Abstract
Objective
Radiofrequency ablation (RFA) was proven as effective in reducing thyroid nodules’ volume. However, whether technical procedure aspects could influence the volume reduction rate (VRR) has not been clarified. This retrospective pilot study aimed to analyze the correlation of RFA power, duration, and energy with VRR.
Methods
During the period from June to December 2018 two primary-care centers treated benign thyroid nodules of adult outpatients according to the same RFA procedure. Technical parameters to be investigated were the following: median power (Pmedian), effective time of treatment (Teff), energy calculated as Pmedian × Teff (Ecalc), and energy delivered per mL as Kcal × 4184 × nodule’s volume (Edel). Continuous variables were analyzed by the Mann–Whitney test. Data of 1-year posttreatment follow-up were collected on December 2019 and the correlation of the above parameters with VRR was analyzed by linear regression.
Results
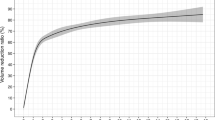
Forty-one nodules were included and their 1-year VRR was 66.6%. RFA was performed with a Pmedian of 55 W, Teff 10.24 min, Ecalc 31,380 J, and Edel 1473 J/mL. Edel was significantly correlated with VRR (p = 0.014) while Pmedian, Teff, and Ecalc not. A strong correlation of Edel with VRR was found in nodules <10 mL (p = 0.001) while no significant correlation was observed in nodules >10 mL.
Conclusions
This study showed that the energy delivered with RFA is the only technical parameter significantly correlated with the VRR of thyroid nodules.

Similar content being viewed by others
References
J.B. Vander, E.A. Gaston, T.R. Dawber, The significance of nontoxic thyroid nodules. Final report of a 15-year study of the incidence of thyroid malignancy. Ann. Intern. Med. 69(3), 537–540 (1968)
W.M. Tunbridge, D.C. Evered, R. Hall et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin. Endocrinol. 7(6), 481–493 (1977)
S. Guth, U. Theune, J. Aberle, A. Galach, C.M. Bamberger, Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur. J. Clin. Investig. 39(8), 699–706 (2009)
L. Hegedüs, S.J. Bonnema, F.N. Bennedbaek, Management of simple nodular goiter: current status and future perspectives. Endocr. Rev. 24(1), 102–132 (2003)
S. Filetti, C. Durante, M. Torlontano, Nonsurgical approaches to the management of thyroid nodules. Nat. Clin. Pract. Endocrinol. Metab. 2(7), 384–394 (2006)
E. Papini, C.M. Pacella, L.A. Solbiati, G. Achille, D. Barbaro, S. Bernardi, V. Cantisani, R. Cesareo, A. Chiti, L. Cozzaglio, A. Crescenzi, F. De Cobelli, M. Deandrea, L. Fugazzola, G. Gambelunghe, R. Garberoglio, G. Giugliano, L. Luzi, R. Negro, L. Persani, B. Raggiunti, F. Sardanelli, E. Seregni, M. Sollini, S. Spiezia, F. Stacul, D. Van Doorne, L.M. Sconfienza, G. Mauri, Minimally-invasive treatments for benign thyroid nodules: a Delphi-based consensus statement from the Italian minimally-invasive treatments of the thyroid (MITT) group. Int. J. Hyperth. 36, 376–382 (2019). https://doi.org/10.1080/02656736.2019.1575482
C.F. Dietrich, T. Müller, J. Bojunga, Y. Dong, G. Mauri, M. Radzina, M. Dighe, X.W. Cui, F. Grünwald, A. Schuler, A. Ignee, H. Korkusuz, Statement and recommendations on interventional ultrasound as a thyroid diagnostic and treatment procedure. Ultrasound Med. Biol. 44, 14–36 (2018). https://doi.org/10.1016/j.ultrasmedbio.2017.08.1889
J.H. Kim, J.H. Baek, H.K. Lim, H.S. Ahn, S.M. Baek, Y.J. Choi, Y.J. Choi, S.R. Chung, E.J. Ha, S.Y. Hahn, S.L. Jung, D.S. Kim, S.J. Kim, Y.K. Kim, C.Y. Lee, J.H. Lee, K.H. Lee, Y.H. Lee, J.S. Park, H. Park, J.H. Shin, C.H. Suh, J.Y. Sung, J.S. Sim, I. Youn, M. Choi, D.G. Na; Guideline Committee for the Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology, 2017 Thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J. Radiol. 19, 632–655 (2018). https://doi.org/10.3348/kjr.2018.19.4.632
P. Trimboli, M. Castellana, L. M. Sconfienza, C. Virili, L. C. Pescatori, R. Cesareo, F. Giorgino, R. Negro, L. Giovanella, G. Mauri, Efficacy of thermal ablation in benign non-functioning solid thyroid nodule: a systematic review and meta-analysis. Endocrine. (2019). https://doi.org/10.1007/s12020-019-02019-3
M. Deandrea, P. Trimboli, F. Garino et al. Long term efficacy of a single session RFA of benign thyroid nodules: a longitudinal 5-year observational study. J. Clin. Endocrinol. Metab. 104(9), 3751–3756 (2019)
R. Negro, M. Rucco, A. Creanza, A. Mormile, P. P. Limone, R. Garberoglio, S. Spiezia, S. Monti, C. Cugini, G. El Dalati, M. Deandrea, Machine learning prediction of radiofrequency thermal ablation efficacy: a new option to optimize thyroid nodule selection. Eur. Thyroid J. (2019). https://doi.org/10.1159/000504882
G. Gambelunghe, R. Fede, V. Bini, M. Monacelli, N. Avenia, M. D’Ajello, R. Colella, G. Nasini, P. De Feo, Ultrasound-guided interstitial laser ablation for thyroid nodules is effective only at high total amounts of energy: results from a three-year pilot study. Surg. Innov. 20, 345–350 (2013). https://doi.org/10.1177/1553350612459276
J.H. Baek, Y.S. Kim, D. Lee, J.Y. Huh, J.H. Lee, Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am. J. Roentgenol. 194, 1137–1142 (2010)
W.K. Jeong, J.H. Baek, H. Rhim, J.S. Kim, M.S. Kwak, H.J. Jeong, D. Lee, Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur. Radiol. 18, 1244–1250 (2008)
W.J. Moon, J.H. Baek, S.L. Jung, D.W. Kim, E.K. Kim, J.Y. Kim, J.Y. Kwak, J.H. Lee, J.H. Lee, Y.H. Lee, D.G. Na, J.S. Park, S.W. Park, Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J. Radiol. 12, 1–14 (2011)
S.N. Goldberg, J.W. Charboneau, G.D. Dodd 3rd, D.E. Dupuy, D.A. Gervais, A.R. Gillams, R.A. Kane, F.T. Lee Jr, T. Livraghi, J.P. McGahan, H. Rhim, S.G. Silverman, L. Solbiati, T.J. Vogl, B.J. Wood, Image-guided tumor ablation: proposal for standardization of terms and reporting criteria. Radiology 228, 335–345 (2003)
D. Sacks, T.E. McClenny, J.F. Cardella, C.A. Lewis, Society of interventional radiology clinical practice guidelines. J. Vasc. Interv. Radiol. 14, S199–S202 (2003)
G. Mauri, C.M. Pacella, E. Papini, L. Solbiati, S.N. Goldberg, M. Ahmed, L.M. Sconfienza, Image-guided thyroid ablation: proposal for standardization of terminology and reporting criteria. Thyroid 29, 611–618 (2019). https://doi.org/10.1089/thy.2018.0604
M. Mathonnet, A. Cuerq, C. Tresallet, J. C. Thalabard, E. Fery-Lemonnier, G. Russ, What is the care pathway of patients who undergo thyroid surgery in France and its potential pitfalls? A national cohort. BMJ Open 7, e013589 (2017). https://doi.org/10.1136/bmjopen-2016-013589
M. Deandrea, F. Garino, M. Alberto, R. Garberoglio, R. Rossetto, N. Bonelli, S. Spiezia, M. De Santis, S. Monti, M.G. Deiana, T. Vincenzo, C. Cugini, G. El Dalati, P.P. Limone, Radiofrequency ablation for benign thyroid nodules according to different ultrasound features: an Italian multicentre prospective study. Eur. J. Endocrinol. 180, 79–87 (2019). https://doi.org/10.1530/EJE-18-0685
G. Mauri, N. Gennaro, M.K. Lee, J.H. Baek, Laser and radiofrequency ablations for benign and malignant thyroid tumors. Int. J. Hyperth. 36, 13–20 (2019). https://doi.org/10.1080/02656736.2019.1622795
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Also, for this retrospective study, formal consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Trimboli, P., Deandrea, M. Treating thyroid nodules by radiofrequency: is the delivered energy correlated with the volume reduction rate? A pilot study. Endocrine 69, 682–687 (2020). https://doi.org/10.1007/s12020-020-02275-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02275-8