Abstract
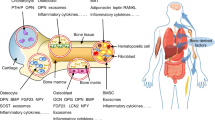
Metabolic bone disease occurs when there is a net loss in bone density. Osteoporosis, the most common metabolic bone disease, is a devastating problem and an increasingly major public health issue. A substantial body of evidence in the elderly population indicates that a relationship exists between the components of body weight and various measures of bone/mass, density, and function. Both muscle and fat contribute to the body’s total weight and the intimate associations of muscle, fat, and bone are known. But the close functional interactions between muscle and bone or fat and bone are largely unidentified and have drawn much attention in recent years. Each of these tissues not only responds to afferent signals from traditional hormone systems and the central nervous systems but also secretes factors with important endocrine functions. Studies suggest that during growth, development, and aging, the relationship of muscle and fat with the skeleton possibly governs bone homeostasis and turnover. A better understanding of the endocrine function and the cellular and molecular mechanisms and pathways linking muscle or adipose tissues with bone anabolism and catabolism is a new avenue for novel pathways for anabolic drug discovery. These in turn will likely lead to more rational therapy toward increasingly prevalent disorders like osteoporosis. In this review, some of the recent works on the interaction of bone with muscle and fat are highlighted, and in so doing the role of parathyroid hormone (PTH), and PTH-related peptide (PTHrP) is surveyed.

Similar content being viewed by others
References
X. Feng, J.M. McDonald, Disorders of bone remodeling. Annu. Rev. Pathol. 6, 121–145 (2011)
L.G. Raisz, Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J. Clin. Invest. 115, 3318–3325 (2005)
S. Khosla, B.L. Riggs, Pathophysiology of age-related bone loss and osteoporosis. Endocrinol. Metab. Clin. North Am. 34, 1015–1030 (2005)
U.S.D.o.H.a.H. Services, National healthcare disparities report, Agency for healthcare research and quality, in: www.ahrq.gov/qual/qrdr11.htm, pp. 98–102 (2011). Accessed 28 Apr 2014
G. Mazziotti, J. Bilezikian, E. Canalis, D. Cocchi, A. Giustina, New understanding and treatments for osteoporosis. Endocrine 41, 58–69 (2012)
C.J. Rosen, J.P. Bilezikian, Clinical review 123: anabolic therapy for osteoporosis. J. Clin. Endocrinol. Metab. 86, 957–964 (2001)
E.M. Greenfield, Anabolic effects of intermittent PTH on osteoblasts. Curr. Mol. Pharmacol. 5, 127–134 (2012)
N.S. Datta, Osteoporotic fracture and parathyroid hormone. World J. Orthop. 2, 67–74 (2011)
P.D. Miller, J.P. Bilezikian, M. Diaz-Curiel, P. Chen, F. Marin, J.H. Krege, M. Wong, R. Marcus, Occurrence of hypercalciuria in patients with osteoporosis treated with teriparatide. J. Clin. Endocrinol. Metab. 92, 3535–3541 (2007)
K.A. Cappuzzo, J.C. Delafuente, Teriparatide for severe osteoporosis. Ann. Pharmacother. 38, 294–302 (2004)
A. Sikon, P. Batur, Profile of teriparatide in the management of postmenopausal osteoporosis. Int. J. Womens Health 2, 37–44 (2010)
L. Pietrogrande, Update on the efficacy, safety, and adherence to treatment of full length parathyroid hormone, PTH (1-84), in the treatment of postmenopausal osteoporosis. Int. J. Womens Health 1, 193–203 (2010)
M.P. Herrmann-Erlee, J.N. Heersche, J.W. Hekkelman, P.J. Gaillard, G.W. Tregear, J.A. Parsons, J.T. Potts Jr, Effects of bone in vitro of bovine parathyroid hormone and synthetic fragments representing residues 1–34, 2–34 and 3–34. Endocr. Res. Commun. 3, 21–35 (1976)
T.F. DeBartolo, L.E. Pegg, C. Shasserre, T.J. Hahn, Comparison of parathyroid hormone and calcium ionophore A23187 effects on bone resorption and nucleic acid synthesis in cultured fetal rat bone. Calcif. Tissue Int. 34, 495–500 (1982)
B.R. MacDonald, J.A. Gallagher, R.G. Russell, Parathyroid hormone stimulates the proliferation of cells derived from human bone. Endocrinology 118, 2445–2449 (1986)
E. Canalis, M. Centrella, W. Burch, T.L. McCarthy, Insulin-like growth factor I mediates selective anabolic effects of parathyroid hormone in bone cultures. J. Clin. Invest. 83, 60–65 (1989)
S. Nishida, A. Yamaguchi, T. Tanizawa, N. Endo, T. Mashiba, Y. Uchiyama, T. Suda, S. Yoshiki, H.E. Takahashi, Increased bone formation by intermittent parathyroid hormone administration is due to the stimulation of proliferation and differentiation of osteoprogenitor cells in bone marrow. Bone 15, 717–723 (1994)
N.C. Partridge, X. Li, L. Qin, Understanding parathyroid hormone action. Ann. NY Acad. Sci. 1068, 187–193 (2006)
N.S. Datta, R. Kolailat, G.J. Pettway, J.E. Berry, L.K. McCauley, PTH and PTHrP induces mitogen activated protein kinase phosphatase-1 in differentiated bone marrow stromal cells, mouse osteoblast and cementoblast cell lines. J. Bone Miner. Res. 22, S137 (2007)
R. Lindsay, H. Zhou, F. Cosman, J. Nieves, D.W. Dempster, A.B. Hodsman, Effects of a one-month treatment with PTH(1–34) on bone formation on cancellous, endocortical, and periosteal surfaces of the human ilium. J. Bone Miner. Res. 22, 495–502 (2007)
N.S. Datta, C. Chen, J.E. Berry, L.K. McCauley, PTHrP signaling targets cyclin D1 and induces osteoblastic cell growth arrest. J. Bone Miner. Res. 20, 1051–1064 (2005)
N.S. Datta, R. Kolailat, A. Fite, G. Pettway, A.B. Abou-Samra, Distinct roles for mitogen-activated protein kinase phosphatase-1 (MKP-1) and ERK-MAPK in PTH1R signaling during osteoblast proliferation and differentiation. Cell. Signal. 22, 457–466 (2010)
G.J. Pettway, J.A. Meganck, A.J. Koh, E.T. Keller, S.A. Goldstein, L.K. McCauley, Parathyroid hormone mediates bone growth through the regulation of osteoblast proliferation and differentiation. Bone 42, 806–818 (2008)
J.M. Hock, L.A. Fitzpatrick, J.P. Bilezikian, Actions of parathyroid hormone, in Principles of Bone Biology, 2nd edn., ed. by J.P. Bilezikian, L.G. Raisz, G.A. Rodan (Academic Press, San Diego, 2002), pp. 463–482
J.M. Hock, V. Krishnan, J.E. Onyia, J.P. Bidwell, J. Milas, D. Stanislaus, Osteoblast apoptosis and bone turnover. J. Bone Miner. Res. 16, 975–984 (2001)
R.L. Jilka, R.S. Weinstein, T. Bellido, P. Roberson, A.M. Parfitt, S.C. Manolagas, Increased bone formation by prevention of osteoblast apoptosis with parathyroid hormone. J. Clin. Invest. 104, 439–446 (1999)
S.C. Manolagas, Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr. Rev. 21, 115–137 (2000)
H. Dobnig, R.T. Turner, Evidence that intermittent treatment with parathyroid hormone increases bone formation in adult rats by activation of bone lining cells. Endocrinology 136, 3632–3638 (1995)
D. Leaffer, M. Sweeney, L.A. Kellerman, Z. Avnur, J.L. Krstenansky, B.H. Vickery, J.P. Caulfield, Modulation of osteogenic cell ultrastructure by RS-23581, an analog of human parathyroid hormone (PTH)-related peptide-(1–34), and bovine PTH-(1–34). Endocrinology 136, 3624–3631 (1995)
Y. Rhee, M.R. Allen, K. Condon, V. Lezcano, A.C. Ronda, C. Galli, N. Olivos, G. Passeri, C.A. O’Brien, N. Bivi, L.I. Plotkin, T. Bellido, PTH receptor signaling in osteocytes governs periosteal bone formation and intra-cortical remodeling. J. Bone Miner. Res. 26, 1035–1046 (2011)
D. Goltzman, Studies on the mechanisms of the skeletal anabolic action of endogenous and exogenous parathyroid hormone. Arch. Biochem. Biophys. 473, 218–224 (2008)
N.S. Datta, A.B. Abou-Samra, PTH and PTHrP signaling in osteoblasts. Cell. Signal. 21, 1245–1254 (2009)
L.K. McCauley, T.J. Martin, Twenty-five years of PTHrP progress: from cancer hormone to multifunctional cytokine. J. Bone Miner. Res. 27, 1231–1239 (2012)
Y.Y. Kong, U. Feige, I. Sarosi, B. Bolon, A. Tafuri, S. Morony, C. Capparelli, J. Li, R. Elliott, S. McCabe, T. Wong, G. Campagnuolo, E. Moran, E.R. Bogoch, G. Van, L.T. Nguyen, P.S. Ohashi, D.L. Lacey, E. Fish, W.J. Boyle, J.M. Penninger, Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature 402, 304–309 (1999)
Y.T. Teng, H. Nguyen, X. Gao, Y.Y. Kong, R.M. Gorczynski, B. Singh, R.P. Ellen, J.M. Penninger, Functional human T-cell immunity and osteoprotegerin ligand control alveolar bone destruction in periodontal infection. J. Clin. Invest. 106, R59–R67 (2000)
R. Pacifici, Osteoimmunology and its implications for transplantation. Am. J. Transpl. 13, 2245–2254 (2013)
R. Baum, E.M. Gravallese, Impact of inflammation on the osteoblast in rheumatic diseases. Curr. Osteoporos. Rep. 12, 9–16 (2014)
A. Di Benedetto, I. Gigante, S. Colucci, M. Grano, Periodontal disease: linking the primary inflammation to bone loss. Clin. Dev. Immunol. 2013, 503754 (2013)
J.L. Funk, A role for parathyroid hormone-related protein in the pathogenesis of inflammatory/autoimmune diseases. Int. Immunopharmacol. 1, 1101–1121 (2001)
R. Alemzadeh, J. Kichler, Parathyroid hormone is associated with biomarkers of insulin resistance and inflammation, independent of vitamin D status, in obese adolescents. Metab. Syndr. Relat. Disord. 10, 422–429 (2012)
V. Bhatia, S.O. Kim, J.F. Aronson, C. Chao, M.R. Hellmich, M. Falzon, Role of parathyroid hormone-related protein in the pro-inflammatory and pro-fibrogenic response associated with acute pancreatitis. Regul. Pept. 175, 49–60 (2012)
H. Kaji, Linkage between muscle and bone: common catabolic signals resulting in osteoporosis and sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 16, 272–277 (2013)
J.D. Schipilow, H.M. Macdonald, A.M. Liphardt, M. Kan, S.K. Boyd, Bone micro-architecture, estimated bone strength, and the muscle-bone interaction in elite athletes: an HR-pQCT study. Bone 56, 281–289 (2013)
M.F. Barbe, S. Gallagher, V.S. Massicotte, M. Tytell, S.N. Popoff, A.E. Barr-Gillespie, The interaction of force and repetition on musculoskeletal and neural tissue responses and sensorimotor behavior in a rat model of work-related musculoskeletal disorders. BMC Musculoskelet. Disord. 14, 303 (2013)
J. Rittweger, G. Beller, J. Ehrig, C. Jung, U. Koch, J. Ramolla, F. Schmidt, D. Newitt, S. Majumdar, H. Schiessl, D. Felsenberg, Bone-muscle strength indices for the human lower leg. Bone 27, 319–326 (2000)
E. Schoenau, From mechanostat theory to development of the “Functional Muscle-Bone-Unit”. J. Musculoskelet. Neuronal Interact. 5, 232–238 (2005)
M.H. Edwards, C.L. Gregson, H.P. Patel, K.A. Jameson, N.C. Harvey, A.A. Sayer, E.M. Dennison, C. Cooper, Muscle size, strength, and physical performance and their associations with bone structure in the Hertfordshire Cohort Study. J. Bone Miner. Res. 28, 2295–2304 (2013)
C. Cipriani, E. Romagnoli, V. Carnevale, I. Raso, A. Scarpiello, M. Angelozzi, A. Tancredi, S. Russo, F. De Lucia, J. Pepe, S. Minisola, Muscle strength and bone in healthy women: effect of age and gonadal status. Hormones (Athens) 11, 325–332 (2012)
J.H. Park, K.H. Park, S. Cho, Y.S. Choi, S.K. Seo, B.S. Lee, H.S. Park, Concomitant increase in muscle strength and bone mineral density with decreasing IL-6 levels after combination therapy with alendronate and calcitriol in postmenopausal women. Menopause 20, 747–753 (2013)
H.T. Ma, J.F. Griffith, L. Xu, P.C. Leung, The functional muscle-bone unit in subjects of varying BMD. Osteoporos. Int. 25, 999–1004 (2014)
V. Bokan, Muscle weakness and other late complications of diabetic polyneuropathy. Acta Clin. Croat. 50, 351–355 (2011)
T.T. van Sloten, H.H. Savelberg, I.G. Duimel-Peeters, K. Meijer, R.M. Henry, C.D. Stehouwer, N.C. Schaper, Peripheral neuropathy, decreased muscle strength and obesity are strongly associated with walking in persons with type 2 diabetes without manifest mobility limitations. Diab. Res. Clin. Pract. 91, 32–39 (2011)
P. Vestergaard, Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos. Int. 18, 427–444 (2007)
D.R. Sinacore, M.K. Hastings, K.L. Bohnert, F.A. Fielder, D.T. Villareal, V.P. Blair 3rd, J.E. Johnson, Inflammatory osteolysis in diabetic neuropathic (charcot) arthropathies of the foot. Phys. Ther. 88, 1399–1407 (2008)
G. Mabilleau, M.E. Edmonds, Role of neuropathy on fracture healing in Charcot neuro-osteoarthropathy. J. Musculoskelet. Neuronal Interact. 10, 84–91 (2010)
S. Balducci, M. Sacchetti, G. Orlando, L. Salvi, L. Pugliese, G. Salerno, V. D’Errico, C. Iacobini, F.G. Conti, S. Zanuso, A. Nicolucci, G. Pugliese, Correlates of muscle strength in diabetes: The study on the assessment of determinants of muscle and bone strength abnormalities in diabetes (SAMBA). Nutr. Metab. Cardiovasc. Dis. 23(11), 1037–1042 (2013)
B. Roy, Biomolecular basis of the role of diabetes mellitus in osteoporosis and bone fractures. World J. Diabet. 4, 101–113 (2013)
L. Gennari, D. Merlotti, R. Valenti, E. Ceccarelli, M. Ruvio, M.G. Pietrini, C. Capodarca, M.B. Franci, M.S. Campagna, A. Calabro, D. Cataldo, K. Stolakis, F. Dotta, R. Nuti, Circulating sclerostin levels and bone turnover in type 1 and type 2 diabetes. J. Clin. Endocrinol. Metab. 97, 1737–1744 (2012)
S. Judex, C.T. Rubin, Is bone formation induced by high-frequency mechanical signals modulated by muscle activity? J. Musculoskelet. Neuronal Interact. 10, 3–11 (2010)
P. Juffer, R.T. Jaspers, P. Lips, A.D. Bakker, J. Klein-Nulend, Expression of muscle anabolic and metabolic factors in mechanically loaded MLO-Y4 osteocytes. Am. J. Physiol. Endocrinol. Metab. 302, E389–E395 (2012)
L. Ferrucci, M. Baroni, A. Ranchelli, F. Lauretani, M. Maggio, P. Mecocci, C. Ruggiero, Interaction between bone and muscle in older persons with mobility limitations. Curr. Pharm. Des. (2013) [Epub ahead of print]
L.F. Bonewald, The amazing osteocyte. J. Bone Miner. Res. 26, 229–238 (2011)
K.R. Chien, G. Karsenty, Longevity and lineages: toward the integrative biology of degenerative diseases in heart, muscle, and bone. Cell 120, 533–544 (2005)
B.K. Pedersen, M.A. Febbraio, Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol. Rev. 88, 1379–1406 (2008)
B.K. Pedersen, F. Edward, Adolph distinguished lecture: muscle as an endocrine organ: IL-6 and other myokines. J. Appl. Physiol. 107, 1006–1014 (2009)
W.M. Jackson, A.B. Aragon, J.D. Bulken-Hoover, L.J. Nesti, R.S. Tuan, Putative heterotopic ossification progenitor cells derived from traumatized muscle. J. Orthop. Res. 27, 1645–1651 (2009)
W.S. Zundel, F.H. Tyler, The muscular dystrophies. N. Engl. J. Med. 273, 537–543 (1965)
T. Harslof, M. Frost, T.L. Nielsen, L.B. Husted, M. Nyegaard, K. Brixen, A.D. Borglum, L. Mosekilde, M. Andersen, L. Rejnmark, B.L. Langdahl, Polymorphisms of muscle genes are associated with bone mass and incident osteoporotic fractures in Caucasians. Calcif. Tissue Int. 92, 467–476 (2013)
B. Buehring, N. Binkley, Myostatin: the holy grail for muscle, bone, and fat? Curr. Osteoporos. Rep. 11, 407–414 (2013)
M.N. Elkasrawy, M.W. Hamrick, Myostatin (GDF-8) as a key factor linking muscle mass and bone structure. J. Musculoskelet. Neuronal Interact. 10, 56–63 (2010)
M. Elkasrawy, S. Fulzele, M. Bowser, K. Wenger, M. Hamrick, Myostatin (GDF-8) inhibits chondrogenesis and chondrocyte proliferation in vitro by suppressing Sox-9 expression. Growth Factors 29, 253–262 (2011)
M.W. Hamrick, The skeletal muscle secretome: an emerging player in muscle-bone crosstalk. BoneKEy Rep. 1, 60 (2012)
M.W. Hamrick, P.L. McNeil, S.L. Patterson, Role of muscle-derived growth factors in bone formation. J. Musculoskelet. Neuronal Interact. 10, 64–70 (2010)
M. Hamrick, JMNI special issue: basic science and mechanisms of muscle-bone interactions. J. Musculoskelet. Neuronal Interact. 10, 1–2 (2010)
H. Kaufman, A. Reznick, H. Stein, M. Barak, G. Maor, The biological basis of the bone-muscle inter-relationship in the algorithm of fracture healing. Orthopedics 31, 751 (2008)
K. Walsh, Adipokines, myokines and cardiovascular disease. Circ. J. 73, 13–18 (2009)
K. Tanaka, E. Matsumoto, Y. Higashimaki, T. Katagiri, T. Sugimoto, S. Seino, H. Kaji, Role of osteoglycin in the linkage between muscle and bone. J. Biol. Chem. 287, 11616–11628 (2012)
M.C. Gozo, P.J. Aspuria, D.J. Cheon, A.E. Walts, D. Berel, N. Miura, B.Y. Karlan, S. Orsulic, Foxc2 induces Wnt4 and Bmp4 expression during muscle regeneration and osteogenesis. Cell Death Differ. 20, 1031–1042 (2013)
W. Qin, L. Sun, J. Cao, Y. Peng, L. Collier, Y. Wu, G. Creasey, J. Li, Y. Qin, J. Jarvis, W.A. Bauman, M. Zaidi, C. Cardozo, The central nervous system (CNS)-independent anti-bone-resorptive activity of muscle contraction and the underlying molecular and cellular signatures. J. Biol. Chem. 288, 13511–13521 (2013)
K.D. Schluter, H.M. Piper, Cardiovascular actions of parathyroid hormone and parathyroid hormone-related peptide. Cardiovasc. Res. 37, 34–41 (1998)
I. Tastan, R. Schreckenberg, S. Mufti, Y. Abdallah, H.M. Piper, K.D. Schluter, Parathyroid hormone improves contractile performance of adult rat ventricular cardiomyocytes at low concentrations in a non-acute way. Cardiovasc. Res. 82, 77–83 (2009)
M.R. Rutledge, V. Farah, A.A. Adeboye, M.R. Seawell, S.K. Bhattacharya, K.T. Weber, Parathyroid hormone, a crucial mediator of pathologic cardiac remodeling in aldosteronism. Cardiovasc. Drugs Ther. 27, 161–170 (2013)
J. Jansen, P. Gres, C. Umschlag, F.R. Heinzel, H. Degenhardt, K.D. Schluter, G. Heusch, R. Schulz, Parathyroid hormone-related peptide improves contractile function of stunned myocardium in rats and pigs. Am. J. Physiol. Heart Circ. Physiol. 284, H49–H55 (2003)
J. Qian, M.C. Colbert, D. Witte, C.Y. Kuan, E. Gruenstein, H. Osinska, B. Lanske, H.M. Kronenberg, T.L. Clemens, Midgestational lethality in mice lacking the parathyroid hormone (PTH)/PTH-related peptide receptor is associated with abrupt cardiomyocyte death. Endocrinology 144, 1053–1061 (2003)
Y. Fei, G. Gronowicz, M.M. Hurley, Fibroblast growth factor-2, bone homeostasis and fracture repair. Curr. Pharm. Des. 19, 3354–3363 (2013)
Y. Fei, M.M. Hurley, Role of fibroblast growth factor 2 and Wnt signaling in anabolic effects of parathyroid hormone on bone formation. J. Cell. Physiol. 227, 3539–3545 (2012)
S. Yakar, H.W. Courtland, D. Clemmons, IGF-1 and bone: new discoveries from mouse models. J. Bone Miner. Res. 25, 2543–2552 (2010)
D.R. Clemmons, The diagnosis and treatment of growth hormone deficiency in adults. Curr. Opin. Endocrinol. Diabet. Obes. 17, 377–383 (2010)
A. Giustina, A. Barkan, P. Chanson, A. Grossman, A. Hoffman, E. Ghigo, F. Casanueva, A. Colao, S. Lamberts, M. Sheppard, S. Melmed, Guidelines for the treatment of growth hormone excess and growth hormone deficiency in adults. J. Endocrinol. Invest. 31, 820–838 (2008)
L.E. Olson, C. Ohlsson, S. Mohan, The Role of GH/IGF-I-Mediated mechanisms in sex differences in cortical bone size in mice. Calcif. Tissue Int. 88, 1–8 (2011)
T. Brioche, R.A. Kireev, S. Cuesta, A. Gratas-Delamarche, J.A. Tresguerres, M.C. Gomez-Cabrera, J. Vina, Growth hormone replacement therapy prevents sarcopenia by a dual mechanism: improvement of protein balance and of antioxidant defenses. J. Gerontol. Ser. A 2013, 1079–5006 (2013)
K. Ho, V. Chikani, Action of GH on skeletal muscle: molecular and functional mechanisms. J. Mol. Endocrinol. 52, R107–R123 (2013)
A. Giustina, G. Mazziotti, E. Canalis, Growth hormone, insulin-like growth factors, and the skeleton. Endocr. Rev. 29, 535–559 (2008)
D.D. Bikle, Y. Wang, Insulin like growth factor-I: a critical mediator of the skeletal response to parathyroid hormone. Curr. Mol. Pharmacol. 5, 135–142 (2012)
G. Lombardi, C. Di Somma, L. Vuolo, E. Guerra, E. Scarano, A. Colao, Role of IGF-I on PTH effects on bone. J. Endocrinol. Invest. 33, 22–26 (2010)
E. Schoenau, Bone mass increase in puberty: what makes it happen? Horm. Res. 65(Suppl 2), 2–10 (2006)
C. Rommel, S.C. Bodine, B.A. Clarke, R. Rossman, L. Nunez, T.N. Stitt, G.D. Yancopoulos, D.J. Glass, Mediation of IGF-1-induced skeletal myotube hypertrophy by PI(3)K/Akt/mTOR and PI(3)K/Akt/GSK3 pathways. Nat. Cell Biol. 3, 1009–1013 (2001)
D.R. Vyas, E.E. Spangenburg, T.W. Abraha, T.E. Childs, F.W. Booth, GSK-3beta negatively regulates skeletal myotube hypertrophy. Am. J. Physiol. Cell Physiol. 283, C545–C551 (2002)
C.G. Tahimic, Y. Wang, D.D. Bikle, Anabolic effects of IGF-1 signaling on the skeleton. Front. Endocrinol. 4, 6 (2013)
K.B. Hagen, H. Dagfinrud, R.H. Moe, N. Osteras, I. Kjeken, M. Grotle, G. Smedslund, Exercise therapy for bone and muscle health: an overview of systematic reviews. BMC Med. 10, 167 (2012)
S. Franckhauser, I. Elias, V. Rotter Sopasakis, T. Ferre, I. Nagaev, C.X. Andersson, J. Agudo, J. Ruberte, F. Bosch, U. Smith, Overexpression of Il6 leads to hyperinsulinaemia, liver inflammation and reduced body weight in mice. Diabetologia 51, 1306–1316 (2008)
K. Kayamori, K. Sakamoto, T. Nakashima, H. Takayanagi, K. Morita, K. Omura, S.T. Nguyen, Y. Miki, T. Iimura, A. Himeno, T. Akashi, H. Yamada-Okabe, E. Ogata, A. Yamaguchi, Roles of interleukin-6 and parathyroid hormone-related peptide in osteoclast formation associated with oral cancers: significance of interleukin-6 synthesized by stromal cells in response to cancer cells. Am. J. Pathol. 176, 968–980 (2010)
C.J. Rosen, A. Klibanski, Bone, fat, and body composition: evolving concepts in the pathogenesis of osteoporosis. Am. J. Med. 122, 409–414 (2009)
A. Cohen, D.W. Dempster, R.R. Recker, J.M. Lappe, H. Zhou, A. Zwahlen, R. Muller, B. Zhao, X. Guo, T. Lang, I. Saeed, X.S. Liu, X.E. Guo, S. Cremers, C.J. Rosen, E.M. Stein, T.L. Nickolas, D.J. McMahon, P. Young, E. Shane, Abdominal fat is associated with lower bone formation and inferior bone quality in healthy premenopausal women: a transiliac bone biopsy study. J. Clin. Endocrinol. Metab. 98, 2562–2572 (2013)
A.J. Sogaard, K. Holvik, T.K. Omsland, G.S. Tell, C. Dahl, B. Schei, J.A. Falch, J.A. Eisman, H.E. Meyer, Abdominal obesity increases the risk of hip fracture. A population-based study of 43,000 women and men aged 60-79 years followed for 8 years. Cohort of Norway. J. Intern. Med. (2014). doi:10.1111/joim.12230
J.J. Cao, Effects of obesity on bone metabolism. J. Orthop. Surg. Res. 6, 30 (2011)
M. Kawai, F.J. de Paula, C.J. Rosen, New insights into osteoporosis: the bone-fat connection. J. Intern. Med. 272, 317–329 (2012)
M.A. Bredella, C.M. Gill, C.J. Rosen, A. Klibanski, M. Torriani, Positive effects of brown adipose tissue on femoral bone structure. Bone 58, 55–58 (2014)
S. Rahman, Y. Lu, P.J. Czernik, C.J. Rosen, S. Enerback, B. Lecka-Czernik, Inducible brown adipose tissue, or beige fat, is anabolic for the skeleton. Endocrinology 154, 2687–2701 (2013)
A.V. Schwartz, S. Sigurdsson, T.F. Hue, T.F. Lang, T.B. Harris, C.J. Rosen, E. Vittinghoff, K. Siggeirsdottir, G. Sigurdsson, D. Oskarsdottir, K. Shet, L. Palermo, V. Gudnason, X. Li, Vertebral bone marrow fat associated with lower trabecular BMD and prevalent vertebral fracture in older adults. J. Clin. Endocrinol. Metab. 98, 2294–2300 (2013)
K.J. Motyl, K.A. Bishop, V.E. DeMambro, S.A. Bornstein, P. Le, M. Kawai, S. Lotinun, M.C. Horowitz, R. Baron, M.L. Bouxsein, C.J. Rosen, Altered thermogenesis and impaired bone remodeling in Misty mice. J. Bone Miner. Res. 28, 1885–1897 (2013)
M.A. Bredella, P.K. Fazeli, B. Lecka-Czernik, C.J. Rosen, A. Klibanski, IGFBP-2 is a negative predictor of cold-induced brown fat and bone mineral density in young non-obese women. Bone 53, 336–339 (2013)
M.A. Bredella, P.K. Fazeli, L.M. Freedman, G. Calder, H. Lee, C.J. Rosen, A. Klibanski, Young women with cold-activated brown adipose tissue have higher bone mineral density and lower Pref-1 than women without brown adipose tissue: a study in women with anorexia nervosa, women recovered from anorexia nervosa, and normal-weight women. J. Clin. Endocrinol. Metab. 97, E584–E590 (2012)
J. Mohiti-Ardekani, H. Soleymani-Salehabadi, M.B. Owlia, A. Mohiti, Relationships between serum adipocyte hormones (adiponectin, leptin, resistin), bone mineral density and bone metabolic markers in osteoporosis patients. J. Bone Miner. Metab. (2013) [Epub ahead of print]
F.J. de Paula, M.C. Horowitz, C.J. Rosen, Novel insights into the relationship between diabetes and osteoporosis. Diabet. Metab. Res. Rev. 26, 622–630 (2010)
K. Fulzele, D.J. DiGirolamo, Z. Liu, J. Xu, J.L. Messina, T.L. Clemens, Disruption of the insulin-like growth factor type 1 receptor in osteoblasts enhances insulin signaling and action. J. Biol. Chem. 282, 25649–25658 (2007)
M. Ferron, J. Wei, T. Yoshizawa, A. Del Fattore, R.A. DePinho, A. Teti, P. Ducy, G. Karsenty, Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell 142, 296–308 (2010)
J. Jortay, M. Senou, M. Abou-Samra, L. Noel, A. Robert, M.C. Many, S.M. Brichard, Adiponectin and skeletal muscle: pathophysiological implications in metabolic stress. Am. J. Pathol. 181, 245–256 (2012)
G. Karsenty, Convergence between bone and energy homeostases: leptin regulation of bone mass. Cell Metab. 4, 341–348 (2006)
L. Fu, M.S. Patel, G. Karsenty, The circadian modulation of leptin-controlled bone formation. Prog. Brain Res. 153, 177–188 (2006)
T.D. Challa, Y. Rais, E.M. Ornan, Effect of adiponectin on ATDC5 proliferation, differentiation and signaling pathways. Mol. Cell. Endocrinol. 323, 282–291 (2010)
L. Basurto, R. Galvan, N. Cordova, R. Saucedo, C. Vargas, S. Campos, E. Halley, F. Avelar, A. Zarate, Adiponectin is associated with low bone mineral density in elderly men. Eur. J. Endocrinol. 160, 289–293 (2009)
J.B. Richards, A.M. Valdes, K. Burling, U.C. Perks, T.D. Spector, Serum adiponectin and bone mineral density in women. J. Clin. Endocrinol. Metab. 92, 1517–1523 (2007)
K.W. Oh, W.Y. Lee, E.J. Rhee, K.H. Baek, K.H. Yoon, M.I. Kang, E.J. Yun, C.Y. Park, S.H. Ihm, M.G. Choi, H.J. Yoo, S.W. Park, The relationship between serum resistin, leptin, adiponectin, ghrelin levels and bone mineral density in middle-aged men. Clin. Endocrinol. 63, 131–138 (2005)
M.R. Araneta, D. von Muhlen, E. Barrett-Connor, Sex differences in the association between adiponectin and BMD, bone loss, and fractures: the Rancho Bernardo study. J. Bone Miner. Res. 24, 2016–2022 (2009)
E. Biver, C. Salliot, C. Combescure, L. Gossec, P. Hardouin, I. Legroux-Gerot, B. Cortet, Influence of adipokines and ghrelin on bone mineral density and fracture risk: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 96, 2703–2713 (2011)
G.A. Williams, Y. Wang, K.E. Callon, M. Watson, J.M. Lin, J.B. Lam, J.L. Costa, A. Orpe, N. Broom, D. Naot, I.R. Reid, J. Cornish, In vitro and in vivo effects of adiponectin on bone. Endocrinology 150, 3603–3610 (2009)
X.H. Luo, L.J. Guo, H. Xie, L.Q. Yuan, X.P. Wu, H.D. Zhou, E.Y. Liao, Adiponectin stimulates RANKL and inhibits OPG expression in human osteoblasts through the MAPK signaling pathway. J. Bone Miner. Res. 21, 1648–1656 (2006)
H.W. Lee, S.Y. Kim, A.Y. Kim, E.J. Lee, J.Y. Choi, J.B. Kim, Adiponectin stimulates osteoblast differentiation through induction of COX2 in mesenchymal progenitor cells. Stem Cells 27, 2254–2262 (2009)
Q. Tu, J. Zhang, L.Q. Dong, E. Saunders, E. Luo, J. Tang, J. Chen, Adiponectin inhibits osteoclastogenesis and bone resorption via APPL1-mediated suppression of Akt1. J. Biol. Chem. 286, 12542–12553 (2011)
X.H. Luo, L.J. Guo, L.Q. Yuan, H. Xie, H.D. Zhou, X.P. Wu, E.Y. Liao, Adiponectin stimulates human osteoblasts proliferation and differentiation via the MAPK signaling pathway. Exp. Cell Res. 309, 99–109 (2005)
M. Kawai, C.J. Rosen, The IGF-I regulatory system and its impact on skeletal and energy homeostasis. J. Cell. Biochem. 111, 14–19 (2010)
R. Tenta, M.D. Kontogianni, N. Yiannakouris, Association between circulating levels of adiponectin and indices of bone mass and bone metabolism in middle-aged post-menopausal women. J. Endocrinol. Invest. 35, 306–311 (2012)
I. Kanazawa, T. Yamaguchi, T. Sugimoto, Baseline serum total adiponectin level is positively associated with changes in bone mineral density after 1-year treatment of type 2 diabetes mellitus. Metabolism 59, 1252–1256 (2010)
I. Kanazawa, T. Yamaguchi, M. Yamauchi, M. Yamamoto, S. Kurioka, S. Yano, T. Sugimoto, Adiponectin is associated with changes in bone markers during glycemic control in type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 94, 3031–3037 (2009)
J. Cornish, K.E. Callon, U. Bava, C. Lin, D. Naot, B.L. Hill, A.B. Grey, N. Broom, D.E. Myers, G.C. Nicholson, I.R. Reid, Leptin directly regulates bone cell function in vitro and reduces bone fragility in vivo. J. Endocrinol. 175, 405–415 (2002)
T. Thomas, B. Burguera, Is leptin the link between fat and bone mass? J. Bone Miner. Res. 17, 1563–1569 (2002)
G. Karsenty, F. Oury, The central regulation of bone mass, the first link between bone remodeling and energy metabolism. J. Clin. Endocrinol. Metab. 95, 4795–4801 (2010)
R.S. Ahima, J.S. Flier, Adipose tissue as an endocrine organ. Trends Endocrinol. Metab. 11, 327–332 (2000)
K.J. Motyl, C.J. Rosen, Understanding leptin-dependent regulation of skeletal homeostasis. Biochimie 94, 2089–2096 (2012)
K.E. Barbour, J.M. Zmuda, R. Boudreau, E.S. Strotmeyer, M.J. Horwitz, R.W. Evans, A.M. Kanaya, T.B. Harris, D.C. Bauer, J.A. Cauley, Adipokines and the risk of fracture in older adults. J. Bone Miner. Res. 26, 1568–1576 (2011)
J.M. Lin, D. Naot, M. Watson, J.L. Costa, I.R. Reid, J. Cornish, A. Grey, Skeletal actions of fasting-induced adipose factor (FIAF). Endocrinology 154, 4685–4694 (2013)
L. Wattanachanya, W.D. Lu, R.K. Kundu, L. Wang, M.J. Abbott, D. O’Carroll, T. Quertermous, R.A. Nissenson, Increased bone mass in mice lacking the adipokine apelin. Endocrinology 154, 2069–2080 (2013)
L. Thommesen, A.K. Stunes, M. Monjo, K. Grosvik, M.V. Tamburstuen, E. Kjobli, S.P. Lyngstadaas, J.E. Reseland, U. Syversen, Expression and regulation of resistin in osteoblasts and osteoclasts indicate a role in bone metabolism. J. Cell. Biochem. 99, 824–834 (2006)
H. Zhang, H. Xie, Q. Zhao, G.Q. Xie, X.P. Wu, E.Y. Liao, X.H. Luo, Relationships between serum adiponectin, apelin, leptin, resistin, visfatin levels and bone mineral density, and bone biochemical markers in post-menopausal Chinese women. J. Endocrinol. Invest. 33, 707–711 (2010)
H. Xie, S.Y. Tang, X.H. Luo, J. Huang, R.R. Cui, L.Q. Yuan, H.D. Zhou, X.P. Wu, E.Y. Liao, Insulin-like effects of visfatin on human osteoblasts. Calcif. Tissue Int. 80, 201–210 (2007)
A.R. Moschen, S. Geiger, R. Gerner, H. Tilg, Pre-B cell colony enhancing factor/NAMPT/visfatin and its role in inflammation-related bone disease. Mutat. Res. 690, 95–101 (2010)
H. Xie, P.L. Xie, X.H. Luo, X.P. Wu, H.D. Zhou, S.Y. Tang, E.Y. Liao, Omentin-1 exerts bone-sparing effect in ovariectomized mice. Osteoporos. Int. 23, 1425–1436 (2012)
B.K. Tan, S. Pua, F. Syed, K.C. Lewandowski, J.P. O’Hare, H.S. Randeva, Decreased plasma omentin-1 levels in Type 1 diabetes mellitus. Diabet. Med. 25, 1254–1255 (2008)
B.K. Tan, R. Adya, S. Farhatullah, K.C. Lewandowski, P. O’Hare, H. Lehnert, H.S. Randeva, Omentin-1, a novel adipokine, is decreased in overweight insulin-resistant women with polycystic ovary syndrome: ex vivo and in vivo regulation of omentin-1 by insulin and glucose. Diabetes 57, 801–808 (2008)
D.T. Villareal, C.M. Apovian, R.F. Kushner, S. Klein, Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Am. J. Clin. Nutr. 82, 923–934 (2005)
R. Armamento-Villareal, C. Sadler, N. Napoli, K. Shah, S. Chode, D.R. Sinacore, C. Qualls, D.T. Villareal, Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. J. Bone Miner. Res. 27, 1215–1221 (2012)
I.A. Hosny, H.S. Elghawabi, W.B. Younan, A.A. Sabbour, M.A. Gobrial, Beneficial impact of aerobic exercises on bone mineral density in obese premenopausal women under caloric restriction. Skeletal Radiol. 41, 423–427 (2012)
K. Shah, R. Armamento-Villareal, N. Parimi, S. Chode, D.R. Sinacore, T.N. Hilton, N. Napoli, C. Qualls, D.T. Villareal, Exercise training in obese older adults prevents increase in bone turnover and attenuates decrease in hip bone mineral density induced by weight loss despite decline in bone-active hormones. J. Bone Miner. Res. 26, 2851–2859 (2011)
D.T. Villareal, L. Fontana, E.P. Weiss, S.B. Racette, K. Steger-May, K.B. Schechtman, S. Klein, J.O. Holloszy, Bone mineral density response to caloric restriction-induced weight loss or exercise-induced weight loss: a randomized controlled trial. Arch. Intern. Med. 166, 2502–2510 (2006)
M. Cifuentes, C.S. Riedt, R.E. Brolin, M.P. Field, R.M. Sherrell, S.A. Shapses, Weight loss and calcium intake influence calcium absorption in overweight postmenopausal women. Am. J. Clin. Nutr. 80, 123–130 (2004)
I.R. Reid, Relationships among body mass, its components, and bone. Bone 31, 547–555 (2002)
R.T. Brookheart, C.I. Michel, J.E. Schaffer, As a matter of fat. Cell Metab. 10, 9–12 (2009)
R.W. Schwenk, H. Vogel, A. Schurmann, Genetic and epigenetic control of metabolic health. Mol. Metabol. 2, 337–347 (2013)
R.J. Fajardo, L. Karim, V.I. Calley, M.L. Bouxsein, A Review of Rodent Models of Type 2 Diabetic Skeletal Fragility. J. Bone Miner. Res. (2014). doi:10.1002/jbmr.2210
T. Ong, O. Sahota, W. Tan, L. Marshall, A United Kingdom perspective on the relationship between body mass index (BMI) and bone health: a cross sectional analysis of data from the Nottingham Fracture Liaison Service. Bone 59, 207–210 (2014)
B. Tran, N.D. Nguyen, J.R. Center, J.A. Eisman, T.V. Nguyen, Association between fat-mass-and-obesity-associated (FTO) gene and hip fracture susceptibility. Clin. Endocrinol. (2013). 10.1111/cen.12335
L. McCabe, J. Zhang, S. Raehtz, Understanding the skeletal pathology of type 1 and 2 diabetes mellitus. Crit. Rev. Eukaryot. Gene Expr. 21, 187–206 (2011)
G.A. Brockmann, N. Schafer, C. Hesse, S. Heise, C. Neuschl, A. Wagener, G.A. Churchill, R. Li, Relationship between obesity phenotypes and genetic determinants in a mouse model for juvenile obesity. Physiol. Genomics 45, 817–826 (2013)
A. Krings, S. Rahman, S. Huang, Y. Lu, P.J. Czernik, B. Lecka-Czernik, Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone 50, 546–552 (2012)
G. Musso, Non-alcoholic fatty liver, adipose tissue, and the bone: a new triumvirate on the block. Endocrine 42, 237–239 (2012)
B. Havekes, H.P. Sauerwein, Adipocyte-myocyte crosstalk in skeletal muscle insulin resistance; is there a role for thyroid hormone? Curr. Opin. Clin. Nutr. Metab. Care 13, 641–646 (2010)
C.B. Confavreux, R.L. Levine, G. Karsenty, A paradigm of integrative physiology, the crosstalk between bone and energy metabolisms. Mol. Cell. Endocrinol. 310, 21–29 (2009)
Y.C. Hwang, I.K. Jeong, K.J. Ahn, H.Y. Chung, Circulating osteocalcin level is associated with improved glucose tolerance, insulin secretion and sensitivity independent of the plasma adiponectin level. Osteoporos. Int. 23, 1337–1342 (2012)
A. Aoki, T. Muneyuki, M. Yoshida, H. Munakata, S.E. Ishikawa, H. Sugawara, M. Kawakami, M. Kakei, Circulating osteocalcin is increased in early-stage diabetes. Diabet. Res. Clin. Pract. 92, 181–186 (2011)
I. Kanazawa, T. Yamaguchi, M. Yamauchi, M. Yamamoto, S. Kurioka, S. Yano, T. Sugimoto, Serum undercarboxylated osteocalcin was inversely associated with plasma glucose level and fat mass in type 2 diabetes mellitus. Osteoporos. Int. 22, 187–194 (2011)
J.R. Villafan-Bernal, S. Sanchez-Enriquez, J.F. Munoz-Valle, Molecular modulation of osteocalcin and its relevance in diabetes (Review). Int. J. Mol. Med. 28, 283–293 (2011)
H.T. Viljakainen, M. Pekkinen, E. Saarnio, H. Karp, C. Lamberg-Allardt, O. Makitie, Dual effect of adipose tissue on bone health during growth. Bone 48, 212–217 (2011)
M. Di Monaco, C. Castiglioni, F. Vallero, R. Di Monaco, R. Tappero, Parathyroid hormone is significantly associated with body fat compartment in men but not in women following a hip fracture. Aging Clin. Exp. Res. 25, 371–376 (2013)
E. Ishimura, S. Okuno, N. Tsuboniwa, K. Norimine, S. Fukumoto, K. Yamakawa, T. Yamakawa, S. Shoji, Y. Nishizawa, M. Inaba, Significant positive association between parathyroid hormone and fat mass and lean mass in chronic hemodialysis patients. J. Clin. Endocrinol. Metab. 98, 1264–1270 (2013)
M.F. McCarty, C.A. Thomas, PTH excess may promote weight gain by impeding catecholamine-induced lipolysis-implications for the impact of calcium, vitamin D, and alcohol on body weight. Med. Hypotheses 61, 535–542 (2003)
A.P. Sage, J. Lu, E. Atti, S. Tetradis, M.G. Ascenzi, D.J. Adams, L.L. Demer, Y. Tintut, Hyperlipidemia induces resistance to PTH bone anabolism in mice via oxidized lipids. J. Bone Miner. Res. 26, 1197–1206 (2011)
A. Bellia, G. Marinoni, M. D’Adamo, V. Guglielmi, M. Lombardo, G. Donadel, P. Gentileschi, D. Lauro, M. Federici, R. Lauro, P. Sbraccia, Parathyroid hormone and insulin resistance in distinct phenotypes of severe obesity: a cross-sectional analysis in middle-aged men and premenopausal women. J. Clin. Endocrinol. Metab. 97, 4724–4732 (2012)
M. Di Monaco, C. Castiglioni, F. Vallero, R. Di Monaco, R. Tappero, Parathyroid hormone response to severe vitamin D deficiency is sex associated: an observational study of 571 hip fracture inpatients. J. Nutr. Health Aging 17, 180–184 (2013)
M. Di Monaco, F. Vallero, R. Di Monaco, R. Tappero, A. Cavanna, Fat mass and skeletal muscle mass in hip-fracture women: a cross-sectional study. Maturitas 56, 404–410 (2007)
M. Romero, A. Ortega, N. Olea, M.I. Arenas, A. Izquierdo, J. Bover, P. Esbrit, R.J. Bosch, Novel role of parathyroid hormone-related protein in the pathophysiology of the diabetic kidney: evidence from experimental and human diabetic nephropathy. J. Diabet. Res. 2013, 162846 (2013)
J.J. Wysolmerski, Parathyroid hormone-related protein: an update. J. Clin. Endocrinol. Metab. 97, 2947–2956 (2012)
X.L. Ye, C.F. Lu, Association of polymorphisms in the leptin and leptin receptor genes with inflammatory mediators in patients with osteoporosis. Endocrine 44, 481–488 (2013)
Acknowledgments
The author was partially supported by the grants from The Office of The Vice President for Research (OVPR), Cardiovascular Research Institute (CVRI), and Institutional funding, Wayne State University, during writing of this manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Datta, N.S. Muscle–bone and fat–bone interactions in regulating bone mass: do PTH and PTHrP play any role?. Endocrine 47, 389–400 (2014). https://doi.org/10.1007/s12020-014-0273-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0273-3