Abstract
Background
Both thyroid-stimulating immunoglobulins immunoassay (TSI IA) and thyrotrophin receptor antibody immunoassay (TRAb IA) are commonly used for the diagnosis of Graves’ disease (GD). The aim of the present study was to compare the clinical diagnostic performance of these two methods.
Methods
Sera were obtained from 1103 subjects presenting a variety of clinical conditions from three centers: 100 subjects with untreated GD, 200 with treated GD, 62 with autoimmune thyroid disease(AIT), 216 with other thyroid diseases (OTHER-T), 214 with non-thyroid autoimmune diseases (NTAD), 191 with other diseases (OD), and 120 healthy subjects (HS). Both TSI and TRAb IAs were performed for all 1013 serum samples. Bioassay was performed for 86 samples whose TSI results were inconsistent the TRAb assay results.
Results
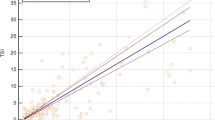
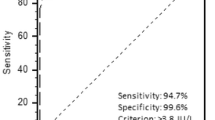
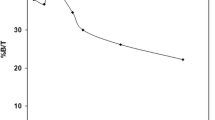
Comparing untreated GD patients with the control groups (AIT, NTAD, OTHER-T, OD, and HS) resulted in an area under the curve (AUC) of 0.992 for the TSI IA and 0.989 for the TRAb IA with no statistically significant difference observed between these AUC values (P = 0.2733). The best TSI CDP (clinical decision point) value was 0.42 IU/L. The differences in sensitivity (100% vs. 95%, P = 0.7991) and specificity (97.1% vs. 97.6%, P = 0.9426) between the TSI and TRAb IA were not statistically significant. TSI IA had a higher agreement with the TSI bioassay than TRAb IA.
Conclusion
The clinical diagnostic performance of the TSI IA for diagnosing Graves’ disease was very similar to that of the TRAb IA. TSI IA can be used to diagnose GD in the Chinese.


Similar content being viewed by others
Abbreviations
- TSHR:
-
Thyroid-stimulating hormone receptor
- TRAb:
-
Thyrotrophin receptor antibody
- TSI:
-
Thyroid-stimulating immunoglobulin
- GD:
-
Graves’ disease
- TSBAb:
-
Thyroid-stimulating blocking antibody
- IA:
-
Immunoassay
- BA:
-
Bioassay
- M22:
-
Human TSHR-stimulating antibody
- GD-UT:
-
Untreated Graves’ disease
- GD-T:
-
Treated Graves’ disease
- AIT:
-
Autoimmune thyroiditis
- OTHER-T:
-
Other thyroid diseases
- NTAD:
-
Non-thyroid autoimmune diseases
- OD:
-
Other diseases
- HS:
-
Healthy subjects
- ROC:
-
Receiver operating characteristic
- hTSHR:
-
Human thyroid-stimulating hormone receptor
- TG-Ab:
-
Thyroglobulin antibody
- TPO-Ab:
-
Thyroid peroxidase antibody
- TSH:
-
Thyroid stimulating hormone
- FT4:
-
Free thyroxine
- FT3:
-
Free triiodothyronine
- TT4:
-
Total thyroxine
- TT3:
-
Total triiodothyrogen
- CV:
-
Coefficient of variation
- SE:
-
Sensitivity
- SP:
-
Specificity
- ICC:
-
Interclass correlation coefficient
- CDP:
-
Clinical decision point
References
T.J. Smith, L. Hegedus, Graves’ disease. N. Engl. J. Med. 375(16), 1552–1565 (2016)
M.B. Zimmermann, K. Boelaert, Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 3(4), 286–295 (2015)
F. Brandt, D. Almind, K. Christensen, A. Green, T.H. Brix, L. Hegedus, Excess mortality in hyperthyroidism: the influence of preexisting comorbidity and genetic confounding: a danish nationwide register-based cohort study of twins and singletons. J. Clin. Endocrinol. Metab. 97(11), 4123–4129 (2012)
S. De Leo, S.Y. Lee, L.E. Braverman, Hyperthyroidism. Lancet (Lond., Engl.) 388(10047), 906–918 (2016)
T. Diana, P.D. Olivo, G.J. Kahaly, Thyrotropin receptor blocking antibodies. Hormone Metab. Res. 50(12), 853–862 (2018)
S.A. Morshed, T.F. Davies, Graves’ disease mechanisms: the role of stimulating, blocking, and cleavage region TSH receptor antibodies. Hormone Metab. Res. 47(10), 727–734 (2015)
B.R. Smith, R. Hall, Thyroid-stimulating immunoglobulins in Graves’ disease. Lancet (Lond., Engl.) 2(7878), 427–431 (1974)
K. Southgate, F. Creagh, M. Teece, C. Kingswood, B. Rees Smith, A receptor assay for the measurement of TSH receptor antibodies in unextracted serum. Clin. Endocrinol. 20(5), 539–548 (1984)
J. Bolton, J. Sanders, Y. Oda, C. Chapman, R. Konno, J. Furmaniak, B. Rees Smith, Measurement of thyroid-stimulating hormone receptor autoantibodies by ELISA. Clin. Chem. 45(12), 2285–2287 (1999)
S. Costagliola, N.G. Morgenthaler, R. Hoermann, K. Badenhoop, J. Struck, D. Freitag, S. Poertl, W. Weglohner, J.M. Hollidt, B. Quadbeck et al. Second generation assay for thyrotropin receptor antibodies has superior diagnostic sensitivity for Graves’ disease. J. Clin. Endocrin. Metab. 84(1), 90–97 (1999)
B.R. Smith, J. Bolton, S. Young, A. Collyer, A. Weeden, J. Bradbury, D. Weightman, P. Perros, J. Sanders, J. Furmaniak, A new assay for thyrotropin receptor autoantibodies. Thyroid 14(10), 830–835 (2004)
M. Schott, D. Hermsen, M. Broecker-Preuss, M. Casati, J.C. Mas, A. Eckstein, D. Gassner, R. Golla, C. Graeber, J. van Helden et al. Clinical value of the first automated TSH receptor autoantibody assay for the diagnosis of Graves’ disease (GD): an international multicentre trial. Clin. Endocrinol. 71(4), 566–573 (2009)
G.J. Kahaly, L. Bartalena, L. Hegedus, L. Leenhardt, K. Poppe, S.H. Pearce, 2018 European Thyroid Association guideline for the management of Graves’ hyperthyroidism. Eur. Thyroid J. 7(4), 167–186 (2018)
S.D. Lytton, G.J. Kahaly, Bioassays for TSH-receptor autoantibodies: an update. Autoimm. Rev. 10(2), 116–122 (2010)
C. Autilio, R. Morelli, P. Locantore, A. Pontecorvi, C. Zuppi, C. Carrozza, Stimulating TSH receptor autoantibodies immunoassay: analytical evaluation and clinical performance in Graves’ disease. Annal. Clin. Biochem. 55(1), 172–177 (2018)
S. Allelein, M. Ehlers, S. Goretzki, D. Hermsen, J. Feldkamp, M. Haase, T. Dringenberg, C. Schmid, H. Hautzel, M. Schott, Clinical evaluation of the first automated assay for the detection of stimulating TSH receptor autoantibodies. Hormone Metab. Res. 48(12), 795–801 (2016)
R. Tozzoli, F. D’Aurizio, D. Villalta, L. Giovanella, Evaluation of the first fully automated immunoassay method for the measurement of stimulating TSH receptor autoantibodies in Graves’ disease. Clin. Chem. Lab. Med. 55(1), 58–64 (2017)
X.H. Wan. Diagnostics (The 8th edition). (People’s Medical Publishing House, Beijing, China, 2013)
K. Soeby, P.B. Jensen, T. Werge, S. Sorensen, Mining of hospital laboratory information systems: a model study defining age- and gender-specific reference intervals and trajectories for plasma creatinine in a pediatric population. Clin. Chem. Lab. Med. 53(10), 1621–1630 (2015)
J. Yoshimura Noh, N. Miyazaki, K. Ito, K. Takeda, S. Hiramatsu, S. Morita, A. Miyauchi, T. Murakami, K. Inomata, S. Noguchi et al. Evaluation of a new rapid and fully automated electrochemiluminescence immunoassay for thyrotropin receptor autoantibodies. Thyroid 18(11), 1157–1164 (2008)
S. Doroudian, I.B. Pedersen, C.S. Knudsen, A. Handberg, S.L. Andersen, Comparison of three competitive immunoassays for measurement of TSH receptor antibodies in patients with Graves’ disease. Scand. J. Clin. Lab. Invest. 77(7), 535–540 (2017)
K. Kamijo, K. Ishikawa, M. Tanaka, Clinical evaluation of 3rd generation assay for thyrotropin receptor antibodies: the M22-biotin-based ELISA initiated by Smith. Endocrine J. 52(5), 525–529 (2005)
C. Massart, R. Sapin, J. Gibassier, A. Agin, M. d’Herbomez, Intermethod variability in TSH-receptor antibody measurement: implication for the diagnosis of Graves disease and for the follow-up of Graves ophthalmopathy. Clin. Chem. 55(1), 183–186 (2009)
I.B. Pedersen, A. Handberg, N. Knudsen, L. Heickendorff, P. Laurberg, Assays for thyroid-stimulating hormone receptor antibodies employing different ligands and ligand partners may have similar sensitivity and specificity but are not interchangeable. Thyroid 20(2), 127–133 (2010)
N.R. Syme, A.D. Toft, M. Stoddart, G.J. Beckett, Clinical performance of the Roche cobas e411 automated assay system for thyrotropin-receptor antibodies for the diagnosis of Graves’ disease. Annal. Clin. Biochemistry 48(Pt 5), 471–473 (2011)
D. Villalta, F. D’Aurizio, M. Da Re, D. Ricci, F. Latrofa, R. Tozzoli, Diagnostic accuracy of a new fluoroenzyme immunoassay for the detection of TSH receptor autoantibodies in Graves’ disease. Autoimmun. Highlights 9(1), 3 (2018)
Acknowledgements
The authors are grateful to Siemens (China) Co., Ltd, for providing technical support.
Author contributions
XC, XL, and LQ designed the study. CM, XC, and LQ analyzed the data. XL and XC were responsible for patient enrollment QJ, HZ, ZD, ZZ, YH, AS, and GY contributed materials and analyte detection. CM and XC contributed manuscript writing. All authors reviewed the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Xinqi Cheng, Xiaofeng Chai, Chaochao Ma, Qiang Jia, Honggang Zhao
Supplementary information
Rights and permissions
About this article
Cite this article
Cheng, X., Chai, X., Ma, C. et al. Clinical diagnostic performance of a fully automated TSI immunoassay vs. that of an automated anti‑TSHR immunoassay for Graves’ disease: a Chinese multicenter study. Endocrine 71, 139–148 (2021). https://doi.org/10.1007/s12020-020-02386-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02386-2