Abstract
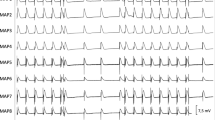
Several case reports suggest QT prolongation leading to ventricular arrhythmias with fatal outcome after intoxication with the μ-opioid receptor agonist and anti-diarrheal agent loperamide. The number of cases of loperamide misuse are growing due to its potential stimulating effects. Loperamide intoxications can be treated by naloxone. However, previous reports described a further QT prolongation associated with naloxone administration. Therefore, the aim of this study was to investigate the effects of loperamide and naloxone on the cardiac electrophysiology in a sensitive whole-heart model. Twenty-six hearts of New Zealand White rabbits were retrogradely perfused in a modified Langendorff apparatus. Monophasic action potentials were recorded by endo- and epicardially positioned catheters. Hearts were stimulated at different cycle lengths, thereby obtaining action potential duration at 90% of repolarization (APD90) and QT intervals. Programmed ventricular stimulation was used to assess ventricular vulnerability. Fourteen hearts were perfused with ascending concentrations of loperamide (0.2 μM, 0.35 μM, and 0.5 μM) after obtaining baseline data. Another 12 hearts were treated with naloxone (0.1 μM, 0.5 μM, 2 μM). Loperamide led to a significant increase in QT interval, APD90, and ventricular tachycardia (VT) episodes. In contrast, naloxone led to a decrease in QT interval and APD90. Accordingly, the number of VT episodes was unaltered. To the best of our knowledge, this is the first experimental study that investigated the effects of loperamide and naloxone in a whole-heart model. Loperamide led to a significant increase in action potential duration and QT interval. Simultaneously, the number of ventricular tachycardias was significantly increased. In contrast, naloxone led to a shortening of the action potential duration without altering arrhythmia susceptibility.




Similar content being viewed by others
References
Daniulaityte, R., Carlson, R., Falck, R., Cameron, D., Perera, S., Chen, L., et al. (2013). “I just wanted to tell you that loperamide WILL WORK”: A web-based study of extra-medical use of loperamide. Drug and Alcohol Dependence, 130(1–3), 241–244.
Teigeler, T., Stahura, H., Alimohammad, R., Kalahasty, G., Koneru, J. N., Ellenbogen, M., et al. (2019). Electrocardiographic changes in loperamide toxicity: Case report and review of literature. Journal of Cardiovascular Electrophysiology, 30(11), 2618–2626.
Enakpene, E. O., Riaz, I. B., Shirazi, F. M., Raz, Y., & Indik, J. H. (2015). The long QT teaser: Loperamide abuse. American Journal of Medicine, 128(10), 1083–1086.
Vaughn, P., Solik, M. M., Bagga, S., & Padanilam, B. J. (2016). Electrocardiographic abnormalities, malignant ventricular arrhythmias, and cardiomyopathy associated with loperamide abuse. Journal of Cardiovascular Electrophysiology, 27(10), 1230–1233.
Sahu, K. K., El Meligy, A., Mishra, A. K., & Goyal, S. (2020). A tale of twists: Loperamide-induced torsades de pointes and ventricular tachycardia storm. BMJ Case Reports, 13(2), e232823.
Kang, J., Compton, D. R., Vaz, R. J., & Rampe, D. (2016). Proarrhythmic mechanisms of the common anti-diarrheal medication loperamide: Revelations from the opioid abuse epidemic. Naunyn Schmiedebergs Arch Pharmacol., 389(10), 1133–1137.
Harmer, A. R., Valentin, J. P., & Pollard, C. E. (2011). On the relationship between block of the cardiac Na(+) channel and drug-induced prolongation of the QRS complex. British Journal of Pharmacology, 164(2), 260–273.
Church, J., Fletcher, E. J., Abdel-Hamid, K., & MacDonald, J. F. (1994). Loperamide blocks high-voltage-activated calcium channels and N-methyl-d-aspartate-evoked responses in rat and mouse cultured hippocampal pyramidal neurons. Molecular Pharmacology, 45(4), 747–757.
Hagiwara, K., Nakagawasai, O., Murata, A., Yamadera, F., Miyoshi, I., Tan-No, K., et al. (2003). Analgesic action of loperamide, an opioid agonist, and its blocking action on voltage-dependent Ca2+ channels. Neuroscience Research, 46(4), 493–497.
Pugsley, M. K., Hayes, E. S., Wang, W. Q., & Walker, M. J. (2015). Ventricular arrhythmia incidence in the rat is reduced by naloxone. Pharmacological Research, 97, 64–69.
Tschirhart, J. N., Li, W., Guo, J., & Zhang, S. (2019). Blockade of the Human Ether A-Go-Go-Related Gene (hERG) potassium channel by fentanyl. Molecular Pharmacology, 95(4), 386–397.
Oldroyd, K. G., Hicks, M. N., & Cobbe, S. M. (1993). Influence of hyperkalaemia and ischaemia on non-receptor-mediated cardiac electrophysiological effects of naloxone. Cardiovascular Research, 27(2), 296–303.
Drolet, B., Simard, C., & Roden, D. M. (2004). Unusual effects of a QT-prolonging drug, arsenic trioxide, on cardiac potassium currents. Circulation, 109(1), 26–29.
Frommeyer, G., Ellermann, C., Dechering, D. G., Kochhauser, S., Bogeholz, N., Guner, F., et al. (2016). Ranolazine and vernakalant prevent ventricular arrhythmias in an experimental whole-heart model of short QT syndrome. Journal of Cardiovascular Electrophysiology, 27(10), 1214–1219.
Okusanya, A., & Li, X. (2018). Loperamide abuse and dependence: Clinical features and treatment considerations. Journal of Addiction Medicine, 12(6), 496–498.
Eggleston, W., Clark, K. H., & Marraffa, J. M. (2017). Loperamide abuse associated with cardiac dysrhythmia and death. Annals of Emergency Medicine, 69(1), 83–86.
Wightman, R. S., Hoffman, R. S., Howland, M. A., Rice, B., Biary, R., & Lugassy, D. (2016). Not your regular high: Cardiac dysrhythmias caused by loperamide. Clinical Toxicology (Philadelphia, PA), 54(5), 454–458.
McDonald, R., Lorch, U., Woodward, J., Bosse, B., Dooner, H., Mundin, G., et al. (2018). Pharmacokinetics of concentrated naloxone nasal spray for opioid overdose reversal: Phase I healthy volunteer study. Addiction, 113(3), 484–493.
Ellermann, C., Wolfes, J., Puckhaber, D., Bogeholz, N., Leitz, P., Lange, P. S., et al. (2019). Digitalis promotes ventricular arrhythmias in flecainide- and ranolazine-pretreated hearts. Cardiovascular Toxicology, 19(3), 237–243.
Osadchii, O. E. (2017). Effects of Na+ channel blockers on the restitution of refractory period, conduction time, and excitation wavelength in perfused guinea-pig heart. PLoS ONE, 12(2), e0172683.
Frommeyer, G., Garthmann, J., Ellermann, C., Dechering, D. G., Kochhauser, S., Reinke, F., et al. (2018). Broad antiarrhythmic effect of mexiletine in different arrhythmia models. Europace, 20(8), 1375–1381.
Valentin, J. P., Hoffmann, P., De Clerck, F., Hammond, T. G., & Hondeghem, L. (2004). Review of the predictive value of the Langendorff heart model (Screenit system) in assessing the proarrhythmic potential of drugs. Journal of Pharmacological and Toxicological Methods, 49(3), 171–181.
Marraffa, J. M., Holland, M. G., Sullivan, R. W., Morgan, B. W., Oakes, J. A., Wiegand, T. J., et al. (2014). Cardiac conduction disturbance after loperamide abuse. Clinical Toxicology (Philadelphia, PA), 52(9), 952–957.
Acknowledgements
This study was supported by the Hans-and-Gertie Fischer Foundation (to G.F.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
Ethical Approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution at which the studies were conducted.
Additional information
Handling editor: Dakshesh Patel.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wolfes, J., Ellermann, C., Burde, S. et al. Divergent Electrophysiological Effects of Loperamide and Naloxone in a Sensitive Whole-Heart Model. Cardiovasc Toxicol 21, 248–254 (2021). https://doi.org/10.1007/s12012-020-09616-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-020-09616-z