Abstract
Developmental exposure to endocrine disruptors has resulted in the increased incidence of infertility and testicular germ cell tumors (T2GCT) in young men residing in developed countries. Unlike T1GCT (infants and young children) and T3GCT (aged men), T2GCT arise from CIS/GCNIS that develops from pre-CIS. Pre-CIS represents undifferentiated, growth-arrested gonocytes that persist in fetal testes due to endocrine disruption. However, whether pre-CIS truly exist, do CIS develop into T2GCT, why no CIS in T1GCT/T3GCT, why germ cell tumors (GCT) also occur along midline at extra-gonadal sites, why T1GCT show partial erasure and T2GCT show complete erasure of genomic imprints are open questions that are awaiting answers. We propose that rather than pre-CIS, pluripotent, very small embryonic-like stem cells (VSELs) get affected by exposure to endocrine disruption. Since VSELs are developmentally equivalent to primordial germ cells (PGCs), T2GCT cells show complete erasure of genomic imprints and CIS represents growth-arrested clonally expanding stem/progenitor cells. PGCs/VSELs migrate along the midline to various organs and this explains why GCT occur along the midline, T1GCT show partial erasure of imprints as they develop from migrating PGCs. T3GCT possibly reflects effects of aging due to compromised differentiation and expansion of pre-meiotic spermatocytes. Absent spermatogenesis in pre-pubertal and aged testes explains absence of CIS in T1GCT and T3GCT. Endocrine disruptors possibly alter epigenetic state of VSELs and thus rather than maintaining normal tissue homeostasis, VSELs undergo increased proliferation and compromised differentiation resulting in reduced sperm count, infertility and TGCT. This newly emerging understanding offers alternate premise to explain TGCT and warrants further exploration.


Similar content being viewed by others
Abbreviations
- VSELs:
-
Very small embryonic-like stem cells
- SSCs:
-
Spermatogonial stem cells
- PGCs:
-
Primordial germ cells
- TGCT:
-
Testicular germ cell tumors
- CIS:
-
Carcinoma in situ
- GCNIS:
-
Germ cell neoplasia in situ
- OCT-4A:
-
Transcription factor reflecting pluripotent state
- FSH:
-
Follicle stimulating hormone
References
Skakkebaek, N. E., Rajpert-De Meyts, E., & Main, K. M. (2001). Testicular dysgenesis syndrome: An increasingly common developmental disorder with environmental aspects. Human Reproduction, 16(5), 972–978.
Xing, J. S., & Bai, Z. M. (2018). Is testicular dysgenesis syndrome a genetic, endocrine, or environmental disease, or an unexplained reproductive disorder? Life Sciences, 194, 120–129.
Ostrowski, K. A., & Walsh, T. J. (2015). Infertility with testicular Cancer. The Urologic Clinics of North America, 42(3), 409–420.
Jacobsen, R., Bostofte, E., Engholm, G., Hansen, J., Olsen, J. H., Skakkebaek, N. E., & Moller, H. (2000). Risk of testicular cancer in men with abnormal semen characteristics: cohort study. BMJ, 321(7264), 789–792.
Walsh, T. J., Croughan, M. S., Schembri, M., Chan, J. M., & Turek, P. J. (2009). Increased risk of testicular germ cell cancer among infertile men. Archives of Internal Medicine, 169(4), 351–356.
Rajpert-De Meyts E, Skakkebaek NE, Toppari J. (2018) Testicular cancer pathogenesis, diagnosis and endocrine aspects. In: Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; Editors. De Groot LJ, et al. https://www.ncbi.nlm.nih.gov/pubmed/25905224.
Spiller, C. M., & Bowles, J. (2017). Germ cell neoplasia in situ: The precursor cell for invasive germ cell tumors of the testis. The International Journal of Biochemistry & Cell Biology, 86, 22–25.
Elzinga-Tinke, J. E., Dohle, G. R., & Looijenga, L. H. (2015). Etiology and early pathogenesis of malignant testicular germ cell tumors: Towards possibilities for preinvasive diagnosis. Asian Journal of Andrology, 17(3), 381–393.
Hanna, N. H., & Einhorn, L. H. (2014). Testicular cancer--discoveries and updates. The New England Journal of Medicine, 371(21), 2005–2016.
Ghazarian, A. A., Kelly, S. P., Altekruse, S. F., Rosenberg, P. S., & McGlynn, K. A. (2017). Future of testicular germ cell tumor incidence in the United States: Forecast through 2026. Cancer, 123(12), 2320–2328.
Le Cornet, C., Lortet-Tieulent, J., Forman, D., Béranger, R., Flechon, A., Fervers, B., et al. (2014). Testicularcancer incidence to rise by 25%by 2025 in Europe? Model based predictions in 40 countries using population-based registry data. European Journal of Cancer, 50(4), 831–839.
Shanmugalingam, T., Soultati, A., Chowdhury, S., Rudman, S., & Van Hemelrijck, M. (2013). Global incidence and outcome of testicular cancer. Clin Epidemiol., 5, 417–427.
Kristensen, D. G., Skakkebæk, N. E., Rajpert-De Meyts, E., & Almstrup, K. (2013). Epigenetic features of testicular germ cell tumors in relation to epigenetic characteristics of foetal germ cells. The International Journal of Developmental Biology, 57(2–4), 309–317.
Looijenga, L. H., Verkerk, A. J., Dekker, M. C., van Gurp, R. J., Gillis, A. J., & Oosterhuis, J. W. (1998). Genomic imprinting in testicular germ cell tumours. APMIS, 106(1), 187–195.
Lim, J., Goriely, A., Turner, G. D., Ewen, K. A., Jacobsen, G. K., Graem, N., Wilkie, A. O., & Rajpert-De Meyts, E. (2011). OCT2, SSX and SAGE1 reveal the phenotypic heterogeneity of spermatocytic seminoma reflecting distinct subpopulations of spermatogonia. The Journal of Pathology, 224(4), 473–483.
Yang, Q. E., & Oatley, J. M. (2014). Spermatogonial stem cell functions in physiological and pathological conditions. Current Topics in Developmental Biology, 107, 235–267.
Rajpert-De Meyts, E. (2006). Developmental model for the pathogenesis of testicular carcinoma in situ: Genetic and environmental aspects. Human Reproduction Update, 12(3), 303–323.
Oosterhuis, J. W., Stoop, H., Dohle, G., Boellaard, W., van Casteren, N., Wolffenbuttel, K., & Looijenga, L. H. (2011). A pathologist's view on the testis biopsy. International Journal of Andrology, 34, e14–e20. https://doi.org/10.1111/j.1365-2605.2011.01204.x.
Jorgensen, A., Johansen, M. L., Juul, A., Skakkebaek, N. E., Main, K. M., & Rajpert-De Meyts, E. (2015). Pathogenesis of germ cell neoplasia in testicular dysgenesis and disorders of sex development. Seminars in Cell & Developmental Biology, 45, 124–137.
de Jong, B., Oosterhuis, J. W., Castedo, S. M., Vos, A., & te Meerman, G. J. (1990). Pathogenesis of adult testicular germ cell tumors. A cytogenetic model. Cancer Genetics and Cytogenetics, 48(2), 143–167.
Rajpert-De Meyts, E., & Skakkebaek, N. E. (2011). Pathogenesis of testicular carcinoma in situ and germ cell cancer: Still more questions than answers. International Journal of Andrology, 34(4), e2–e6.
Skakkebaek, N. E. (1972). Possible carcinoma-in-situ of the testis. Lancet, 2(7776), 516–517.
Berney, D. M., Looijenga, L. H., Idrees, M., Oosterhuis, J. W., Rajpert-De Meyts, E., Ulbright, T. M., & Skakkebaek, N. E. (2016). Germ cell neoplasia in situ (GCNIS): evolution of the current nomenclature for testicular pre-invasive germ cell malignancy. Histopathology, 69(1), 7–10.
Burns, W. R., Sabanegh, E., Dada, R., Rein, B., & Agarwal, A. (2010). Is male infertility a forerunner to cancer? Intl Braz J Urol, 36, 527–536.
Litchfield, K., Loveday, C., Levy, M., Dudakia, D., Rapley, E., Nsengimana, J., Bishop, D. T., Reid, A., Huddart, R., Broderick, P., Houlston, R. S., & Turnbull, C. (2018). Large-scale sequencing of testicular germ cell tumour (TGCT) cases excludes major TGCT predisposition gene. European Urology, 73(6), 828–831.
Rajpert-De Meyts, E., & Skotheim, R. I. (2018). Complex polygenic nature of testicular germ cell cancer suggests multifactorial aetiology. European Urology, 73(6), 832–833.
Nielsen, J. E., Kristensen, D. M., Almstrup, K., Jørgensen, A., Olesen, I. A., Jacobsen, G. K., Horn, T., Skakkebaek, N. E., Leffers, H., & Rajpert-de Meyts, E. (2012). A novel double staining strategy for improved detection of testicular carcinoma in situ cells in human semen samples. Andrologia, 44(2), 78–85.
Akyüz, M., Topaktaş, R., Ürkmez, A., Koca, O., & Öztürk, M. İ. (2018). Evaluation of germ-cell neoplasia in situ entity in testicular tumors. Turk J Urol., 16, 1–5.
Basiri, A., Movahhed, S., Parvin, M., Salimi, M., & Rezaeetalab, G. H. (2016). The histologic features of intratubular germ cell neoplasia and its correlation with tumor behavior. Investig Clin Urol, 53(3), 195–205.
Kucia, M., Reca, R., Campbell, F. R., Zuba-SurmaE, M. M., Ratajczak, J., & Ratajczak, M. Z. (2006). A population of very small embryonic-like (VSEL) CXCR4(+) SSEA-1(+)Oct-4+ stem cells identified in adult bone marrow. Leukemia, 20, 857–869.
Zuba-Surma, E. K., Kucia, M., Wu, W., Klich, I., Lillard Jr., J. W., Ratajczak, J., & Ratajczak, M. Z. (2008). Very small embryonic-like stem cells are present in adult murine organs: ImageStream-based morphological analysis and distribution studies. Cytometry. Part A, 73A, 1116–1127.
Kucia, M., Halasa, M., Wysoczynski, M., Baskiewicz-Masiuk, M., Moldenhawer, S., Zuba-Surma, E., Czajka, R., Wojakowski, W., Machalinski, B., & Ratajczak, M. Z. (2007). Morphological and molecular characterization of novel population of CXCR4+ SSEA-4+ Oct-4+ very small embryonic-like cells purified from human cord blood: Preliminary report. Leukemia, 21(2), 297–303.
Bhartiya, D., Shaikh, A., Nagvenkar, P., Kasiviswanathan, S., Pethe, P., Pawani, H., Mohanty, S., Rao, S. G., Zaveri, K., & Hinduja, I. (2012). Very small embryonic-like stem cells with maximum regenerative potential get discarded during cord blood banking and bone marrow processing for autologous stem cell therapy. Stem Cells and Development, 21(1), 1–6.
Abbott, A. (2013). Doubt cast over tiny stem cells. Nature, 499, 390.
Bhartiya, D. (2017). Pluripotent stem cells in adult tissues: Struggling to be acknowledged over two decades. Stem Cell Reviews, 13(6), 713–724.
Ratajczak, M. Z., Zuba-Surma, E. K., Machalinski, B., Ratajczak, J., & Kucia, M. (2008). Very small embryonic-like (VSEL) stem cells: Purification from adult organs, characterization, and biological significance. Stem Cell Reviews, 4(2), 89–99.
Ratajczak, M. Z., Zuba-Surma, E. K., Wysoczynski, M., Wan, W., Ratajczak, J., Wojakowski, W., & Kucia, M. (2008). Hunt for pluripotent stem cell -- regenerative medicine search for almighty cell. Journal of Autoimmunity, 30(3), 151–162.
Virant-Klun, I. (2016). Very small embryonic-like stem cells: A potential developmental link between germinal lineage and hematopoiesis in humans. Stem Cells and Development, 25(2), 101–113.
Scaldaferri, M. L., Klinger, F. G., Farini, D., Di Carlo, A., Carsetti, R., Giorda, E., & De Felici, M. (2015). Hematopoietic activity in putative mouse primordial germ cell population. Mechanisms of Development, 136, 53–63.
Lahlil, R., Scrofani, M., Barbet, R., Tancredi, C., Aries, A., & Hénon, P. (2018). VSELs maintain their pluripotency and competence to differentiate after enhanced ex vivo expansion. Stem Cell Reviews, 14, 510–524. https://doi.org/10.1007/s12015-018-9821-1.
Ratajczak, M. Z. (2017). Why are hematopoietic stem cells so 'sexy'? On a search for developmentalexplanation. Leukemia, 31(8), 1671–1677.
Bhartiya, D., Shaikh, A., Anand, S., Patel, H., Kapoor, S., Sriraman, K., Parte, S., & Unni, S. (2016). Endogenous, very small embryonic-like stem cells: Critical review, therapeutic potential and a look ahead. Human Reproduction Update, 23(1), 41–76.
Ratajczak, M. Z., Marycz, K., Poniewierska-Baran, A., Fiedorowicz, K., Zbucka-Kretowska, M., & Moniuszko, M. (2014). Very small embryonic-like stem cells as a novel developmental concept and the hierarchy of the stem cell compartment. Advances in Medical Sciences, 59(2), 273–280.
Shin, D. M., Liu, R., Klich, I., Ratajczak, J., Kucia, M., & Ratajczak, M. Z. (2010). Molecular characterization of isolated from murine adult tissues very small embryonic/epiblast like stem cells (VSELs). Molecules and Cells, 29(6), 533–538.
Kim, Y., Jeong, J., Kang, H., Lim, J., Heo, J., Ratajczak, J., Ratajczak, M. Z., & Shin, D. M. (2014). The molecular nature of very small embryonic-like stem cells in adult tissues. Int J Stem Cells, 7(2), 55–62.
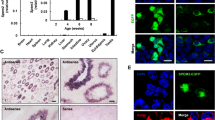
Bhartiya, D., Kasiviswanathan, S., Unni, S. K., Pethe, P., Dhabalia, J. V., Patwardhan, S., & Tongaonkar, H. B. (2010). Newer insights into premeiotic development of germ cells in adult human testis using Oct-4 as a stem cell marker. The Journal of Histochemistry and Cytochemistry, 58(12), 1093–1010.
Kanatsu-Shinohara, M., Inoue, K., Lee, J., Yoshimoto, M., Ogonuki, N., Miki, H., Baba, S., Kato, T., Kazuki, Y., Toyokuni, S., Toyoshima, M., Niwa, O., Oshimura, M., Heike, T., Nakahata, T., Ishino, F., Ogura, A., & Shinohara, T. (2004). Generation of pluripotent stem cells from neonatal mouse testis. Cell, 119(7), 1001–1012.
Guan, K., Nayernia, K., Maier, L. S., Wagner, S., Dressel, R., Lee, J. H., Nolte, J., Wolf, F., Li, M., Engel, W., & Hasenfuss, G. (2006). Pluripotency of spermatogonial stem cells from adult mouse testis. Nature, 440(7088), 1199–1203.
Bhartiya, D., Kasiviswananthan, S., & Shaikh, A. (2012). Cellular origin of testis-derived pluripotent stem cells: A case for very small embryonic-like stem cells. Stem Cells and Development, 21(5), 670–674.
Anand, S., Bhartiya, D., Sriraman, K., Patel, H., & Manjramkar, D. D. (2014). Very small embryonic-like stem cells survive and restore spermatogenesis after busulphan treatment in mouse testis. J Stem Cell Res Ther., 12, 628–697. https://doi.org/10.1007/s12015-016-9685-1.
Anand, S., Bhartiya, D., Sriraman, K., & Mallick, A. (2016). Underlying mechanisms that restore spermatogenesis on transplanting healthy niche cells in busulphan treated mouse testis. Stem Cell Reviews, 12(6), 682–697.
Patel, H., & Bhartiya, D. (2016). Testicular stem cells express follicle-stimulating hormone receptors and are directly modulated by FSH. Reproductive Sciences, 23(11), 1493–1508.
Kurkure, P., Prasad, M., Dhamankar, V., & Bakshi, G. (2015). Very small embryonic-like stem cells (VSELs) detected in azoospermic testicular biopsies of adult survivors of childhood cancer. Reproductive Biology and Endocrinology, 13, 122. https://doi.org/10.1186/s12958-015-0121-1.
Stimpfel, M., Skutella, T., Kubista, M., Malicev, E., Conrad, S., & Virant-Klun, I. (2012). Potential stemness of frozen-thawed testicular biopsies without sperm in infertile men included into the in vitro fertilization programme. Journal of Biomedicine & Biotechnology, 2012, 1–15. https://doi.org/10.1155/2012/291038.
Virant-Klun, I., Zech, N., Rozman, P., Vogler, A., Cvjeticanin, B., Klemenc, P., Malicev, E., & Meden-Vrtovec, H. (2008). Putative stem cells with an embryonic character isolated from the ovarian surface epithelium of women with no naturally present follicles and oocytes. Differentiation, 76, 843–856.
Bruggeman, J. W., Koster, J., Lodder, P., Repping, S., & Hamer, G. (2018). Massive expression of germ cell-specific genes is a hallmark of cancer and a potential target for novel treatment development. Oncogene. https://doi.org/10.1038/s41388-018-0357-2.
Ratajczak, M. Z., Shin, D. M., Liu, R., Marlicz, W., Tarnowski, M., Ratajczak, J., & Kucia, M. (2010). Epiblast/germ line hypothesis of cancer development revisited: lesson from the presence of Oct-4+ cells in adult tissues. Stem Cell Reviews, 6(2), 307–316.
Bhartiya, D., & Ganguly, R. (2016). Do somatic cells de-differentiate/trans-differentiate or vsels initiate cancer and explain plasticity in adult tissues? J Cancer Stem Cell Research, 4, e1006. https://doi.org/10.14343/JCSCR.2016.4e1006.
Bhartiya, D. (2017). Do adult somatic cells undergo reprogramming or endogenous pluripotent stem cells get activated to account for plasticity, regeneration and cancer initiation? Stem Cell Reviews, 13(5), 699–701.
De Felici, M. (2016). The formation and migration of primordial germ cells in mouse and man. Results and Problems in Cell Differentiation, 58, 23–46.
Cantú, A. V., & Laird, D. J. (2017). A pilgrim’s progress: Seeking meaning in primordial germ cell migration. Stem Cell Research, 24, 181–187.
Ferlin, A., Pengo, M., Selice, R., Salmaso, L., Garolla, A., & Foresta, C. (2008). Analysis of single nucleotide polymorphismsof FSH receptor genesuggests association with testicular cancer susceptibility. Endocrine-Related Cancer, 5(2), 429–437.
Bang, A. K., Busch, A. S., Almstrup, K., Gromoll, J., Kliesch, S., Rajpert-De Meyts, E., Skakkebaek, N. E., Juul, A., Tüttelmann, F., & Jørgensen, N. (2018). Is the FSHR 2039A>G variant associated with susceptibility to testicular germ cell cancer? Andrology., 6(1), 176–183.
Tüttelmann, F., Laan, M., Grigorova, M., Punab, M., Sõber, S., & Gromoll, J. (2012). Combined effects of the variants FSHB -211G>T and FSHR 2039A>G on male reproductive parameters. The Journal of Clinical Endocrinology and Metabolism, 97(10), 3639–3647.
Bhartiya, D., Patel, H., Ganguly, R., Shaikh, A., Shukla, Y., Sharma, D., & Singh, P. (2018). Novel insights into adult and cancer stem cell biology. Stem Cells and Development. https://doi.org/10.1089/scd.2018.0118.
Acknowledgements
Authors thank ICMR for providing financial support. AK also thanks CSIR/UGC for her fellowship during her PhD program. NIRRH manuscript number is REV/655/07-2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kaushik, A., Bhartiya, D. Pluripotent Very Small Embryonic-Like Stem Cells in Adult Testes – An Alternate Premise to Explain Testicular Germ Cell Tumors. Stem Cell Rev and Rep 14, 793–800 (2018). https://doi.org/10.1007/s12015-018-9848-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-018-9848-3