Abstract
Renalase is a novel, recently identified, flavin adenine dinucleotide-dependent amine oxidase. It is secreted by the kidney and metabolizes circulating catecholamines. Renalase has significant hemodynamic effects, therefore it is likely to participate in the regulation of cardiovascular function.The aim of our study was to investigate the involvement of renalase gene polymorphisms in hypertension in type 2 diabetes patients. A total of 892 patients and 400 controls were genotyped with three SNPs in the renalase gene. The C allele of rs2296545 SNP was associated with hypertension (P < 0.01). For rs2576178 SNP, frequencies in hypertensive patients differed from controls, but not from normotensive patients. For rs10887800 SNP, the differences in the G allele frequencies were observed in hypertensive patients with stroke, with 66% of patients being GG homozygotes. To confirm observed association we later genotyped 130 stroke patients without diabetes. The OR for risk allele was 1.79 (95% CI 1.33–2.41). In conclusion, the renalase gene polymorphism was associated with hypertension in type 2 diabetes patients. The most interesting result is a strong association of the rs10887800 polymorphism with stroke in patients with and without diabetes. The G allele of this polymorphism might thus be useful in identifying diabetes patients at increased risk of stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
About 70% of mortality in diabetic patients is secondary to coexisting cardiovascular disease (Mazzone 2007). Hypertension is a major risk factor for various cardiovascular diseases, including coronary heart disease and stroke (Kannel 2000).Hypertension is a common comorbidity in individuals with type 2 diabetes and a major risk factor for macro- and microvascular complications (Sowers et al. 2001; Sowers 2004; Derosa et al. 2006; Aronow 2008; Wong et al. 2010). The relationship between diabetes and hypertension has not been completely elucidated. The manifestation and severity of hypertension depend on inherited predisposition combined with environmental factors. Identification of factors for genetic risk of hypertension is thus essential for risk prediction of cardiovascular disease and/or diabetes. Several genes have shown association with essential hypertension either in the candidate gene studies or GWAS but the results have often been discordant (Cowley 2006; Sharma and McNeill 2006; Puddu et al. 2007; Adeyemo et al. 2009).
Renalase is a novel, recently identified, flavin adenine dinucleotide-dependent amine oxidase (Xu et al. 2005). Renalase is secreted by the kidney and metabolizes circulating catecholamines. It has significant hemodynamic effects, therefore it is likely to participate in the regulation of cardiovascular function. Animal studies showed a dose-dependent reduction in blood pressure, heart rate, myocardial contractility, and vascular tone (Li et al. 2008; Gu et al. 2011; Wu et al. 2011).
Recent experimental data strongly support the hypothesis that renalase regulates blood pressure and is important in the pathogenesis of hypertension (Desir 2007; Li et al. 2008; Desir 2011; Wu et al. 2011).
Human renalase is encoded by a gene on chromosome 10 (10q23.33). The renalase gene, encompassing 311,000 bp, has 10 exons (Desir 2008). It was reported to affect risk of type 1 diabetes (Barrett et al. 2009; Reddy et al. 2011) and considered a novel candidate gene for type 2 diabetes (Rampersaud et al. 2007). A recently published study reported association of the renalase gene polymorphisms with essential hypertension (Zhao et al. 2007). The authors examined eight single nucleotide polymorphisms (SNPs) of the renalase gene among 1,317 hypertensive individuals and 1,269 normotensive controls from the International Collaborative Study of Cardiovascular Disease in Asia. Two of the analyzed SNPs were significantly associated with essential hypertension. These results support the theory that renalase plays an important role in the development and maintenance of hypertension. If replicated, they may provide novel genetic susceptibility markers for hypertension.
The purpose of our preliminary study was to investigate the potential involvement of the renalase gene polymorphisms in hypertension in type 2 diabetes patients. Later in the study the cohort of patients with stroke but no diabetes was included to confirm observed association of the renalase gene SNP with stroke. The SNPs selected for our study are located in putative functional regions. One SNP (rs2296545) results in an amino-acid substitution (Asp37Glu) and might affect the function of the gene product. The other two SNPs are at the 5′ flanking region (rs2576178) and near exon/intron boundary (rs10887800) and might affect gene regulation and expression.
Materials and Methods
Study Population and Design
The present investigation was designed to analyze the renalase gene polymorphisms in type 2 diabetes (T2DM) patients with and without hypertension. To compare the prevalence of polymorphisms in patients with a healthy population, we studied a control group of healthy individuals. Later in the study an additional group of patients with stroke was included to confirm the observed association.
The study population (cases) consisted of 892 unrelated T2DM patients, consecutively enrolled between January 2004 and September 2008. The recruited patients were referred by physicians from the Departments of Internal Diseases, Endocrinology and Nephrology and the outpatient Diabetes Clinic of Medical University. They were enrolled without selection for any complications of diabetes or coexisting diseases. All subjects were Caucasians of Polish origin. Diabetes was diagnosed according to American Diabetes Association criteria. For the diagnosis one or more of the following conditions were met: the presence of classic symptoms of hyperglycemia (polyuria, polydipsia, weight loss), fasting plasma glucose ≥126 mg/dl or random plasma glucose ≥200 mg/dl, the use of insulin or oral hypoglycemic agents. The mean duration of diabetes was 12.9 years (range 8–26). It was estimated from time of the first symptoms attributable to the disease or from time of first detection of glycosuria. The mean level of HbA1c was 8.8%. In the patient group 681 individuals (76%) were hypertensive. Hypertension was defined according to World Health Organization criteria (WHO 1999). All patients had persistent systolic blood pressure >140 mm Hg and diastolic blood pressure >90 mm Hg and/or were receiving anti-hypertensive treatment. The secondary hypertension was excluded by clinical and laboratory examination. In the studied patient population with long lasting T2DM, 41% had a diabetic renal disease and almost 46% had diabetic retinopathy.
A positive family history of diabetes in first-degree relatives was reported by 218 patients (24%).
Glycemic control was evaluated by measuring glycated HbA1c levels by turbidimetric inhibition immunoassay (TINIA) using Tina-quant hemoglobin A1cII (Roche-Hitachi 747). All other biochemical parameters were measured by standard laboratory procedures.
Patients with stroke but without diabetes (n = 130) were included later in the study to confirm the association of the SNP in renalase gene with stroke, observed in diabetic patients. They were hospitalized in the Stroke Unit of Department of Neurology. Among this group 112 patients had ischemic stroke and 18 had hemorrhagic stroke.
Healthy subjects (controls) (n = 400) were normotensive volunteers (mostly blood donors and hospital staff members) with no history of diabetes or hypertension. Their systolic and diastolic blood pressure was less than 140 and 90 mm Hg, respectively. Written informed consent was obtained from all subjects in accordance with principles of the Declaration of Helsinki. The protocol of the study was approved by the institutional ethics committee.
Genotype Determination
We analyzed two SNPs that were found to be associated with hypertension in the Asian study (Zhao et al. 2007) and one (rs10887800) of those that were not associated, for a potential confirmation of negative result as well.
Genomic DNA was extracted from peripheral blood leukocytes (obtained from EDTA anticoagulated blood) using a technique from Madisen et al. (1987), with modifications.
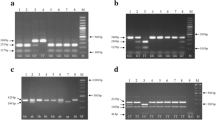
Genotypes for three SNPs in the renalase gene region (dbSNP accession numbers: rs2576178, rs10887800 and rs2296545) were determined by the PCR–RFLP method.
The following primers were used : for rs2296545 forward 5′-GGAAGTCCCCGATCACGTGAC-3′ and reverse 5′-TGCTGTGTGGGACAAGGCTGA-3′; for rs2576178 forward 5′-AGCAGAGAAGCAGCTTAACCT-3′ and reverse 5′-TTATCTGCAAGTCAGCGTAAC-3′ and for rs10887800 forward 5′-CAGGAAAGAAAGAGTTGACAT-3′ and reverse 5′-AAGTTGTTCCAGCTACTGT-3′ Genomic DNA (200 ng) was amplified in a final volume of 30 μl, containing 10 mM TRIS pH 8.3, 50 mM KCl, 1.5 mM MgCl2, 200 μM each dNTP, 1 μM of each primer and 2 U Taq polymerase (all reagents from MBI Fermentas, St. Leon-Rot, Germany). The initial denaturation at 95°C was followed by 35 cycles of denaturation at 94°C, annealing at 60°C, extension at 72°C, 1 min. each and a final extension at 72°C for 7 min. The PCR products (10 μl) were digested for 6–10 h with 5 U of Eco81 I, Msp I and Pst I restriction endonucleases, respectively (MBI Fermentas) at 37°C. Fragments were analyzed on 2.5% agarose gel.
The quality of genotyping was controlled by using blind DNA duplicates for some samples (96). Also, for all SNPs, 30 samples were randomly selected for each genotype and the PCR products were sequenced with the forward primers by automated sequencing in CEQ 8000 Genetic Analysis System (Beckman Coulter).
Statistical Analysis
Statistical calculations were performed using SPSS 11.0 for Windows (SPSS, Inc., Chicago, IL, USA). For baseline characteristics the normally distributed continuous variables are presented as means ± SD. The Hardy–Weinberg equilibrium was tested with the Χ2 test. Genotype distribution and allele frequencies were compared between groups using a Χ2 test of independence with 2 × 2 contingency and z statistics. Student’s t test and Mann–Whitney test were used for statistical significance. Where appropriate, the odds ratios (OR) with corresponding 95% confidence intervals (CI) were calculated. An interaction of the polymorphisms with hypertension, stroke and various risk factors was examined with multiple logistic regression analysis. A two-tailed type I error rate of 5% was considered statistically significant. Power calculations were done using on-line available power calculator (http://calculators.stat.ucla.edu).
Results
The genotypes of three renalase gene polymorphisms: rs2576178 (5′ flanking region), rs10887800 (intron 6) and rs2296545 (exon 2) were determined in 892 patients with type 2 diabetes, 130 patients with stroke and 400 healthy individuals. The genotyping error rate in the total of 366 samples checked was <0.27%. The demographic and clinical characteristics of all groups are presented in Table 1. As expected, subjects with diabetes had a higher mean BMI, were more likely to have a family history of diabetes in a first-degree relative and had a higher mean values of total cholesterol. There were no statistically significant differences in demographic profile between T2DM subjects with hypertension and those without. The mean age was 59.9 ± 16 for patients with hypertension and 60.3 ± 18 for those without and male to female ratio was 1.17 in both subgroups.
Genotype distribution and allele frequencies of three renalase gene polymorphisms were compared in subgroups of T2DM patients with and without hypertension. Genotyping results for the rs2296545 and rs2576178 polymorphisms are summarized in Table 2. The rs2296545 SNP was inconsistent with HWE in T2DM subjects with hypertension (P < 0.0001) The frequency of the C allele of this polymorphism was significantly higher in diabetes patients with hypertension than in normotensive subgroup and healthy controls (P < 0.01). Genotype distribution was also different between patients with hypertension and controls (P < 0.001). For the rs2576178 SNP the genotype distribution in all patient subgroups and controls was in HWE. The genotype distribution in the entire group of patients with diabetes was different from healthy controls, but there was no difference between hypertensive and normotensive patients.
Patients and controls were classified by their genotypes of rs2296545 and rs2576178 SNPs and relationship between clinical and biochemical parameters and genotype was analyzed. The following parameters were examined :age, % males, age at diagnosis, systolic and diastolic blood pressure, BMI, HbA1c, total cholesterol, triglycerides and creatinine. No statistically significant associations were observed between genotypes and studied parameters (all p values in a range 0.092–0.873) (data not shown).
A multivariate logistic regression analysis was performed with the renalase gene genotype and crucial clinical parameters as independent variables and the hypertension status as dependent variable. The results showed that after confounding effects of age, gender, BMI and lipid profile were adjusted, the renalase rs2296545 genotype was significantly and independently associated with hypertension in diabetic patients (OR 2.58, 95% CI 1.231–4.067, P 0.0093).
The distribution of genotypes and alleles of the rs10887800 polymorphism is shown in Table 3. This SNP deviated slightly from HWE proportions in T2DM patients without hypertension (P = 0.034). The frequencies of the G allele were similar in hypertensive patients and controls (0.49 and 0.48, respectively). Normotensive patients showed slightly lower frequency of this allele (0.44). The significant differences in the distribution of this polymorphism were seen in hypertensive patients with a history of stroke. Out of 681 diabetes patients with hypertension, 41 had a history of stroke. The G allele frequency in this subgroup was 0.80. Among174 GG homozygotes observed in all hypertensive patients, 28 were stroke survivors.
To confirm this observed association we also included in our study a group of 130 stroke patients without diabetes. In this group the frequency of the risk allele was 0.62. The odds ratio (OR) for the G allele was 1.79 (95% CI 1.33–2.41). Eighty-seven percent of these patients with stroke were G allele carriers.
The presence of the G allele did not show any statistically significant association with gender, diabetes duration, BMI or cholesterol.
Discussion
The renalase gene is a reasonable candidate to be potentially involved in blood pressure regulation. In a large study on the potential association of renalase gene polymorphisms with human hypertension eight SNPs were examined. The results suggested that genetic variants in the renalase gene may influence the susceptibility to essential hypertension in the northern Han Chinese population The authors studied common single nucleotide variations, with minor allele frequencies (MAF) ≥0.05 (Zhao et al. 2007).
In our study patients with T2DM, patients with stroke and healthy individuals were genotyped with three SNPs in the renalase gene : rs2576178 (MAF = 0.48) and rs2296545 (MAF = 0.44) which in Zhao’s study were associated with hypertension (Zhao et al. 2007) and in addition rs10887800. The frequencies of genotypes and alleles for rs2296545 and rs10887800 were similar to those observed in Zhao’s study but different for the rs2576178 SNP. Minor allele frequencies in our study were 0.48 for rs2296545 and 0.48 for rs10887800.
We observed that the frequency of the C allele of rs2296545 polymorphism was also higher in diabetes patients with hypertension than in patients without hypertension and controls. This suggests that in Polish population, at least in diabetic patients, the C allele of this polymorphism is also associated with susceptibility to hypertension. This polymorphism might affect the function of the gene product but it also might be nonfunctional but in the tight linkage disequilibrium with another functional variant. This needs further functional studies. However, because the rs2296545 SNP shows substantial deviation from HWE estimates (P < 0.0001) in T2DM patients with hypertension, these results should be viewed with caution. The genotyping errors can be excluded since the quality of genotyping in our study was carefully controlled with using blind sample duplicates and direct sequencing. The likely reason for the deviation from HWE may be the selection bias.
Regarding the rs2576178 polymorphism, there was no significant difference in the genotype/allele distribution between hypertensive and normotensive patients. If the effect of the G allele is small, this result might be due to the relatively small size of our normotensive patient subgroup. There was a significant difference in the G allele frequency of this SNP between our and Zhao’s studies (0.30 and 0.52, respectively, compared to 0.356 in NCBI dbSNP), thus the genetic heterogeneity across populations might also partially explain the discrepancy between Zhao’s and our results. The G allele and GG genotype frequencies of rs2576178 SNP were higher in the entire group of diabetic patients than in controls which might suggest an association of renalase gene SNP with diabetes itself. This would require further studies in a larger patient population to draw such conclusion. The association of the renalase gene locus with type 2 diabetes was earlier observed in a genome-wide association scan in the Amish population (Rampersaud et al. 2007).
The rs10887800 polymorphism was not associated with hypertension in Zhao’s study. In our study the frequencies of the G allele were also similar in hypertensive patients and controls. However, the significant difference was observed in the hypertensive diabetes patients who had a stroke (6% of all hypertensive patients). The G allele frequency in those patients was 1.63 times higher than in all hypertensive patients and 95% of patients with stroke were G allele carriers. To confirm this association we genotyped patients with stroke but no diabetes with this polymorphism. The frequency of the G allele was high in this group, with the odds ratio for this risk allele 1.79 (95% CI 1.33–2.41). This suggests that the G allele might be a risk factor for stroke in hypertensive individuals. The mechanism of this is not clear. Stroke is a multifactorial polygenic disease controlled by multiple genetic and environmental factors. Hypertension is one of important stroke risk predictors and it contributes significantly to the onset of disease (Rohr et al. 1996). These two conditions might share the same etiopathogenesis. The candidate genes for hypertension might be involved in stroke pathogenesis as well but they may have different impact depending on other, nongenetic risk factors (Matarin et al. 2010). There is a possibility that observed association of renalase gene with stroke could be related to more severe hypertension. However, at present there are no data reported indicating that any particular genotypes of renalase gene polymorphisms affect the severity of hypertension. In our study we did not observe association between studied SNPs and blood pressure values in stroke patient group. Elaborating this would require a separate study in a larger population of stroke patients.
The results obtained in our study have to be interpreted with caution. The renalase gene is not a typical candidate gene in hypertension and/or cardiovascular disease. The biological mechanisms of any association of gene variants with those diseases are not clear at this point. In addition, our study is a hospital-based case control study and although the sample size is relatively large and homogeneous, the genotyping results should be replicated in future large-scale studies.
In conclusion, our study is the first published study of the association of the renalase gene polymorphisms with hypertension and stroke in European population. The results demonstrate that the renalase gene polymorphism rs2296545 is associated with hypertension in type 2 diabetes patients. The most interesting result is a strong association of the rs10887800 polymorphism with stroke in diabetes patients with hypertension and also in stroke patients without diabetes. The G allele of this polymorphism might thus be useful in identifying diabetes patients and other individuals at the risk of stroke.
References
Adeyemo, A., Gerry, N., Chen, G., Herbert, A., Doumatey, A., Huang, H., et al. (2009). A genome-wide association study of hypertension and blood pressure in African Americans. Public Library of Science Genetics, 5, e1000564.
Aronow, W. S. (2008). Hypertension and the older diabetic. Clinics in Geriatric Medicine, 24, 489–501.
Barrett, J. C., Clayton, D. G., Concannon, P., Akolkar, B., Cooper, J. D., et al. (2009). Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nature Genetics, 41, 703–707.
Cowley, A. W., Jr. (2006). The genetic dissection of essential hypertension. Nature Reviews Genetics, 7, 829–840.
Derosa, G., Salvadeo, S., & Cicero, A. F. (2006). Recommendations for the treatment of hypertension in patients with DM: Critical evaluation based on clinical trials. Current Clinical Pharmacology, 1, 21–33.
Desir, G. V. (2007). Renalase is a novel renal hormone that regulates cardiovascular function. Journal of the American Society of Hypertension, 1, 99–103.
Desir, G. V. (2008). Renalase deficiency in chronic kidney disease, and its contribution to hypertension and cardiovascular disease. Current Opinion in Nephrology and Hypertension, 17, 181–185.
Desir, G. V. (2011). Role of renalase in the regulation of blood pressure and the renal dopamine system. Current Opinion in Nephrology and Hypertension, 20, 31–36.
Gu, R., Lu, W., Xie, J., Bai, J., & Xu, B. (2011). Renalase deficiency in heart failure model of rats–a potential mechanism underlying circulating norepinephrine accumulation. Public Library of Science, 6, e14633.
Kannel, V. B. (2000). Elevated systolic blood pressure as a cardiovascular risk factor. American Journal of Cardiology, 85, 251–255.
Li, G., Xu, J., Wang, P., Velazquez, H., Li, Y., Wu, Y., et al. (2008). Catecholamines regulate the activity, secretion, and synthesis of renalase. Circulation, 117, 1277–1282.
Madisen, L., Hoar, D. I., Holroyd, C. D., Crisp, M., & Hodes, M. E. (1987). The banking : The effects of storage of blood and isolated DNA on the integrity of DNA. American Journal of Medical Genetics, 27, 379–390.
Matarin, M., Singleton, A., Hardy, J., & Meschia, J. (2010). The genetics of ischaemic stroke. Journal of Internal Medicine, 267, 139–155.
Mazzone, T. (2007). Prevention of macrovascular disease in patients with diabetes mellitus: Opportunities for intervention. American Journal of Medicine, 120, S26–S32.
Puddu, P., Puddu, G. M., Cravero, E., Ferrari, E., & Muscari, A. (2007). The genetic basis of essential hypertension. Acta Cardiologica, 62, 281–293.
Rampersaud, E., Damcott, C. M., Fu, M., Shen, H., McArdle, P., et al. (2007). Identification of novel candidate genes for type 2 diabetes from a genome-wide association scan in the old order Amish. Diabetes, 56, 3053–3062.
Reddy, M. V., Wang, H., Liu, S., Bode, B., Reed, J. C., et al. (2011). Association between type 1 diabetes and GWAS SNPs in the southwest US Caucasian population. Genes & Immunity, 12, 208–212.
Rohr, J., Kittner, S., Feeser, B., Hebel, J. R., Whyte, M. G., Weinstein, A., et al. (1996). Traditional risk factors and ischemic stroke in young adults: The Baltimore-Washington Cooperative Young Stroke Study. Archives of Neurology, 53, 603–607.
Sharma, V., & McNeill, J. H. (2006). The etiology of hypertension in the metabolic syndrome part two: The gene environment interaction. Current Vascular Pharmacology, 4, 305–320.
Sowers, J. R. (2004). Insulin resistance and hypertension. American Journal of Physiology. Heart and Circulatory Physiology., 286, H1597–H1602.
Sowers, J. R., Epstein, M., & Frohlich, E. D. (2001). Diabetes, hypertension and cardiovascular disease. An update. Hypertension, 37, 1053–1059.
Wong, W. T., Wong, S. L., Tian, X. Y., & Huang, Y. (2010). Endothelial dysfunction: The common consequence in diabetes and hypertension. Cardiovascular Pharmacology, 55, 300–307.
World Health Organization. International Society of Hypertension Guideline for Management of Hypertension. (1999). Journal of Hypertension, 17, 151–183.
Wu, Y., Xu, J., Velazquez, H., Wang, P., Li, G., Liu, D., et al. (2011). Renalase deficiency aggravates ischemic myocardial damage. Kidney International, 79, 853–860.
Xu, J., Li, G., Wang, P., Velazquez, H., Yao, X., Li, Y., et al. (2005). Renalase is a novel soluble monoamine oxidase that regulates cardiac function and blood pressure. Journal of Clinical Investigation, 115, 1275–1280.
Zhao, Q., Fan, Z., He, J., Chen, S., Li, H., Zhang, P., et al. (2007). Renalase gene is a novel susceptibility gene for essential hypertension: A two-stage association study in northern Han Chinese population. Journal of Molecular Medicine, 85, 877–885.
Acknowledgments
This study was supported in part by the grant DS 379/09 from Medical University of Lublin. The authors thank Ms. Bozenna Jarzabkowska for her skillful technical help.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Buraczynska, M., Zukowski, P., Buraczynska, K. et al. Renalase Gene Polymorphisms in Patients With Type 2 Diabetes, Hypertension and Stroke. Neuromol Med 13, 321–327 (2011). https://doi.org/10.1007/s12017-011-8158-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12017-011-8158-6