Abstract
Background
In this study, we hypothesized that activation of PPAR-γ enhanced MSCs survival and their therapeutic efficacy via upregulating the expression of Cx43.
Methods
MI was induced in 50 male Sprague–Dawley rats. The rats were randomized into five groups: MI group and four intervention groups, including the MSCs group, combined therapy group (MSCs+ pioglitazone), pioglitazone group and PBS group. Two weeks later, 5 × 106 MSCs labeled with PKH26 in PBS were injected into the infarct anterior ventricular free wall in the MSCs and combined therapy groups, and PBS alone was injected into the infarct anterior ventricular free wall in the PBS group. Pioglitazone (3 mg/kg/day) was given to the combined therapy and pioglitazone groups by oral gavage at the same time for another 2 weeks. Myocardial function and relevant signaling molecules involved were all examined thereafter.
Results
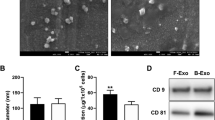
Heart function was enhanced after MSCs treatment for 2 weeks post MI. A significant improvement of heart function was observed in the combined therapy group in contrast to the other three intervention groups. Compared with the MSCs group, there was a higher level of PPAR-γ in the combined therapy group; Cx43 was remarkably increased in different regions of the left ventricle; TGF-β1 was decreased in the infarct zone and border zone. To the downstream signaling molecules, mothers against Smad proteins including Smad2 and Smad3 presented a synchronized alteration with TGF-β1; no differences of the expressions of ERK1/2 and p38 could be discovered in the left ventricular cardiac tissue.
Conclusions
MSCs transplantation combined with pioglitazone administration improved cardiac function more effectively after MI. Activation of PPAR-γ could promote MSCs to express Cx43. Inhibition of TGF-β1/Smads signaling pathway might be involved in the process.







Similar content being viewed by others
Abbreviations
- MSCs:
-
Mesenchymal Stem Cells
- PPAR-γ:
-
Peroxisome Proliferator-activated Receptor Gamma Cx43 Connexin 43
- TGF-β1:
-
Transforming growth factor beta-1
- Smad:
-
Decapentaplegic homolog proteins
- ERK:
-
Extracellular signal-regulated kinase
References
Hou, J., Wang, L., Jiang, J., et al. (2013). Cardiac stem cells and their roles in myocardial infarction. Stem Cell Reviews, 9, 326–338.
Pavo, N., Charwat, S., Nyolczas, N., et al. (2014). Cell therapy for human ischemic heart diseases: critical review and summary of the clinical experiences. Journal of Molecular and Cellular Cardiology, 75, 12–24.
Wen, Z., Zheng, S., Zhou, C., et al. (2011). Repair mechanisms of bone marrow mesenchymal stem cells in myocardial infarction. Journal of Cellular and Molecular Medicine, 15, 1032–1043.
Wang, T., Sun, S., Wan, Z., et al. (2012). Effects of bone marrow mesenchymal stem cells in a rat model of myocardial infarction. Resuscitation, 83, 1391–1396.
Santos, Nascimento, D., Mosqueira, D., Sousa, L. M., et al. (2014). Human umbilical cord tissue-derived mesenchymal stromal cells attenuate remodeling after myocardial infarction by proangiogenic, antiapoptotic, and endogenous cell-activation mechanisms. Stem Cell Research & Therapy, 5, 5.
Hare, J. M., Fishman, J. E., Gerstenblith, G., et al. (2012). Comparison of allogeneic vs autologous bone marrow–derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy The POSEIDON randomized trial mesenchymal stem cells and ischemic cardiomyopathy. JAMA, 308, 2369–2379.
Mathiasen, A. B., Jørgensen, E., Qayyum, A. A., et al. (2012). Rationale and design of the first randomized, double-blind, placebo-controlled trial of intramyocardial injection of autologous bone-marrow derived Mesenchymal Stromal Cells in chronic ischemic Heart Failure (MSC-HF Trial). American Heart Journal, 164, 285–291.
Buravkova, L.B., Andreeva, E.R., Gogvadze, V., et al. (2014). Mesenchymal stem cells and hypoxia: Where are we? Mitochondrion, 19 Pt A, 105–112.
Chacko, S. M., Ahmed, S., Selvendiran, K., et al. (2010). Hypoxic preconditioning induces the expression of prosurvival and proangiogenic markers in mesenchymal stem cells. American Journal of Physiology. Cell Physiology, 299(6), C1562–C1570.
McGinley, L. M., McMahon, J., Stocca, A., et al. (2013). Mesenchymal stem cell survival in the infarcted heart is enhanced by lentivirus vector-mediated heat shock protein 27 expression. Human Gene Therapy, 24(10), 840–851.
Xing, Y., Hou, J., Guo, T., et al. (2014). MicroRNA-378 promotes mesenchymal stem cells survival and vascularization under hypoxic-ischemic condition in vitro. Stem Cell Research & Therapy, 5, 130.
Kim, E., & Fishman, G. I. (2013). Designer gap junctions that prevent cardiac arrhythmias. Trends in Cardiovascular Medicine, 23(2), 33–38.
Li, X., Heinzel, F. R., Boengler, K., et al. (2004). Role of connexin-43 in ischemic preconditioning does not involve intercellular communication through gap junctions. Journal of Molecular and Cellular Cardiology, 36, 161–163.
Taniguchi Ishikawa, E., Gonzalez-Nieto, D., Ghiaur, G., et al. (2012). Connexin-43 prevents hematopoietic stem cell senescence through transfer of reactive oxygen species to bone marrow stromal cells. Proceedings of the National Academy of Sciences of the United States of America, 109(23), 9071–9076.
Lu, G., Haider, H. K., Porollo, A., et al. (2010). Mitochondria-specific transgenic overexpression of connexin-43 simulates preconditioning-induced cytoprotection of stem cells. Cardiovascular Research, 88(2), 277–286.
Wang, D., Shen, W., Zhang, F., et al. (2010). Connexin43 promotes survival of mesenchymal stem cells in ischaemic heart. Cell Biology International, 34(4), 415–423.
Rosen, E. D., & Spiegelman, B. M. (2001). PPARγ: a nuclear regulator of metabolism, differentiation, and cell growth. The Journal of Biological Chemistry, 276(41), 37731–37734.
Ahmadian, M., Suh, J. M., Hah, N., et al. (2013). PPARγ signaling and metabolism: the good, the bad and the future. Nature Medicine, 19(5), 557–566.
Srivastava, R. A. (2011). Evaluation of anti-atherosclerotic activities of PPAR-α, PPAR-γ, and LXR agonists in hyperlipidemic atherosclerosis-susceptible F(1)B hamsters. Atherosclerosis, 4(1), 86–93.
Nagashima, A., Watanabe, R., Ogawa, M., et al. (2012). Different roles of PPAR-γ activity on physiological and pathological alteration after myocardial ischemia. Journal of Cardiovascular Pharmacology, 60(2), 158–164.
Kanakasabai, S., Pestereva, E., Chearwae, W., et al. (2012). PPARγ agonists promote oligodendrocyte differentiation of neural stem cells by modulating stemness and differentiation genes. PLoS One, 7(11), e50500.
Liang, C., Ren, Y., Tan, H., et al. (2009). Rosiglitazone via upregulation of Akt/eNOS pathways attenuates dysfunction of endothelial progenitor cells, induced by advanced glycation end products. British Journal of Pharmacology, 158(8), 1865–1873.
Shinmura, D., Togashi, I., Miyoshi, S., et al. (2011). Pretreatment of human mesenchymal stem cells with pioglitazone improved efficiency of cardiomyogenic transdifferentiation and cardiac function. Stem Cells, 29(2), 357–366.
Segond, N., Degrelle, S. A., Berndt, S., et al. (2013). Transcriptome analysis of PPARγ target genes reveals the involvement of lysyl oxidase in human placental cytotrophoblast invasion. PLoS One, 8(11), e79413.
Kawai, T., Masaki, T., Doi, S., et al. (2009). PPAR-gamma agonist attenuates renal interstitial fibrosis and inflammation through reduction of TGF-beta. Laboratory Investigation, 89(1), 47–58.
Hou, J., Wang, L., Yan, P., et al. (2014). Angiotensin II downregulates connexin 43 via TGF-β1 mediated signaling pathways in a rat model of myocardial infarction. Experimental and Clinical Cardiology, 20(8), 2905–2940.
de Oliveira, F. L., Araújo-Jorge, T. C., de Souza, E. M., et al. (2012). Oral administration of GW788388, an inhibitor of transforming growth factor beta signaling, prevents heart fibrosis in Chagas disease. PLoS Neglected Tropical Diseases, 6(6), e1696.
Williams, A. R., & Hare, J. M. (2011). Mesenchymal stem cells biology, pathophysiology, translational findings, and therapeutic implications for cardiac disease. Circulation Research, 109, 923–940.
Wang, S., Qu, X., & Zhao, R. C. (2012). Clinical applications of mesenchymal stem cells. Journal of Hematology & Oncology, 5, 19.
Zimmet, H., Porapakkham, P., Porapakkham, P., et al. (2012). Short- and long-term outcomes of intracoronary and endogenously mobilized bone marrow stem cells in the treatment of ST-segment elevation myocardial infarction: a meta-analysis of randomized control trials. European Journal of Heart Failure, 14(1), 91–105.
Kandala, J., Upadhyay, G. A., Pokushalov, E., et al. (2013). Meta-analysis of stem cell therapy in chronic ischemic cardiomyopathy. The American Journal of Cardiology, 112(2), 217–225.
Numasawa, Y., Kimura, T., Miyoshi, S., et al. (2011). Treatment of human mesenchymal stem cells with angiotensin receptor blocker improved efficiency of cardiomyogenic transdifferentiation and improved cardiac function via angiogenesis. Stem Cells, 29(9), 1405–1414.
Wang, L., Waltenberger, B., Pferschy-Wenzig, E. M., et al. (2014). Natural product agonists of peroxisome proliferator-activated receptor gamma (PPARγ): a review. Biochemical Pharmacology, 92(1), 73–89.
Morales-Garcia, J. A., Luna-Medina, R., Alfaro-Cervello, C., et al. (2011). Peroxisome proliferator-activated receptor γ ligands regulate neural stem cell proliferation and differentiation in vitro and in vivo. Glia, 59(2), 293–307.
Chiang, M. C., Cheng, Y. C., Lin, K. H., et al. (2013). PPARγ regulates the mitochondrial dysfunction in human neural stem cells with tumor necrosis factor alpha. Neuroscience, 229, 118–129.
Xu, D. Y., Davis, B. B., Wang, Z. H., et al. (2013). A potent soluble epoxide hydrolase inhibitor, t-AUCB, acts through PPARγ to modulate the function of endothelial progenitor cells from patients with acute myocardial infarction. International Journal of Cardiology, 167(4), 1298–1304.
Bruedigam, C., Eijken, M., Koedam, M., et al. (2010). A new concept underlying stem cell lineage skewing that explains the detrimental effects of thiazolidinediones on bone. Stem Cells, 28(5), 916–927.
Scott, M. A., Nguyen, V. T., Levi, B., et al. (2011). Current methods of adipogenic differentiation of mesenchymal stem cells. Stem Cells and Development, 20(10), 1793–1804.
Fontes, M. S., van Veen, T. A., de Bakker, J. M., et al. (2012). Functional consequences of abnormal Cx43 expression in the heart. Biochimica et Biophysica Acta, 181(8), 2020–2029.
Greener, I. D., Sasano, T., Wan, X., et al. (2012). Connexin43 gene transfer reduces ventricular tachycardia susceptibility after myocardial infarction. Journal of the American College of Cardiology, 60(12), 1103–1110.
Lu, G., Jiang, S., Ashraf, M., et al. (2012). Subcellular preconditioning of stem cells: mito-Cx43 gene targeting is cytoprotective via shift of mitochondrial Bak and Bcl-xL balance. Regenerative Medicine, 7(3), 323–334.
Lu, G., Haider, H. K., Jiang, S., et al. (2009). Sca-1+ stem cell survival and engraftment in the infarcted heart: dual role for preconditioning-induced connexin-43. Circulation, 119(19), 2587–2596.
Wang, D. G., Zhang, F. X., Chen, M. L., et al. (2014). Cx43 in mesenchymal stem cells promotes angiogenesis of the infarcted heart independent of gap junctions. Molecular Medicine Reports, 9(4), 1095–1102.
Roell, W., Lewalter, T., Sasse, P., et al. (2007). Engraftment of connexin 43-expressing cells prevents post-infarct arrhythmia. Nature, 450, 819–824.
Bacova, B., Radosinska, J., Knezl, V., et al. (2010). Omega-3 fatty acids and atorvastatin suppress ventricular fibrillation inducibility in hypertriglyceridemic rat hearts: implication of intracellular coupling protein, connexin-43. Journal of Physiology and Pharmacology, 61(6), 717–723.
Radosinska, J., Bacova, B., Knezl, V., et al. (2013). Dietary omega-3 fatty acids attenuate myocardial arrhythmogenic factors and propensity of the heart to lethal arrhythmias in a rodent model of human essential hypertension. Journal of Hypertension, 31(9), 1876–1885.
Zambrano, S., Blanca, A. J., Ruiz-Armenta, M. V., et al. (2013). L-Carnitine protects against arterial hypertension-related cardiac fibrosis through modulation of PPAR-γ expression. Biochemical Pharmacology, 85(7), 937–944.
Liu, X., Wang, Q. X., Guo, M., et al. (2013). Beneficial effects of pioglitazone on atrial structural and electrical remodeling in vitro cellular models. Journal of Molecular and Cellular Cardiology, 65, 1–8.
Neuhaus, J., Heinrich, M., Schwalenberg, T., et al. (2009). TGF-beta1 inhibits Cx43 expression and formation of functional syncytia in cultured smooth muscle cells from human detrusor. European Urology, 55(2), 491–497.
Surinkaew, S., Kumphune, S., Chattipakorn, S., et al. (2013). Inhibition of p38 MAPK during ischemia, but not reperfusion, effectively attenuates fatal arrhythmia in ischemia/reperfusion heart. Journal of Cardiovascular Pharmacology, 61(2), 133–141.
Zhao, Y., Yu, L., Xu, S., et al. (2011). Down-regulation of connexin43 gap junction by serum deprivation in human endothelial cells was improved by (−)-Epigallocatechin gallate via ERK MAP kinase pathway. Biochemical and Biophysical Research Communications, 404(1), 217–222.
Acknowledgments
This study was supported by Grant [2013]163 from Key Laboratory of Malignant Tumor Molecular Mechanism and Translational Medicine of Guangzhou Bureau of Science and Information Technology; Grant KLB09001 from the Key Laboratory of Malignant Tumor Gene Regulation and Target Therapy of Guangdong Higher Education Institutes; National Natural Science Foundation of China (No: 81070125, 81270213), Science and Technology Foundation in Guangdong Province (No: 2010B031600032, 2014A020211002) and the Fundamental Research Funds for the Central Universities (13ykzd16).
Conflict of Interest
The authors declare no conflicts of interest.
Authors’ Contributions
This work was done by the investigators of the Sun Yat-sen Memorial Hospital of Sun Yat-sen University. The authors took responsibility for all aspects of the reliability and had no differences in data presentation and interpretation. Jingying Hou and Linyun Wang carried out the experiments and drafted the manuscript; Yue Xing, Tianzhu Guo, Shaoxin Zheng and Changqing Zhou participated in the preparation of the animal model, tissue staining, and molecular assay; Jinghui Hou, Hui Huang and Jingfeng Wang provided the technical assistance; Huibao Long, Tingting Zhong and Quanhua Wu participated the statistical analysis; Tong Wang conceived the study and participated in the study design. All the authors have read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Jingying Hou and Dr. Lingyun Wang played equally important roles in the development of the experimental protocol in the interpretation of the results, and in the texture of the present article.
Rights and permissions
About this article
Cite this article
Hou, J., Wang, L., Hou, J. et al. Peroxisome Proliferator-Activated Receptor Gamma Promotes Mesenchymal Stem Cells to Express Connexin43 via the Inhibition of TGF-β1/Smads Signaling in a Rat Model of Myocardial Infarction. Stem Cell Rev and Rep 11, 885–899 (2015). https://doi.org/10.1007/s12015-015-9615-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-015-9615-7