Abstract
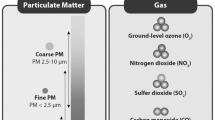
Air pollution is defined as the presence of noxious substances in the air at levels that impose a health hazard. Thus, there has been long-standing interest in the possible role of indoor and outdoor air pollutants on the development of respiratory disease. In this regard, asthma has been of particular interest but many studies have also been conducted to explore the relationship between air pollution, allergic rhinitis, and atopic dermatitis. Traffic-related air pollutants or TRAP refers to a broad group of pollutants including elemental carbon, black soot, nitrogen dioxide (NO2), nitric oxide (NO), sulfur dioxide (SO2), particulate matter (PM2.5 and PM10), carbon monoxide (CO), and carbon dioxide (CO2). In this review, we aim to examine the current literature regarding the impact of early childhood exposure to TRAP on the development of asthma, allergic rhinitis, and atopic dermatitis. Although there is growing evidence suggesting significant associations, definitive conclusions cannot be made with regard to the effect of TRAP on these diseases. This conundrum may be due to a variety of factors, including different definitions used to define TRAP, case definitions under consideration, a limited number of studies, variation in study designs, and disparities between studies in consideration of confounding factors. Regardless, this review highlights the need for future studies to be conducted, particularly with birth cohorts that explore this relationship further. Such studies may assist in understanding more clearly the pathogenesis of these diseases, as well as other methods by which these diseases could be treated.


Similar content being viewed by others
References
USEPA (2016) NArAQS table. Usepa https://www.epa.gov/criteria-air-pollutants/naaqs
Air quality | History of air pollution in the UK. http://www.air-quality.org.uk/02.php. Accessed 7 Feb 2018
Stern AC History of air pollution legislation in the United States. J Air Pollut Control Assoc 32(1):44–61
Safety and health topics | Indoor air quality | Occupational safety and health administration. https://www.osha.gov/SLTC/indoorairquality/. Accessed 7 Feb 2018
Greenbaum D. Traffic-related air pollution: a critical review of the literature on emissions, exposure, and health effects. Presented at the Clean Air Act Advisory Committee. 2009. Crystal City, VA
Products - Data briefs - Number 10 - October 2008. https://www.cdc.gov/nchs/products/databriefs/db10.htm. Accessed 5 Dec 2017
Peterson B, Saxon A (1996) Global increases in allergic respiratory disease: the possible role of diesel exhaust particles. Ann Allergy Asthma Immunol 77:263–270. https://doi.org/10.1016/S1081-1206(10)63318-2
Favarato G, Anderson HR, Atkinson R, Fuller G, Mills I, Walton H (2014) Traffic-related pollution and asthma prevalence in children. Quantification of associations with nitrogen dioxide. Air Qual Atmos Health 7:459–466. https://doi.org/10.1007/s11869-014-0265-8
Hoek G, Beelen R, de Hoogh K, Vienneau D, Gulliver J, Fischer P, Briggs D (2008) A review of land-use regression models to assess spatial variation of outdoor air pollution. Atmos Environ 42:7561–7578. https://doi.org/10.1016/J.ATMOSENV.2008.05.057
Ryan PH, LeMasters GK (2007) A review of land-use regression models for characterizing intraurban air pollution exposure. Inhal Toxicol 19(Suppl 1):127–133. https://doi.org/10.1080/08958370701495998
Kawasaki S, Takizawa H, Takami K, Desaki M, Okazaki H, Kasama T, Kobayashi K, Yamamoto K, Nakahara K, Tanaka M, Sagai M, Ohtoshi T (2001) Benzene-extracted components are important for the major activity of diesel exhaust particles. Am J Respir Cell Mol Biol 24:419–426. https://doi.org/10.1165/ajrcmb.24.4.4085
Takano H, Yoshikawa T, Ichinose T et al (1997) Diesel exhaust particles enhance antigen-induced airway inflammation and local cytokine expression in mice. Am J Respir Crit Care Med 156:36–42. https://doi.org/10.1164/ajrccm.156.1.9610054
Takenaka H, Zhang K, Diaz-Sanchez D, Tsien A, Saxon A (1995) Enhanced human IgE production results from exposure to the aromatic hydrocarbons from diesel exhaust: direct effects on B-cell IgE production. J Allergy Clin Immunol 95:103–115
Fernvik E, Scharnweber T, Knopp D, Niessner R, Vargaftig BB, Peltre G (2002) Effects of fractions of traffic particulate matter on Th2-cytokines, IgE levels, and bronchial hyperresponsiveness in mice. J Toxicol Environ Health A 65:1025–1045. https://doi.org/10.1080/152873902760125200
Diaz-Sanchez D, Garcia MP, Wang M, Jyrala M, Saxon A (1999) Nasal challenge with diesel exhaust particles can induce sensitization to a neoallergen in the human mucosa. J Allergy Clin Immunol 104:1183–1188. https://doi.org/10.1016/S0091-6749(99)70011-4
Salvi S, Blomberg A, Rudell B et al (1999) Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med 159:702–709. https://doi.org/10.1164/ajrccm.159.3.9709083
Salvi SS, Nordenhall C, Blomberg A et al (2000) Acute exposure to diesel exhaust increases IL-8 and GRO-alpha production in healthy human airways. Am J Respir Crit Care Med 161:550–557. https://doi.org/10.1164/ajrccm.161.2.9905052
Nightingale JA, Maggs R, Cullinan P et al (2000) Airway inflammation after controlled exposure to diesel exhaust particulates. Am J Respir Crit Care Med 162:161–166. https://doi.org/10.1164/ajrccm.162.1.9908092
Sehlstedt M, Behndig AF, Boman C, Blomberg A, Sandström T, Pourazar J (2010) Airway inflammatory response to diesel exhaust generated at urban cycle running conditions. Inhal Toxicol 22:1144–1150. https://doi.org/10.3109/08958378.2010.529181
Xu X, Deng F, Guo X, Lv P, Zhong M, Liu C, Wang A, Tzan K, Jiang SY, Lippmann M, Rajagopalan S, Qu Q, Chen LC, Sun Q (2012) Association of systemic inflammation with marked changes in particulate air pollution in Beijing in 2008. Toxicol Lett 212:147–156. https://doi.org/10.1016/j.toxlet.2012.05.014
Kajekar R (2007) Environmental factors and developmental outcomes in the lung. Pharmacol Ther 114:129–145. https://doi.org/10.1016/j.pharmthera.2007.01.011
LeMasters G, Levin L, Bernstein DI, Lockey SD IV, Lockey JE, Burkle J, Khurana Hershey GK, Brunst K, Ryan PH (2015) Secondhand smoke and traffic exhaust confer opposing risks for asthma in normal and overweight children. Obesity 23:32–36. https://doi.org/10.1002/oby.20941
Dong GH, Qian Z, Liu M-M, Wang D, Ren WH, Fu Q, Wang J, Simckes M, Ferguson TF, Trevathan E (2013) Obesity enhanced respiratory health effects of ambient air pollution in Chinese children: the seven northeastern cities study. Int J Obes 37:94–100. https://doi.org/10.1038/ijo.2012.125
Brunst KJ, Ryan PH, Brokamp C, Bernstein D, Reponen T, Lockey J, Khurana Hershey GK, Levin L, Grinshpun SA, LeMasters G (2015) Timing and duration of traffic-related air pollution exposure and the risk for childhood wheeze and asthma. Am J Respir Crit Care Med 192:421–427. https://doi.org/10.1164/rccm.201407-1314OC
Clark NA, Demers PA, Karr CJ, Koehoorn M, Lencar C, Tamburic L, Brauer M (2010) Effect of early life exposure to air pollution on development of childhood asthma. Environ Health Perspect 118:284–290. https://doi.org/10.1289/ehp.0900916
Leon Hsu H-H, Mathilda Chiu Y-H, Coull BA, Kloog I, Schwartz J, Lee A, Wright RO, Wright RJ (2015) Prenatal particulate air pollution and asthma onset in urban children. Identifying sensitive windows and sex differences. Am J Respir Crit Care Med 192:1052–1059. https://doi.org/10.1164/rccm.201504-0658OC
Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, Oldenwening M, Smit HA, Brunekreef B (2010) Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med 181:596–603. https://doi.org/10.1164/rccm.200906-0858OC
Gehring U, Beelen R, Eeftens M, Hoek G, de Hoogh K, de Jongste JC, Keuken M, Koppelman GH, Meliefste K, Oldenwening M, Postma DS, van Rossem L, Wang M, Smit HA, Brunekreef B (2015) Particulate matter composition and respiratory health: the PIAMA birth cohort study. Epidemiology 26:300–309. https://doi.org/10.1097/EDE.0000000000000264
Gruzieva O, Bergström A, Hulchiy O, Kull I, Lind T, Melén E, Moskalenko V, Pershagen G, Bellander T (2013) Exposure to air pollution from traffic and childhood asthma until 12 years of age. Epidemiology 24:54–61. https://doi.org/10.1097/EDE.0b013e318276c1ea
Carlsten C, Dybuncio A, Becker A, Chan-Yeung M, Brauer M (2011) Traffic-related air pollution and incident asthma in a high-risk birth cohort. Occup Environ Med 68:291–295. https://doi.org/10.1136/oem.2010.055152
Fuertes E, Standl M, Cyrys J, Berdel D, von Berg A, Bauer CP, Krämer U, Sugiri D, Lehmann I, Koletzko S, Carlsten C, Brauer M, Heinrich J (2013) A longitudinal analysis of associations between traffic-related air pollution with asthma, allergies and sensitization in the GINIplus and LISAplus birth cohorts. PeerJ 1:e193. https://doi.org/10.7717/peerj.193
Gehring U, Wijga AH, Hoek G, Bellander T, Berdel D, Brüske I, Fuertes E, Gruzieva O, Heinrich J, Hoffmann B, de Jongste JC, Klümper C, Koppelman GH, Korek M, Krämer U, Maier D, Melén E, Pershagen G, Postma DS, Standl M, von Berg A, Anto JM, Bousquet J, Keil T, Smit HA, Brunekreef B (2015) Exposure to air pollution and development of asthma and rhinoconjunctivitis throughout childhood and adolescence: a population-based birth cohort study. Lancet Respir Med 3:933–942. https://doi.org/10.1016/S2213-2600(15)00426-9
Jerrett M, Shankardass K, Berhane K, Gauderman WJ, Künzli N, Avol E, Gilliland F, Lurmann F, Molitor JN, Molitor JT, Thomas DC, Peters J, McConnell R (2008) Traffic-related air pollution and asthma onset in children: a prospective cohort study with individual exposure measurement. Environ Health Perspect 116:1433–1438. https://doi.org/10.1289/ehp.10968
Krämer U, Sugiri D, Ranft U, Krutmann J, von Berg A, Berdel D, Behrendt H, Kuhlbusch T, Hochadel M, Wichmann HE, Heinrich J, GINIplus and LISAplus study groups (2009) Eczema, respiratory allergies, and traffic-related air pollution in birth cohorts from small-town areas. J Dermatol Sci 56:99–105. https://doi.org/10.1016/j.jdermsci.2009.07.014
Lindgren A, Stroh E, Björk J, Jakobsson K (2013) Asthma incidence in children growing up close to traffic: a registry-based birth cohort. Environ Health 12:91. https://doi.org/10.1186/1476-069X-12-91
McConnell R, Islam T, Shankardass K, Jerrett M, Lurmann F, Gilliland F, Gauderman J, Avol E, Künzli N, Yao L, Peters J, Berhane K (2010) Childhood incident asthma and traffic-related air pollution at home and school. Environ Health Perspect 118:1021–1026. https://doi.org/10.1289/ehp.0901232
Mölter A, Agius R, de Vocht F, Lindley S, Gerrard W, Custovic A, Simpson A (2014) Effects of long-term exposure to PM10 and NO2 on asthma and wheeze in a prospective birth cohort. J Epidemiol Community Health 68:21–28. https://doi.org/10.1136/jech-2013-202681
Mölter A, Simpson A, Berdel D, Brunekreef B, Custovic A, Cyrys J, de Jongste J, de Vocht F, Fuertes E, Gehring U, Gruzieva O, Heinrich J, Hoek G, Hoffmann B, Klümper C, Korek M, Kuhlbusch TAJ, Lindley S, Postma D, Tischer C, Wijga A, Pershagen G, Agius R (2015) A multicentre study of air pollution exposure and childhood asthma prevalence: the ESCAPE project. Eur Respir J 45:610–624. https://doi.org/10.1183/09031936.00083614
Morgenstern V, Zutavern A, Cyrys J, Brockow I, Gehring U, Koletzko S, Bauer CP, Reinhardt D, Wichmann HE, Heinrich J (2007) Respiratory health and individual estimated exposure to traffic-related air pollutants in a cohort of young children. Occup Environ Med 64:8–16. https://doi.org/10.1136/oem.2006.028241
Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Krämer U, Behrendt H, Herbarth O, von Berg A, Bauer CP, Wichmann HE, Heinrich J (2008) Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med 177:1331–1337. https://doi.org/10.1164/rccm.200701-036OC
Oftedal B, Nystad W, Brunekreef B, Nafstad P (2009) Long-term traffic-related exposures and asthma onset in schoolchildren in Oslo, Norway. Environ Health Perspect 117:839–844. https://doi.org/10.1289/ehp.11491
Wu T-J, Wu C-F, Chen B-Y, Lee YL, Guo YL (2016) Age of asthma onset and vulnerability to ambient air pollution: an observational population-based study of adults from Southern Taiwan. BMC Pulm Med 16:54. https://doi.org/10.1186/s12890-016-0218-0
Castro-Giner F, Künzli N, Jacquemin B, Forsberg B, de Cid R, Sunyer J, Jarvis D, Briggs D, Vienneau D, Norback D, González JR, Guerra S, Janson C, Antó JM, Wjst M, Heinrich J, Estivill X, Kogevinas M (2009) Traffic-related air pollution, oxidative stress genes, and asthma (ECHRS). Environ Health Perspect 117:1919–1924. https://doi.org/10.1289/ehp.0900589
Lindgren A, Stroh E, Montnémery P, Nihlén U, Jakobsson K, Axmon A (2009) Traffic-related air pollution associated with prevalence of asthma and COPD/chronic bronchitis. A cross-sectional study in Southern Sweden. Int J Health Geogr 8:2. https://doi.org/10.1186/1476-072X-8-2
Lindgren A, Stroh E, Nihlén U, Montnémery P, Axmon A, Jakobsson K (2009) Traffic exposure associated with allergic asthma and allergic rhinitis in adults. A cross-sectional study in southern Sweden. Int J Health Geogr 8:25. https://doi.org/10.1186/1476-072X-8-25
Environmental Protection Agency (2015) Volatile organic compounds’ impact on indoor air quality. https://www.epa.gov/indoor-air-quality-iaq/volatile-organic-compounds-impact-indoor-air-quality#Sources. Accessed 7 Jun 2018
Tunnicliffe WS, Burge PS, Ayres JG (1994) Effect of domestic concentrations of nitrogen dioxide on airway responses to inhaled allergen in asthmatic patients. Lancet 344:1733–1736. https://doi.org/10.1016/S0140-6736(94)92886-X
Van Winkle MR, Scheff PA (2001) INDOOR AIR Volatile organic compounds, polycyclic aromatic hydrocarbons and elements in the air of ten urban homes. Indoor Air C Indoor Air 11:49–64. https://doi.org/10.1034/j.1600-0668.2001.011001049.x
Lin W, Brunkeef B, Gehring U (2013) Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheezing in children. Int J Epidemiol 42(6):1724–1737. https://doi.org/10.1093/ije/dyt150
Arif AA, Shah SM (2007) Association between personal exposure to volatile organic compounds and asthma among US adult population. Int Arch Occup Environ Health 80:711–719. https://doi.org/10.1007/s00420-007-0183-2
Norbäck D, Björnsson E, Janson C et al (1995) Asthmatic symptoms and volatile organic compounds, formaldehyde, and carbon dioxide in dwellings. Occup Environ Med 52:388–395. https://doi.org/10.1136/OEM.52.6.388
Rumchev K, Spickett J, Bulsara M, Phillips M, Stick S (2004) Association of domestic exposure to volatile organic compounds with asthma in young children. Thorax 59:746–751. https://doi.org/10.1136/thx.2003.013680
Nurmatov UB, Tagiyeva N, Semple S, Devereux G, Sheikh A (2015) Volatile organic compounds and risk of asthma and allergy: a systematic review. Eur Respir Rev 24:92–101. https://doi.org/10.1183/09059180.00000714
Smedje G, Norbäck D (2001) Incidence of asthma diagnosis and self-reported allergy in relation to the school environment--a four-year follow-up study in schoolchildren. Int J Tuberc Lung Dis 5:1059–1066
US EPA, OAR,ORIA I Lead’s impact on indoor air quality https://www.epa.gov/indoor-air-quality-iaq/formaldehydes-impact-indoor-air-quality. Accessed 13 Jun 2018
Medical surveillance - formaldehyde - 1910.1048 App C | Occupational safety and health administration. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10078. Accessed 13 Jun 2018
Gilbert NL, Gauvin D, Guay M, Héroux MÈ, Dupuis G, Legris M, Chan CC, Dietz RN, Lévesque B (2006) Housing characteristics and indoor concentrations of nitrogen dioxide and formaldehyde in Quebec City, Canada. Environ Res 102:1–8. https://doi.org/10.1016/j.envres.2006.02.007
Guo H, Kwok NH, Cheng HR, Lee SC, Hung WT, Li YS (2009) Formaldehyde and volatile organic compounds in Hong Kong homes: concentrations and impact factors. Indoor Air 19:206–217. https://doi.org/10.1111/j.1600-0668.2008.00580.x
Casset A, Marchand C, Purohit A, le Calve S, Uring-Lambert B, Donnay C, Meyer P, de Blay F (2006) Inhaled formaldehyde exposure: effect on bronchial response to mite allergen in sensitized asthma patients. Allergy Eur J Allergy Clin Immunol 61:1344–1350. https://doi.org/10.1111/j.1398-9995.2006.01174.x
CDC (2009) Phthalates. Cent Dis Control:1–3
Rudel RA, Perovich LJ (2009) Endocrine disrupting chemicals in indoor and outdoor air. Atmos Environ 43:170–181. https://doi.org/10.1016/j.atmosenv.2008.09.025
Hsu NY, Lee CC, Wang JY, Li YC, Chang HW, Chen CY, Bornehag CG, Wu PC, Sundell J, Su HJ (2012) Predicted risk of childhood allergy, asthma, and reported symptoms using measured phthalate exposure in dust and urine. Indoor Air 22:186–199. https://doi.org/10.1111/j.1600-0668.2011.00753.x
Bertelsen RJ, LØdrup Carlsen KC, Calafat AM et al (2013) Urinary biomarkers for phthalates associated with asthma in Norwegian children. Environ Health Perspect 121:251–256. https://doi.org/10.1289/ehp.1205256
Just AC, Whyatt RM, Miller RL, Rundle AG, Chen Q, Calafat AM, Divjan A, Rosa MJ, Zhang H, Perera FP, Goldstein IF, Perzanowski MS (2012) Children’s urinary phthalate metabolites and fractional exhaled nitric oxide in an urban cohort. Am J Respir Crit Care Med 186:830–837. https://doi.org/10.1164/rccm.201203-0398OC
Gruzieva O, Bellander T, Eneroth K, Kull I, Melén E, Nordling E, van Hage M, Wickman M, Moskalenko V, Hulchiy O, Pershagen G (2012) Traffic-related air pollution and development of allergic sensitization in children during the first 8 years of life. J Allergy Clin Immunol 129(1):240–246
Codispoti CD, LeMaster GK, Levin L et al (2015) Traffic pollution is associated with early childhood aeroallergen sensitization. Ann Allergy Asthma Immunol 114(2):126–133
Jung D, Leem J, Kim H et al (2015) Effect of traffic-related air pollution on allergic disease: results of the children’s health and environmental research. Allergy Asthma Immunol Res 7(4):359–366
Lee YL, Su HJ, Sheu HM, Yu HS, Guo YL (2008) Traffic-related air pollution, climate and prevalence of eczema in Taiwanese school children. J Invest Dermatol 128(10):2412–2420
Penard-Morand C, Raherison C, Charpin D, Kopferschmitt C, Lavaud F, Caillaud D, Annesi-maesano I (2010) Long-term exposure to close-proximity air pollution and asthma and allergies in urban children. Eur Respir J 36:33–40
Morganstern V, Zutavern A, Cyrys J et al (2008) Atopic diseases, allergic sensitizations, exposure to traffic-related air pollution in children. Am J Respir Crit Care Med 177:1331–1337
China’s Olympian efforts to tackle air pollution - SciDevNet https://www.scidev.net/global/pollution/feature/china-s-olympian-efforts-to-tackle-air-pollution.html. Accessed 7 Jun 2018
Environmental hazards - Chapter 2 - 2018 Yellow book | Travelers’ health | CDC. https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/environmental-hazards. Accessed 7 Jun 2018
USEPA (2014) Air quality index (AQI). A guide to air quality your health 12
Funding
This study was funded by the NIAID Allergy Training Grant T32 AI060515 and NIEHS Training Grant T32 ES010957-16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hassoun, Y., James, C. & Bernstein, D.I. The Effects of Air Pollution on the Development of Atopic Disease. Clinic Rev Allerg Immunol 57, 403–414 (2019). https://doi.org/10.1007/s12016-019-08730-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-019-08730-3