Abstract
Purpose
Adrenal incidentalomas (AI) are discovered after work-up unrelated to adrenal gland diseases; up to 30% of AI show subclinical endogenous cortisol excess (SH), frequently associated to hypertension, obesity, metabolic disorders and increased incidence of cardiovascular events (CVEs).
Methods
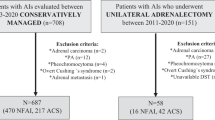
We analysed 628 AI patients divided into two groups: 471 non-functional adrenal adenoma (NFA) and 157 SH. All patients underwent complete examinations, 24-h ambulatory blood pressure monitoring, biohumoral parameters and vascular damage markers, such as c-IMT and ankle brachial index. After long-term follow-up, we registered newly onset of CVEs such as myocardial infarction (MI), percutaneous stenting and surgical bypass (PTA/CABG), stroke, overall/cardiovascular mortality. Moreover, SH patients underwent to surgical (SSH) or pharmacological treatment (MSH).
Results
SH patients showed higher prevalence of metabolic syndrome, diabetes mellitus, and previous CVEs respect NFA at baseline. After follow-up MSH group showed higher recurrence of major CV events compared with NFA and SSH (RR 2.27 MSH vs NFA for MI; RR 2.30 MSH vs NFA for PTA/CABG; RR 2.41 MSH vs NFA for stroke). In SSH there was a significant reduction of the number of antihypertensive medications needed to reach target blood pressure levels (2.3 ± 1.0 to 1.5 ± 0.4 drugs). None differences were found in SH patients, distinguished in relation to cortisol plasma levels after dexamethasone suppression test (1.8–5 µg/dL, above 5 µg/dL).
Conclusions
SH is linked to relevant cardiovascular and metabolic alterations, leading to worsen clinical outcomes. In eligible patients, adrenalectomy is valid and safe option to treat SH, reducing cardiometabolic abnormalities.


Similar content being viewed by others
References
M. Fassnacht, W. Arlt, I. Bancos, H. Dralle, J. Newell-Price, A. Sahdev, A. Tabarin, M. Terzolo, S. Tsagarakis, O.M. Dekkers, Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 175(2), G1–G34 (2016)
F. Mantero, M. Terzolo, G. Arnaldi, G. Osella, A.M. Masini, A. Alı‘, M. Giovagnetti, G. Opocher, A. Angeli, A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. J. Clin. Endocrinol. Metab. 85, 637–644 (2000)
S. Bovio, A. Cataldi, G. Reimondo, P. Sperone, S. Novello, A. Berruti, P. Borasio, C. Fava, L. Dogliotti, G.V. Scagliotti, A. Angeli, M. Terzolo, Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J. Endocrinol. Invest 29(4), 298–302 (2006)
G. Di Dalmazi, R. Pasquali, F. Beuschlein, M. Reincke, Subclinical hypercortisolism: a state, a syndrome, or a disease? Eur. J. Endocrinol. 173(4), M61–M71 (2015)
J. Shen, M. Sun, B. Zhou, J. Yan, Nonconformity in the clinical practice guidelines for subclinical Cushing’s syndrome: which guidelines are trustworthy? Eur. J. Endocrinol. 171, 421–431 (2014)
I.I. Androulakis, G. Kaltsas, G. Piaditis, A.B. Grossman, The clinical significance of adrenal incidentalomas. Eur. J. Clin. Investig. 41, 552–560 (2011)
G. Di Dalmazi, V. Vicennati, S. Garelli, E. Casadio, E. Rinaldi, E. Giampalma, C. Mosconi, R. Golfieri, A. Paccapelo, U. Pagotto, R. Pasquali, Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. Lancet Diabetes Endocrinol. 2(5), 396–405 (2014)
J. Park, A. De Luca, H. Dutton, J.C. Malcolm, M.A. Doyle, Cardiovascular outcomes in autonomous cortisol secretion and nonfunctioning adrenal adenoma: a systematic review. J. Endocr. Soc. 3(5), 996–1008 (2019)
L. Petramala, G. Cavallaro, M. Galassi, C. Marinelli, G. Tonnarini, A. Concistrè, U. Costi, M. Bufi, P. Lucia, G. De Vincentis, G. Iannucci, G. De Toma, C. Letizia, Clinical benefits of unilateral adrenalectomy in patients with subclinical hypercortisolism due to adrenal incidentaloma: results from a single center. High. Blood Press Cardiovasc Prev. 24(1), 69–75 (2017)
W.W. Mayo-Smith, G.W. Boland, R.B. Noto, M.J. Lee, State-of-the-art adrenal imaging. Radiographics 21, 995–1012 (2001)
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285(19), 2486–2497 (2001)
M. Ceruti, L. Petramala, D. Cotesta, S. Cerci, V. Serra, C. Caliumi, M. Iorio, G. De Toma, A. Ciardi, D. Vitolo, C. Letizia, Ambulatory blood pressure monitoring in secondary arterial hypertension due to adrenal diseases. J. Clin. Hypertens. 8, 642–648 (2006)
C. Fagour, S. Bardet, V. Rohmer, Y. Arimone, P. Lecomte, N. Valli, A. Tabarin, Usefulness of adrenal scintigraphy in the follow-up of adrenocortical incidentalomas: a prospective multicenter study. Eur. J. Endocrinol. 160, 257–264 (2009)
M.A. Zeiger, G.B. Thompson, Q.Y. Duh et al. On behalf of the American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr. Pract. 15, 1–20 (2009)
M. Debono, M. Bradburn, M. Bull, B. Harrison, R.J. Ross, J. Newell-Price, Cortisol as a marker for increased mortality in patients with incidental adrenocortical adenomas. J. Clin. Endocrinol. Metab. 99(12), 4462–4470 (2014)
V. Morelli, S. Palmieri, A. Lania, A. Tresoldi, S. Corbetta, E. Cairoli, C. Eller-Vainicher, M. Arosio, M. Copetti, E. Grossi, I. Chiodini, Cardiovascular events in patients with mild autonomous cortisol secretion: analysis with artificial neural networks. Eur. J. Endocrinol. 177(1), 73–83 (2017)
J. Patrova, M. Kjellman, H. Wahrenberg, H. Falhammar, Increased mortality in patients with adrenal incidentalomas and autonomous cortisol secretion: a 13-year retrospective study from one center. Endocrine 58(2), 267–275 (2017)
S. Yener, S. Ertilav, M. Secil, T. Demir, B. Akinci, L. Kebapcilar, A. Comlekci, F. Bayraktar, S. Yesil, Prospective evaluation of tumor size and hormonal status in adrenal incidentalomas. J. Endocrinol. Invest. 33(1), 32–36 (2010)
V. Morelli, G. Reimondo, R. Giordano, S. Della Casa, C. Policola, S. Palmieri, A.S. Salcuni, A. Dolci, M. Mendola, M. Arosio, B. Ambrosi, A. Scillitani, E. Ghigo, P. Beck-Peccoz, M. Terzolo, I. Chiodini, Long-term follow- up in adrenal incidentalomas: an Italian multicenter study. J. Clin. Endocrinol. Metab. 99(3), 827–834 (2014)
N. Vogelzangs, A.T.F. Beekman, Y. Milaneschi, S. Bandinelli, L. Ferrucci, Penninx BWJH. Urinary cortisol and six-year risk of all-cause and cardiovascular mortality. J. Clin. Endocrinol. Metab. 95, 4959–4964 (2010)
M. Iacobone, M. Citton, M. Scarpa, G. Viel, M. Boscaro, D. Nitti, Systematic review of surgical treatment of subclinical Cushing’s syndrome. Br. J. Surg. 102(4), 318–330 (2015)
S. Araujo-Castro, C. Robles Lázaro, P. Parra Ramírez, M. Cuesta Hernández, M.A. Sampedro Núñez, M. Marazuela, Cardiometabolic profile of non-functioning and autonomous cortisol-secreting adrenal incidentalomas. Is the cardiometabolic risk similar or are there differences? Endocrine 66(3), 650–659 (2019)
M. Kumari, M. Shipley, M. Stafford, M. Kivimaki, Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II Study. J. Clin. Endocrinol. Metab. 96, 1478–1485 (2011)
C. Scaroni, M. Zilio, M. Foti, M. Boscaro, Glucose metabolism abnormalities in cushing syndrome: from molecular basis to clinical management. Endocr. Rev. 38(3), 189–219 (2017)
E.B. Geer, J. Islam, C. Buettner, Mechanisms of glucocorticoid induced insulin resistance: focus on adipose tissue function and lipid metabolism. Endocrinol. Metab. Clin. North Am. 43(1), 75–102 (2014)
A. Rafacho, H. Ortsäter, A. Nadal, I. Quesada, Glucocorticoid treatment and endocrine pancreas function: implications for glucose homeostasis, insulin resistance and diabetes. J. Endocrinol. 223(3), R49–R62 (2014)
H. Hodabandehloo, S. Gorgani-Firuzjaee, G. Panahi, R. Meshkani, Molecular and cellular mechanisms linking inflammation to insulin resistance and b-cell dysfunction. Transl. Res. 167(1), 228–256 (2016)
D. Patsouris, J.G. Neels, W. Fan, P.P. Li, M.T. Nguyen, J.M. Olefsky, Glucocorticoids and thiazolidinediones interfere with adipocyte-mediated macrophage chemotaxis and recruitment. J. Biol. Chem. 284(45), 31223–31235 (2009)
G.B. Cansu, S. Atılgan, M.K. Balcı, R. Sarı, S. Özdem, H.A. Altunbaş, Which type 2 diabetes mellitus patients should be screened for subclinical Cushing’s syndrome? Hormones (Athens) 16(1), 22–32 (2017)
C. Letizia, L. Petramala, C.R. Di Gioia, C. Chiappetta, L. Zinnamosca, C. Marinelli, G. Iannucci, A. Ciardi, G. De Toma, G. Iacobellis, Leptin and adiponectin mRNA expression from the adipose tissue surrounding the adrenal neoplasia. J. Clin. Endocrinol. Metab. 100(1), E101–E104 (2015)
M. Weise, V. Abad, R.V. Considine, L. Nieman, K.I. Rother, Leptin secretion in Cushing’s syndrome: preservation of diurnal rhythm and absent response to corticotropin-releasing hormone. J. Clin. Endocrinol. Metab. 84(6), 2075–2079 (1999)
H. Masuzaki, Y. Ogawa, K. Hosoda, T. Miyawaki, I. Hanaoka, J. Hiraoka, A. Yasuno, H. Nishimura, Y. Yoshimasa, S. Nishi, K. Nakao, Glucocorticoid regulation of leptin synthesis and secretion in humans: elevated plasma leptin levels in Cushing’s syndrome. J. Clin. Endocrinol. Metab. 82(8), 2542–2547 (1997)
A. Babinska, M. Kaszubowski, P. Kmieć, K. Sworczak, Adipokine and cytokine levels in patients with adrenocortical cancer, subclinical Cushing’s syndrome and healthy controls. Steroids 140, 39–44 (2018)
F. Maurice, B. Gaborit, C. Vincentelli, I. Abdesselam, M. Bernard, T. Graillon, F. Kober, T. Brue, F. Castinetti, A. Dutour, Cushing syndrome is associated with subclinical LV dysfunction and increased epicardial adipose tissue. J. Am. Coll. Cardiol. 72(18), 2276–2277 (2018)
M.P. Canale, S. Manca di Villahermosa, G. Martino, V. Rovella, A. Noce, A. De Lorenzo, N. Di Daniele, Obesity-related metabolic syndrome: mechanisms of sympathetic overactivity. Int J. Endocrinol. 2013, 865965 (2013)
U.A. Hawkins, E.P. Gomez-Sanchez, C.M. Gomez-Sanchez, C.E. Gomez- Sanchez, The ubiquitous mineralocorticoid receptor: clinical implications. Curr. Hypertens. Rep. 14, 573–580 (2012)
R. Giordano, F. Guaraldi, R. Berardelli, I. Karamouzis, V. D’Angelo, E. Marinazzo, A. Picu, E. Ghigo, E. Arvat, Glucose metabolism in patients with subclinical Cushing’s syndrome. Endocrine 41, 415–423 (2012)
D. Qi, B. Rodrigues, Glucocorticoids produce whole body insulin resistance with changes in cardiac metabolism. Am. J. Physiol. Endocrinol. Metab. 292, E654–E667 (2007)
M.M. Grumbach, B.M. Biller, G.D. Braunstein, K.K. Campbell, J.A. Carney, P.A. Godley, E.L. Harris, J.K. Lee, Y.C. Oertel, M.C. Posner, J.A. Schlechte, H.S. Wieand, Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann. Intern Med 138(5), 424–429 (2003)
M. Terzolo, A. Stigliano, I. Chiodini, P. Loli, L. Furlani, G. Arnaldi, G. Reimondo, A. Pia, V. Toscano, M. Zini, G. Borretta, E. Papini, P. Garofalo, B. Allolio, B. Dupas, F. Mantero, A. Tabarin, Italian association of clinical endocrinologists. AME position statement on adrenal incidentaloma. Eur. J. Endocrinol. 164(6), 851–870 (2011)
I. Chiodini, A. Albani, A.G. Ambrogio, M. Campo, M.C. De Martino, G. Marcelli, V. Morelli, B. Zampetti, A. Colao, R. Pivonello; ABC Group, Six controversial issues on subclinical Cushing’s syndrome. Endocrine 56(2), 262–266 (2017)
R. Rossi, L. Tauchmanova, A. Luciano, M. Di Martino, C. Battista, L. Del Viscovo, V. Nuzzo, G. Lombardi, Subclinical Cushing’s syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J. Clin. Endocrinol. Metab. 85(4), 1440–1448 (2000)
A. Toniato, I. Merante-Boschin, G. Opocher, M.R. Pelizzo, F. Schiavi, E. Ballotta, Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann. Surg. 249(3), 388–391 (2009)
L. Barzon, F. Fallo, N. Sonino, M. Boscaro, Development of overt Cushing’s syndrome in patients with adrenal incidentaloma. Eur. J. Endocrinol. 146(1), 61–66 (2002)
B. de La Villéon, S. Bonnet, H. Gouya, L. Groussin, F. Tenenbaum, S. Gaujoux, B. Dousset, Long-term outcome after adrenalectomy for incidentally diagnosed subclinical cortisol-secreting adenomas. Surgery 160(2), 397–404 (2016)
L. Petramala, D. Lorenzo, G. Iannucci, A. Concistré, L. Zinnamosca, C. Marinelli, G. De Vincentis, A. Ciardi, G. De Toma, C. Letizia, Subclinical Atherosclerosis in Patients with Cushing Syndrome: Evaluation with Carotid Intima-Media Thickness and Ankle-Brachial Index. Endocrinol. Metab. 30(4), 488–493 (2015)
G. Reimondo, B. Allasino, M. Coletta et al. Evaluation of midnight salivary cortisol as a predictor factor for common carotid arteries intima media thickness in patients with clinically inapparent adrenal adenomas. Int J. Endocrinol. 2015, 674734 (2015)
M. Evran, G. Akkus, I. Berk Bozdoğan et al. Carotid intima-media thickness as the cardiometabolic risk indicator in patients with nonfunctional adrenal mass and metabolic syndrome screening. Med Sci. Monit. 22, 991–997 (2016)
N.N. Imga, O. Ucar Elalmis, M. Muslum Tuna et al. The relationship between increased epicardial fat thickness and left ventricular hypertrophy and carotid intima-media thickness in patients with nonfunctional adrenal incidentaloma. Int J. Endocrinol. Metab. 14, e37635 (2016)
R. Lupoli, P. Ambrosino, A. Tortora et al. Markers of atherosclerosis in patients with Cushing’s syndrome: a meta-analysis of literature studies. Ann. Med 49, 206–216 (2017)
P.M. Stewart, Is subclinical Cushing’s syndrome an entity or a statistical fallout from diagnostic testing? Consensus surrounding the diagnosis is required before optimal treatment can be defined. J. Clin. Endocrinol. Metab. 95(6), 2618–2620 (2010)
B. Williams, G. Mancia, W. Spiering, E. Agabiti Rosei, M. Azizi, M. Burnier, D. Clement, A. Coca, G. De Simone, A. Dominiczak, T. Kahan, F. Mahfoud, J. Redon, L. Ruilope, A. Zanchetti, M. Kerins, S. Kjeldsen, R. Kreutz, S. Laurent, G.Y.H. Lip, R. McManus, K. Narkiewicz, F. Ruschitzka, R. Schmieder, E. Shlyakhto, K. Tsioufis, V. Aboyans, I. Desormais, 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Press 27(6), 314–340 (2018)
Author information
Authors and Affiliations
Contributions
L.P., C.L., G.D.T., and G.I.: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. L.P. and C.L.: protocol/project development and manuscript writing/editing. F.O., R.R., and A.C.: manuscript writing/editing. G.D.V., M.S., and L.P.: data analysis. F.O., R.R., and A.C.: data collection or management and data analysis. M.S., G.I., and G.D.V.: data collection or management.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Petramala, L., Olmati, F., Concistrè, A. et al. Cardiovascular and metabolic risk factors in patients with subclinical Cushing. Endocrine 70, 150–163 (2020). https://doi.org/10.1007/s12020-020-02297-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02297-2