 50, 51–57 (2001)
M.P. Okoshi, X. Yan, K. Okoshi, M. Nakayama, A.J. Schuldt, T.D. O’Connell, P.C. Simpson, B.H. Lorell, Aldosterone directly stimulates cardiac myocyte hypertrophy. J. of card. fail. 10, 511–518 (2004)
R. Rocha, A.E. Rudolph, G.E. Frierdich, D.A. Nachowiak, B.K. Kekec, E.A. Blomme, E.G. McMahon, J.A. Delyani, Aldosterone induces a vascular inflammatory phenotype in the rat heart. Am. J. Physiol. Heart Circ. Physiol. 283, H1802–1810 (2002)
J.E. Yi, J. Shin, S.H. Ihm, J.H. Kim, S. Park, K.I. Kim, W.S. Kim, W.B. Pyun, Y.M. Kim, S.K. Kim, Not nondipping but nocturnal blood pressure predicts left ventricular hypertrophy in the essential hypertensive patients: the Korean Ambulatory Blood Pressure multicenter observational study. J. Hypertens. 32, 1999–2004 (2014)
C. Cuspidi, R. Facchetti, M. Bombelli, C. Sala, F. Negri, G. Grassi, G. Mancia, Nighttime blood pressure and new-onset left ventricular hypertrophy: findings from the Pamela population. Hypertension. 62, 78–84 (2013)
A.M. O’Flynn, E. Dolan, R.J. Curtin, E. O’Brien, I.J. Perry, P.M. Kearney, Night-time blood pressure and target organ damage: a comparative analysis of absolute blood pressure and dipping status. J. Hypertens. 33, 2257–2264. (2015)
W.Y. Yang, J.D. Melgarejo, L. Thijs, Z.Y. Zhang, J. Boggia, F.F. Wei, T.W. Hansen, K. Asayama, T. Ohkubo, J. Jeppesen, E. Dolan, K. Stolarz-Skrzypek, S. Malyutina, E. Casiglia, L. Lind, J. Filipovsky, G.E. Maestre, Y. Li, J.G. Wang, Y. Imai, K. Kawecka-Jaszcz, E. Sandoya, K. Narkiewicz, E. O’Brien, P. Verhamme, J.A. Staessen, Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA. 322, 409–420 (2019)
Y. Yano, R.M. Tanner, S. Sakhuja, B.C. Jaeger, J.N. Booth 3rd, M. Abdalla, D. Pugliese, S.R. Seals, G. Ogedegbe, D.W. Jones, P. Muntner, D. Shimbo, Association of daytime and nighttime blood pressure with cardiovascular disease events among African American individuals. JAMA Cardiol. 4, 910–917 (2019)
P. Jakubik, T. Janota, J. Widimsky Jr., T. Zelinka, B. Strauch, O. Petrak, H. Benakova, D. Bezdickova, D. Wichterle, T. Zima, J. Hradec, Impact of essential hypertension and primary aldosteronism on plasma brain natriuretic peptide concentration. Blood Press. 15, 302–307 (2006)
Y. Yang, L.M. Zhu, J.Z. Xu, X.F. Tang, P.J. Gao, Comparison of left ventricular structure and function in primary aldosteronism and essential hypertension by echocardiography. Hypertens. Res. 40, 243–250 (2017)
F. Pizzolo, F. Zorzi, L. Chiecchi, L. Consoli, I. Aprili, P. Guarini, A. Castagna, G.L. Salvagno, C. Pavan, O. Olivieri, NT-proBNP, a useful tool in hypertensive patients undergoing a diagnostic evaluation for primary aldosteronism. Endocrine. 45, 479–486. (2014)
W. Hu, P.H. Zhou, X.B. Zhang, C.G. Xu, W. Wang, Pathophysiological functions of adrenomedullin and natriuretic peptides in patients with primary aldosteronism. Endocrine. 48, 661–668 (2015)
Acknowledgements
This study was supported by the National Natural Science Foundation of China [81800339, 81900440], Natural Science Foundation of Shanghai Science and Technology Committee [18ZR1431800], and Fund of Shanghai Municipal Commission of Health and Family Planning [201940413, 20194Y0171].
Funding
This study was supported by the National Natural Science Foundation of China [81800339, 81900440], Natural Science Foundation of Shanghai Science and Technology Committee [18ZR1431800], and Fund of Shanghai Municipal Commission of Health and Family Planning [201940413, 20194Y0171].
Author contributions
Substantially contributed to conception or design: Q.W. and M.H.; contributed to acquisition, analysis, or interpretation of data: Q.W. and M.H.; drafted the manuscript: J.X., X.T., and L.Z.; critically revised the manuscript for important intellectual content: P.G.; gave final approval: J.X. and J.W.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics committee approval
The institutional ethics committee approved this study. Informed consent was obtained from all patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wu, Q., Hong, M., Xu, J. et al. Diurnal blood pressure pattern and cardiac damage in hypertensive patients with primary aldosteronism. Endocrine 72, 835–843 (2021). https://doi.org/10.1007/s12020-021-02606-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02606-3