Abstract
Purpose
Nature is a phenomenal treasure of remedies. Numerous previous studies reported that Nigella sativa NS improved glycemic control, reduced insulin resistance, and improved lipid profile. NS was never investigated before as a monotherapy for newly diagnosed type 2 diabetes mellitus T2DM patients. Our aim was to investigate the potential metabolic benefits of NS monotherapy in newly diagnosed T2DM patients.
Method
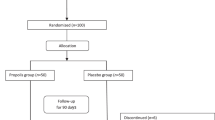
Prospective, open-label randomized clinical trial at outpatient endocrinology clinic at Ain-Shams University hospital. Eligible patients were randomly assigned to either metformin tablets or NS oil capsules. Both groups received treatment for 3 months. Glycemic index (FBG, 2 h pp, A1C, insulin sensitivity %S, secretory function %B, insulin resistance IR), lipid profile (TC, LDL, HDL, TG), liver and kidney functions (AST, ALT, Sr cr), total antioxidant capacity TAC, weight, waist circumference WC and body mass index BMI were assessed at baseline and at the end of treatment period.
Results
A concentration of 1350 mg/day NS in newly diagnosed T2DM patients was inferior to metformin in terms of lowering FBG, 2 h pp, and A1C or increasing %B. However, NS was comparable to metformin in lowering weight, WC, and BMI significantly. NS was comparable to metformin in regards of their effects on fasting insulin, %S, IR, ALT, TC, LDL, HDL, TG, and TAC. Metformin showed significant increase in AST and creatinine which was reserved in NS group.
Conclusion
NS administration in newly diagnosed T2DM was tolerable with no side effects as compared to metformin; however, it was inferior to metformin in terms of diabetes management.

Similar content being viewed by others
References
D.C. Ziemer, P. Kolm, W.S. Weintraub, V. Vaccarino, M.K. Rhee, J.G. Twombly, K.M. Narayan, D.D. Koch, L.S. Phillips, Glucose-independent, black-white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann. Intern. Med. 152(12), 770–777 (2010). https://doi.org/10.7326/0003-4819-152-12-201006150-00004
M. Janghorbani, M.R. Salamat, M. Amini, A. Aminorroaya, Risk of diabetes according to the metabolic health status and degree of obesity. Diabetes Metab. Syndr. 11(Suppl 1), S439–S444 (2017). https://doi.org/10.1016/j.dsx.2017.03.032
X. Li, K. Watanabe, I. Kimura, Gut microbiota dysbiosis drives and implies novel therapeutic strategies for diabetes mellitus and related metabolic diseases. Front. Immunol. 8, 1882 (2017). https://doi.org/10.3389/fimmu.2017.01882
M.J. Berridge, Vitamin D deficiency and diabetes. Biochem. J. 474(8), 1321–1332 (2017). https://doi.org/10.1042/BCJ20170042
A. Cheema, D. Adeloye, S. Sidhu, D. Sridhar, K.Y. Chan, Urbanization and prevalence of type 2 diabetes in Southern Asia. A systematic analysis. J. Glob. Health 4(1), 010404 (2014). https://doi.org/10.7189/jogh.04.010404
J.D. Schofield, Y. Liu, P. Rao-Balakrishna, R.A. Malik, H. Soran, Diabetes dyslipidemia. diabetes Ther. 7(2), 203–219 (2016). https://doi.org/10.1007/s13300-016-0167-x
T.V. Fiorentino, A. Prioletta, P. Zuo, F. Folli, Hyperglycemia-induced oxidative stress and its role in diabetes mellitus related cardiovascular diseases. Curr. Pharm. Des. 19(32), 5695–5703 (2013)
U. Asmat, K. Abad, K. Ismail, Diabetes mellitus and oxidative stress-A concise review. Saudi Pharm. J. 24(5), 547–553 (2016). https://doi.org/10.1016/j.jsps.2015.03.013
M.S. Kirkman, M.T. Rowan-Martin, R. Levin, V.A. Fonseca, J.A. Schmittdiel, W.H. Herman, R.E. Aubert, Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care 38(4), 604–609 (2015). https://doi.org/10.2337/dc14-2098
Hemmingsen, B., Lund, S. S., Gluud, C., Vaag, A., Almdal, T. P., Hemmingsen, C., Wetterslev, J. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database Syst. Rev. CD008143 (2013). https://doi.org/10.1002/14651858.CD008143.pub3
American Diabetes, A., 8. pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2018. Diabetes Care 41(Suppl 1), S73–S85 (2018). https://doi.org/10.2337/dc18-S008
M.F. Kadir, M.S. Bin Sayeed, T. Shams, M.M. Mia, Ethnobotanical survey of medicinal plants used by Bangladeshi traditional health practitioners in the management of diabetes mellitus. J. Ethnopharmacol. 144(3), 605–611 (2012). https://doi.org/10.1016/j.jep.2012.09.050
W. Qidwai, H.B. Hamza, R. Qureshi, A. Gilani, Effectiveness, safety, and tolerability of powdered Nigella sativa (kalonji) seed in capsules on serum lipid levels, blood sugar, blood pressure, and body weight in adults: results of a randomized, double-blind controlled trial. J. Altern. Complement. Med. 15(6), 639–644 (2009). https://doi.org/10.1089/acm.2008.0367
J. Heshmati, N. Namazi, Effects of black seed (Nigella sativa) on metabolic parameters in diabetes mellitus: a systematic review. Complement. Ther. Med. 23(2), 275–282 (2015). https://doi.org/10.1016/j.ctim.2015.01.013
A. Bamosa, H. Kaatabi, A. Badar, A. Al-Khadra, A. Al Elq, B. Abou-Hozaifa, F. Lebda, S. Al-Almaie, Nigella sativa: A potential natural protective agent against cardiac dysfunction in patients with type 2 diabetes mellitus. J. Fam. Community Med. 22(2), 88–95 (2015). https://doi.org/10.4103/2230-8229.155380
E. Farzaneh, F.R. Nia, M. Mehrtash, F.S. Mirmoeini, M. Jalilvand, The effects of 8-week nigella sativa supplementation and aerobic training on lipid profile and VO2 max in sedentary overweight females. Int. J. Prev. Med. 5(2), 210–216 (2014)
J. Javanbakht, R. Hobbenaghi, E. Hosseini, A.M. Bahrami, F. Khadivar, S. Fathi, M.A. Hassan, Histopathological investigation of neuroprotective effects of Nigella sativa on motor neurons anterior horn spinal cord after sciatic nerve crush in rats. Pathol.-Biol. 61(6), 250–253 (2013). https://doi.org/10.1016/j.patbio.2013.03.007
A.A. Sayed, Thymoquinone and proanthocyanidin attenuation of diabetic nephropathy in rats. Eur. Rev. Med. Pharmacol. Sci. 16(6), 808–815 (2012)
A. Benhaddou-Andaloussi, L. Martineau, T. Vuong, B. Meddah, P. Madiraju, A. Settaf, P.S. Haddad, The in vivo antidiabetic activity of nigella sativa is mediated through activation of the ampk pathway and increased muscle Glut4 content. Evid.Based Complement. Altern. Med. 2011, 538671 (2011). https://doi.org/10.1155/2011/538671
N. Houstis, E.D. Rosen, E.S. Lander, Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440(7086), 944–948 (2006). https://doi.org/10.1038/nature04634
B. Meddah, R. Ducroc, M. El Abbes Faouzi, B. Eto, L. Mahraoui, A. Benhaddou-Andaloussi, L.C. Martineau, Y. Cherrah, P.S: Haddad, Nigella sativa inhibits intestinal glucose absorption and improves glucose tolerance in rats. J. Ethnopharmacol. 121(3), 419–424 (2009). https://doi.org/10.1016/j.jep.2008.10.040
W. Sobhi, C. Stevigny, P. Duez, B.B. Calderon, D. Atmani, M. Benboubetra, Effect of lipid extracts of Nigella sativa L. seeds on the liver ATP reduction and alpha-glucosidase inhibition. Pak. J. Pharm. Sci. 29(1), 111–117 (2016)
S. Alimohammadi, R. Hobbenaghi, J. Javanbakht, D. Kheradmand, R. Mortezaee, M. Tavakoli, F. Khadivar, H. Akbari, Protective and antidiabetic effects of extract from Nigella sativa on blood glucose concentrations against streptozotocin (STZ)-induced diabetic in rats: an experimental study with histopathological evaluation. Diagn. Pathol. 8, 137 (2013). https://doi.org/10.1186/1746-1596-8-137
A.O. Bamosa, H. Kaatabi, F.M. Lebdaa, A.M. Elq, A. Al-Sultanb, Effect of Nigella sativa seeds on the glycemic control of patients with type 2 diabetes mellitus. Indian J. Physiol. Pharmacol. 54(4), 344–354 (2010)
A. Benhaddou-Andaloussi, L.C. Martineau, D. Vallerand, Y. Haddad, A. Afshar, A. Settaf, P.S. Haddad, Multiple molecular targets underlie the antidiabetic effect of Nigella sativa seed extract in skeletal muscle, adipocyte and liver cells. Diabetes, Obes. Metab. 12(2), 148–157 (2010). https://doi.org/10.1111/j.1463-1326.2009.01131.x
K.M. Fararh, Y. Atoji, Y. Shimizu, T. Shiina, H. Nikami, T. Takewaki, Mechanisms of the hypoglycaemic and immunopotentiating effects of Nigella sativa L. oil in streptozotocin-induced diabetic hamsters. Res. Vet. Sci. 77(2), 123–129 (2004). https://doi.org/10.1016/j.rvsc.2004.03.002
E.A. Datau, Wardhana, E.E. Surachmanto, K. Pandelaki, J.A. Langi, Fias: Efficacy of Nigella sativa on serum free testosterone and metabolic disturbances in central obese male. Acta Med. Indones. 42(3), 130–134 (2010)
M. Tauseef Sultan, M.S. Butt, F.M. Anjum, Safety assessment of black cumin fixed and essential oil in normal Sprague Dawley rats: Serological and hematological indices. Food Chem. Toxicol. 47(11), 2768–2775 (2009). https://doi.org/10.1016/j.fct.2009.08.011
H. Kaatabi, A.O. Bamosa, A. Badar, A. Al-Elq, B. Abou-Hozaifa, F. Lebda, A. Al-Khadra, S. Al-Almaie, Nigella sativa improves glycemic control and ameliorates oxidative stress in patients with type 2 diabetes mellitus: placebo controlled participant blinded clinical trial. PLoS ONE 10(2), e0113486 (2015). https://doi.org/10.1371/journal.pone.0113486
American Diabetes, A., (2) Classification and diagnosis of diabetes. Diabetes Care 38(Suppl), S8–S16 (2015). https://doi.org/10.2337/dc15-S005
Network, S.P. Research randomizer. (2015). https://www.randomizer.org/about/. Accessed 03 Feb 2016
unit, U.o.O.D.t. HOMA2 calculator. (2014). http://www.dtu.ox.ac.uk/homacalculator/download.php. Accessed 03 Feb 2016
P. Gayoso-Diz, A. Otero-Gonzalez, M.X. Rodriguez-Alvarez, F. Gude, F. Garcia, A. De Francisco, A.G. Quintela, Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr. Disord. 13, 47 (2013). https://doi.org/10.1186/1472-6823-13-47
L. Guariguata, D. Whiting, C. Weil, N. Unwin, The International Diabetes Federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res. Clin. Pract. 94(3), 322–332 (2011). https://doi.org/10.1016/j.diabres.2011.10.040
D.J. Newman, G.M. Cragg, Natural products as sources of new drugs over the 30 years from 1981 to 2010. J. Nat. Prod. 75(3), 311–335 (2012). https://doi.org/10.1021/np200906s
S. Hasani-Ranjbar, Z. Jouyandeh, M. Abdollahi, A systematic review of anti-obesity medicinal plants - an update. J. Diabetes Metab. Disord. 12(1), 28 (2013). https://doi.org/10.1186/2251-6581-12-28
F. Amin, N. Islam, N. Anila, A.H. Gilani, Clinical efficacy of the co-administration of Turmeric and Black seeds (Kalongi) in metabolic syndrome - a double blind randomized controlled trial - TAK-MetS trial. Complement. Ther. Med. 23(2), 165–174 (2015). https://doi.org/10.1016/j.ctim.2015.01.008
M.A. Farhangi, P. Dehghan, S. Tajmiri, Powdered black cumin seeds strongly improves serum lipids, atherogenic index of plasma and modulates anthropometric features in patients with Hashimoto’s thyroiditis. Lipids Health Dis. 17(1), 59 (2018). https://doi.org/10.1186/s12944-018-0704-x
S. Asgary, A. Sahebkar, N. Goli-Malekabadi, Ameliorative effects of Nigella sativa on dyslipidemia. J. Endocrinol. Investig. 38(10), 1039–1046 (2015). https://doi.org/10.1007/s40618-015-0337-0
M. el-Dakhakhny, Studies on the Egyptian Nigella sativa L. IV. Some pharmacological properties of the seeds’ active principle in comparison to its dihydro compound and its polymer. Arzneim. Forsch. 15(10), 1227–1229 (1965)
A. Badar, H. Kaatabi, A. Bamosa, A. Al-Elq, B. Abou-Hozaifa, F. Lebda, A. Alkhadra, S. Al-Almaie, Effect of Nigella sativa supplementation over a one-year period on lipid levels, blood pressure and heart rate in type-2 diabetic patients receiving oral hypoglycemic agents: nonrandomized clinical trial. Ann. Saudi Med. 37(1), 56–63 (2017). https://doi.org/10.5144/0256-4947.2017.56
L. Wang, P. Lin, A. Ma, H. Zheng, K. Wang, W. Li, C. Wang, R. Zhao, K. Liang, F. Liu, X. Hou, J. Song, Y. Lu, P. Zhu, Y. Sun, L. Chen, C-peptide is independently associated with an increased risk of coronary artery disease in t2dm subjects: a cross-sectional study. PLoS ONE 10(6), e0127112 (2015). https://doi.org/10.1371/journal.pone.0127112
H. Shafiq, A. Ahmad, T. Masud, M. Kaleem, Cardio-protective and anti-cancer therapeutic potential of Nigella sativa. Iran. J. Basic Med. Sci. 17(12), 967–979 (2014)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moustafa, H.A.M., El Wakeel, L.M., Halawa, M.R. et al. Effect of Nigella Sativa oil versus metformin on glycemic control and biochemical parameters of newly diagnosed type 2 diabetes mellitus patients. Endocrine 65, 286–294 (2019). https://doi.org/10.1007/s12020-019-01963-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01963-4