Abstract
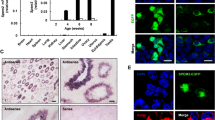
Reproductive health of men has declined in recent past with reduced sperm count and increased incidence of infertility and testicular cancers mainly attributed to endocrine disruption in early life. Present study aims to evaluate whether testicular stem cells including very small embryonic-like stem cells (VSELs) and spermatogonial stem cells (SSCs) get affected by endocrine disruption and result in pathologies in adult life. Effect of treatment on mice pups with estradiol (20 μg on days 5–7) and diethylstilbestrol (DES, 2 μg on days 1–5) was studied on VSELs, SSCs and spermatogonial cells in adult life. Treatment affected spermatogenesis, tubules in Stage VIII & sperm count were reduced along with reduction of meiotic (4n) cells and markers (Prohibitin, Scp3, Protamine). Enumeration of VSELs by flow cytometry (2–6 μm, 7AAD-, LIN-CD45-SCA-1+) and qRT-PCR using specific transcripts for VSELs (Oct-4a, Sox-2, Nanog, Stella, Fragilis), SSCs (tOct-4, Gfra-1, Gpr-125) and early germ cells (Mvh, Dazl) showed several-fold increase but transition from c-Kit negative to c-Kit positive spermatogonial cells was blocked on D100 after treatment. Transcripts specific for apoptosis (Bcl2, Bax) remained unaffected but tumor suppressor (p53) and epigenetic regulator (NP95) transcripts showed marked disruption. 9 of 10 mice exposed to DES showed tumor-like changes. To conclude, endocrine disruption resulted in a tilt towards excessive self-renewal of VSELs (leading to testicular cancer after DES treatment) and blocked differentiation (reduced numbers of c-Kit positive cells, meiosis, sperm count and fertility). Understanding the underlying basis for infertility and cancer initiation from endogenous stem cells through murine modelling will hopefully improve human therapies in future.








Similar content being viewed by others
Abbreviations
- VSELS:
-
very small embryonic-like stem cells
- SSCs:
-
spermatogonial stem cells
- E2:
-
estradiol
- DES:
-
diethylstilbestrol
- TDS:
-
Testicular Dysgenesis Syndrome
- EDCs:
-
endocrine-disrupting chemicals
- FSH:
-
follicle stimulating hormone
- E:
-
estrogen
- T:
-
testosterone
- LH:
-
luteinizing hormone
- PBS:
-
phosphate buffer saline
- FBS:
-
fetal bovine serum
- CIS:
-
carcinoma in situ
References
GBD 2017 Population and Fertility Collaborators. (2018). Population and fertility by age and sex for 195 countries and territories, 1950-2017: A systematic analysis for the global burden of disease study 2017. Lancet, 392(10159), 1995–2051.
Sumner, R. N., Tomlinson, M., Craigon, J., England, G. C. W., & Lea, R. G. (2019). Independent and combined effects of diethylhexyl phthalate and polychlorinated biphenyl 153 on sperm quality in the human and dog. Scientific Reports, 9, 3409.
De Toni, L., Šabovic, I., Cosci, I., Ghezzi, M., Foresta, C., & Garolla, A. (2019). Testicular cancer: genes, environment, hormones. Front Endocrinol (Lausanne), 10, 408.
Skakkebaek, N. E., Rajpert-De Meyts, E., & Main, K. M. (2001). Testicular dysgenesis syndrome: an increasingly common developmental disorder with environmental aspects. Human Reproduction, 16(5), 972–978.
Skakkebaek, N. E., Jørgensen, N., Andersson, A. M., Juul, A., Main, K. M., Jensen, T. K., & Toppari, J. (2019). Populations, decreasing fertility, and reproductive health. Lancet, 393(10180), 1500–1501.
Skakkebaek, N. E. (2017). Sperm counts, testicular cancers, and the environment. BMJ, 359, j4517. https://doi.org/10.1136/bmj.j4517.
Johnson, M. D. (1998). Genetic risks of intracytoplasmic sperm injection in the treatment of male infertility: Recommendations for genetic counseling and screening. Fertility and Sterility, 70(3), 397–411.
Tüttelmann, F., Ruckert, C., & Röpke, A. (2018). Disorders of spermatogenesis: Perspectives for novel genetic diagnostics after 20 years of unchanged routine. Medizinische Genetik, 30(1), 12–20.
Thirumavalavan, N., Gabrielsen, J. S., & Lamb, D. J. (2019). Where are we going with gene screening for male infertility? Fertility and Sterility, 111(5), 842–850.
Krausz, C., Cioppi, F., & Riera-Escamilla, A. (2018). Testing for genetic contributions to infertility: Potential clinical impact. Expert Review of Molecular Diagnostics, 18(4), 331–346.
Yang, X., Zhang, H., Jiang, Y., Zhang, H., Hu, X., Zhu, D., et al. (2018). Association study between MTRR, TAF4B, PIWIL1 variants and non-obstructive azoospermia in northeast Chinese Han population. Clinical Laboratory, 64(10), 1731–1738.
Salian, S., Doshi, T., & Vanage, G. (2011). Perinatal exposure of rats to Bisphenol a affects fertility of male offspring--an overview. Reproductive Toxicology, 31(3), 359–362.
Doshi, T., D'souza, C., & Vanage, G. (2013). Aberrant DNA methylation at Igf2-H19 imprinting control region in spermatozoa upon neonatal exposure to bisphenol a and its association with post implantation loss. Molecular Biology Reports, 40(8), 4747–4757.
Dumasia, K., Kumar, A., Deshpande, S., & Balasinor, N. H. (2017). Estrogen signaling, through estrogen receptor β, regulates DNA methylation and its machinery in male germ line in adult rats. Epigenetics, 12(6), 476–483.
Pathak, S., Kedia-Mokashi, N., Saxena, M., D'Souza, R., Maitra, A., Parte, P., Gill-Sharma, M., & Balasinor, N. (2009). Effect of tamoxifen treatment on global and insulin-like growth factor 2-H19 locus-specific DNA methylation in rat spermatozoa and its association with embryo loss. Fertility and Sterility, 91(5 Suppl), 2253–2263.
Ankolkar, M., Salvi, V., Warke, H., Vundinti, B. R., & Balasinor, N. H. (2013). Methylation status of imprinted genes DLK1-GTL2, MEST (PEG1), ZAC (PLAGL1), and LINE-1 elements in spermatozoa of normozoospermic men, unlike H19 imprinting control regions, is not associated with idiopathic recurrent spontaneous miscarriages. Fertility and Sterility, 99(6), 1668–1673.
Ankolkar, M., Patil, A., Warke, H., Salvi, V., Kedia Mokashi, N., Pathak, S., & Balasinor, N. H. (2012). Methylation analysis of idiopathic recurrent spontaneous miscarriage cases reveals aberrant imprinting at H19 ICR in normozoospermic individuals. Fertility and Sterility, 98(5), 1186–1192.
Buñay, J., Larriba, E., Patiño-Garcia, D., Urriola-Muñoz, P., Moreno, R. D., & Del Mazo, J. (2019). Combined proteomic and miRNome analyses of mouse testis exposed to an endocrine disruptors chemicals mixture reveals altered toxicological pathways involved in male infertility. Molecular Human Reproduction, 25(3), 156–169.
Shaikh, A., Anand, S., Kapoor, S., Ganguly, R., & Bhartiya, D. (2017). Mouse bone marrow VSELs exhibit differentiation into three embryonic germ lineages and germ & hematopoietic cells in culture. Stem Cell Reviews and Reports, 13, 202–216.
Kucia, M., Reca, R., Campbell, F. R., et al. (2006). A population of very small embryonic-like (VSEL) CXCR4(+) SSEA-1(+)Oct-4+ stem cells identified in adult bone marrow. Leukemia, 20(5), 857–869.
Ratajczak, M. Z., Ratajczak, J., & Kucia, M. (2019). Very small embryonic-like stem cells (VSELs). Circulation Research, 124, 208–210.
Anand, S., Bhartiya, D., Sriraman, K., & Mallick, A. (2016). Underlying mechanisms that restore spermatogenesis on transplanting healthy niche cells in busulphan treated mouse testis. Stem Cell Reviews, 12, 682–697.
Patel, H., & Bhartiya, D. (2016). Testicular stem cells express follicle-stimulating hormone receptors and are directly modulated by FSH. Reproductive Sciences, 11, 1493–1508.
Anand, S., Patel, H., & Bhartiya, D. (2015). Chemoablated mouse seminiferous tubular cells enriched for very small embryonic-like stem cells undergo spontaneous spermatogenesis in vitro. Reproductive Biology and Endocrinology, 13, 33.
Kaushik, A., & Bhartiya, D. (2020). Additional evidence to establish existence of two stem cell populations including VSELs and SSCs in adult mouse testes. Stem Cells Reviews and Reports, https://doi.org/10.1007/s12015-020-09993-6.
Bhartiya, D., Patel, H., Ganguly, R., Shaikh, A., Shukla, Y., Sharma, D., & Singh, P. (2018). Novel insights into adult and cancer stem cell biology. Stem Cells and Development, 22, 1527–1539.
Bhartiya, D. (2018). Stem cells survive oncotherapy & can regenerate non-functional gonads: A paradigm shift for oncofertility. The Indian Journal of Medical Research, 148, 38–49.
Couse, J. F., Dixon, D., Yates, M., Moore, A. B., Ma, L., Maas, R., & Korach, K. S. (2001). Estrogen receptor-alpha knockout mice exhibit resistance to the developmental effects of neonatal diethylstilbestrol exposure on the female reproductive tract. Developmental Biology, 238(2), 224–238.
Nanjappa, M. K., Medrano, T. I., Mesa, A. M., Ortega, M. T., Caldo, P. D., Mao, J., Kinkade, J. A., Levin, E. R., Rosenfeld, C. S., & Cooke, P. S. (2019). Mice lacking membrane estrogen receptor 1 are protected from reproductive pathologies resulting from developmental estrogen exposure. Biology of Reproduction, 101(2), 392–404.
Kaushik, A., & Bhartiya, D. (2018). Pluripotent very small embryonic-like stem cells in adult testes - an alternate premise to explain testicular germ cell tumors. Stem Cell Reviews and Reports, 14(6), 793–800.
Chapman, J. C., Min, S. H., Freeh, S. M., & Michael, S. D. (2009). The estrogen-injected female mouse: New insight into the etiology of PCOS. Reproductive Biology and Endocrinology, 7, 47.
Newbold, R. R., Bullock, B. C., & McLachlan, J. A. (1990). Uterine adenocarcinoma in mice following developmental treatment with estrogens: A model for hormonal carcinogenesis. Cancer Research, 50(23), 7677–7681.
Shirakawa, T., Yaman-Deveci, R., Tomizawa, S., Kamizato, Y., Nakajima, K., Sone, H., Sato, Y., Sharif, J., Yamashita, A., Takada-Horisawa, Y., Yoshida, S., Ura, K., Muto, M., Koseki, H., Suda, T., & Ohbo, K. (2013). An epigenetic switch is crucial for spermatogonia to exit the undifferentiated state toward a kit-positive identity. Development, 140(17), 3565–3576.
Zuba-Surma, E. K., Kucia, M., Abdel-Latif, A., Dawn, B., Hall, B., Singh, R., Lillard JW Jr, & Ratajczak, M. Z. (2008). Morphological characterization of very small embryonic-like stem cells (VSELs) by ImageStream system analysis. Journal of Cellular and Molecular Medicine, 12(1), 292–303.
Atanassova, N., McKinnell, C., Turner, K. J., Walker, M., Fisher, J. S., Morley, M., Millar, M. R., Groome, N. P., & Sharpe, R. M. (2000). Comparative effects of neonatal exposure of male rats to potent and weak (environmental) estrogens on spermatogenesis at puberty and the relationship to adult testis size and fertility: Evidence for stimulatory effects of low estrogen levels. Endocrinology, 141, 3898–3907.
Xing, J. S., & Bai, Z. M. (2018). Is testicular dysgenesis syndrome a genetic, endocrine, or environmental disease, or an unexplained reproductive disorder? Life Sciences, 194, 120–129.
Cheng, L., Albers, P., Berney, D. M., Feldman, D. R., Daugaard, G., Gilligan, T., & Looijenga, L. H. J. (2018). Testicular cancer. Nature Reviews. Disease Primers, 4(1), 29.
Berney, D. M., Looijenga, L. H., Idrees, M., Oosterhuis, J. W., Rajpert-De Meyts, E., Ulbright, T. M., & Skakkebaek, N. E. (2016). Germ cell neoplasia in situ (GCNIS): Evolution of the current nomenclature for testicular pre-invasive germ cell malignancy. Histopathology, 69(1), 7–10.
Zhang, M., Zhou, H., Zheng, C., Xiao, J., Zuo, E., Liu, W., Xie, D., Shi, Y., Wu, C., Wang, H., Li, D., & Li, J. (2014). The roles of testicular c-kit positive cells in de novo morphogenesis of testis. Scientific Reports, 4, 5936.
Rossi, P. (2013). Transcriptional control of KIT gene expression during germ cell development. The International Journal of Developmental Biology, 57(2–4), 179–184.
de Rooij, D. G., & Russell, L. D. (2000). All you wanted to know about spermatogonia but were afraid to ask. Journal of Andrology, 21(6), 776–798.
Schrans-Stassen, B. H., van de Kant, H. J., de Rooij, D. G., & van Pelt, A. M. (1999). Differential expression of c-kit in mouse undifferentiated and differentiating type a spermatogonia. Endocrinology, 140(12), 5894–5900.
Yoshinaga, K., Nishikawa, S., Ogawa, M., Hayashi, S., Kunisada, T., Fujimoto, T., & Nishikawa, S. (1991). Role of c-kit in mouse spermatogenesis: Identification of spermatogonia as a specific site of c-kit expression and function. Development, 113(2), 689–699.
Blume-Jensen, P., Jiang, G., Hyman, R., Lee, K. F., O'Gorman, S., & Hunter, T. (2004). Kit/stem cell factor receptor-induced activation of phosphatidylinositol 3′-kinase is essential for male fertility. Nature Genetics, 24(2), 157–162.
Kissel, H., Timokhina, I., Hardy, M. P., Rothschild, G., Tajima, Y., Soares, V., Angeles, M., Whitlow, S. R., Manova, K., & Besmer, P. (2000). Point mutation in kit receptor tyrosine kinase reveals essential roles for kit signaling in spermatogenesis and oogenesis without affecting other kit responses. The EMBO Journal, 19(6), 1312–1326.
Jackson, M., Krassowska, A., Gilbert, N., Chevassut, T., Forrester, L., Ansell, J., & Ramsahoye, B. (2004). Severe global DNA hypomethylation blocks differentiation and induces histone hyperacetylation in embryonic stem cells. Molecular and Cellular Biology, 24, 8862–8871.
Shin, D. M., Liu, R., Klich, I., Ratajczak, J., Kucia, M., & Ratajczak, M. Z. (2010). Molecular characterization of isolated from murine adult tissues very small embryonic/epiblast like stem cells (VSELs). Molecules and Cells, 29(6), 533–538.
Ratajczak, M. Z. (2012). Igf2-H19, an imprinted tandem gene, is an important regulator of embryonic development, a guardian of proliferation of adult pluripotent stem cells, a regulator of longevity, and a 'passkey' to cancerogenesis. Folia Histochemica et Cytobiologica, 50(2), 171–179.
Shin, D. M., Zuba-Surma, E. K., Wu, W., Ratajczak, J., Wysoczynski, M., Ratajczak, M. Z., & Kucia, M. (2009). Novel epigenetic mechanisms that control pluripotency and quiescence of adult bone marrow-derived Oct4(+) very small embryonic-like stem cells. Leukemia, 23(11), 2042–2051.
Duca, Y., Calogero, A. E., Cannarella, R., Condorelli, R. A., & La Vignera, S. (2019). Current and emerging medical therapeutic agents for idiopathic male infertility. Expert Opinion on Pharmacotherapy, 20(1), 55–67.
Borght, V. M., & Wyns, C. (2018). Fertility and infertility: Definition and epidemiology. Clinical Biochemistry, 62, 2–10.
Casarini, L., Crépieux, P., Reiter, E., Lazzaretti, C., Paradiso, E., Rochira, V., Brigante, G., Santi, D., & Simoni, M. (2020). FSH for the treatment of male infertility. International Journal of Molecular Sciences, 21(7), 2270.
Strohsnitter, W.C. (2019). Prenatal diethylstilbestrol exposure: A harbinger for future testicular cancer incidence? JNCI Cancer Spectrum. https://doi.org/10.1093/jncics/pkz046, 3.
Stang, A., Rusner, C., Trabert, B., Oosterhuis, J. W., McGlynn, K. A., & Heidinger, O. (2019). Incidence of testicular tumor subtypes according to the updated WHO classification, North Rhine-Westphalia, Germany, 2008-2013. Andrology, 7(4), 402–407.
Hom, M., Sriprasert, I., Ihenacho, U., Castelao, J.E., Siegmund, K., Bernstein, L., Cortessis, V.K.(2019).Systematic review and metaanalysis of testicular germ cell tumors following in utero exposure to diethylstilbestrol. JNCI Cancer Spectr, 3(3).
Newbold, R. R., Hanson, R. B., Jefferson, W. N., Bullock, B. C., Haseman, J., & McLachlan, J. A. (2000). Proliferative lesions and reproductive tract tumors in male descendants of mice exposed developmentally to diethylstilbestrol. Carcinogenesis, 21(7), 1355–1363.
Rahman, M. M., Wie, J., Cho, J. H., Tae, H. J., Ahn, D., Lee, S. W., Kim, I. S., & Park, B. Y. (2019). Diethylstilbestrol induces morphological changes in the spermatogonia, Sertoli cells and Leydig cells of adult rat. Research in Veterinary Science, 124, 433–438.
Miyaso, H., Naito, M., Hirai, S., Matsuno, Y., Komiyama, M., Itoh, M., & Mori, C. (2014). Neonatal exposure to diethylstilbestrol causes granulomatous orchitis via epididymal inflammation. Anatomical Science International, 89(4), 215–223.
Hotaling, J. M., & Walsh, T. J. (2009). Male infertility: A risk factor for testicular cancer. Nature Reviews. Urology, 6(10), 550–556.
Ratajczak, M. Z., Shin, D. M., & Kucia, M. (2009). Very small embryonic/epiblast-like stem cells: a missing link to support the germ line hypothesis of cancer development? The American Journal of Pathology, 174(6), 1985–1992.
Ratajczak, M. Z., Bujko, K., Mack, A., Kucia, M., & Ratajczak, J. (2018). Cancer from the perspective of stem cells and misappropriated tissue regeneration mechanisms. Leukemia, 32(12), 2519–2526.
Mitchell, R. T., Camacho-Moll, M. E., Macdonald, J., Anderson, R. A., Kelnar, C. J. H., O'Donnell, M., et al. (2014). Intratubular germ cell neoplasia of the human testis: Heterogeneous protein expression and relation to invasive potential. Modern Pathology, 27, 1255–1266.
Acknowledgements
Authors are thankful to the Central Facilities at the Institute for their help. DB is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
NIRRH Accession Number
NIRRH/MS/RA/850/12–2019.
Funding
We are thankful to Indian Council of Medical Research for providing financial support and to UGC for fellowship (11-04-2016-329,600) to AK.
Author information
Authors and Affiliations
Contributions
DB planned and designed the study and arranged financial support. AK performed all the experiments. Data analysis, interpretation and manuscript preparation was done by DB, AK and SA. All authors have read and agreed to final version of the manuscript.
Corresponding author
Ethics declarations
Yes
Conflict of Interest
No potential conflicts of interest relevant to this article were reported.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 1767 kb)
Rights and permissions
About this article
Cite this article
Kaushik, A., Anand, S. & Bhartiya, D. Altered Biology of Testicular VSELs and SSCs by Neonatal Endocrine Disruption Results in Defective Spermatogenesis, Reduced Fertility and Tumor Initiation in Adult Mice. Stem Cell Rev and Rep 16, 893–908 (2020). https://doi.org/10.1007/s12015-020-09996-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-020-09996-3