Abstract
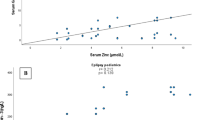
Febrile seizures (FSs) are a common occurrence in young children and a serious concern in pediatric practice; nevertheless, the causes and mechanisms of FS are still unknown. We hypothesized a relation of neuropeptides such as neurotrophin-3 (NT-3) and growth-associated protein-43 (GAP-43) as well as zinc and the oxidant/antioxidant system with pediatric FS. The study included 100 infants categorized into 50 infants with FS and 50 febrile infants without seizures as controls. Clinical assessments, biochemical assays of NT-3 and GAP-43 using ELISA assay kits, and colorimetric measurements of TAC and Zn were performed to all participants. Overall, significant rises of the values of NT-3 and insignificant increases of GAP-43 were detected in children with FS. At the same time, zinc values and the total antioxidant capacity in serum samples were found to be decreased significantly. In addition, a negative correlation was estimated between NT-3 and zinc levels. Serum NT-3 in diagnosing febrile seizures at cutoff point > 49.62 ng/L showed 100% sensitivity, 46% specificity, positive predictive value (PPV) = 48.1%, and negative predictive value (NPP) = 100% with AUC = 0.678. Significant altered circulating NT-3 and zinc levels in FS may indicate their possible role in the pathogenesis of FS. This may open a way for further research and warrants enlightening of the pathophysiological details of FS.



Similar content being viewed by others
Data Availability
The datasets used and analyzed in this study are available upon reasonable request.
References
Paul SP, Blaikley S, Chinthapalli R (2012) Clinical update: febrile convulsion in childhood. Community Pract 85(7):36–38
Paul SP, Eaton M (2013) At a glance febrile convulsion in children. J Fam Health Care 23(1):34-36–7
Laino D, Mencaroni E, Esposito S (2018) Management of pediatric febrile seizures. Int J Environ Res Public Health 15(10):2232. https://doi.org/10.3390/ijerph15102232
Chung S (2014) Febrile seizures. Korean. J Pediatr 57(9):384–395. https://doi.org/10.3345/kjp.2014.57.9.384
Leung AK, Hon KL, Leung TN (2018) Febrile seizures: an overview. Drugs. Context 7:212536. https://doi.org/10.7573/dic.212536
Leung AK (2011) Febrile seizures. In: Leung AK (ed) Common problems in ambulatory pediatrics: specific clinical problems, vol 1. Nova Science Publishers, Inc., New York, NY, pp 199–206
Chiaretti A, Capozzi D, Mariotti P, Valentini P, Manni L, Buonsenso D, Fantacci C, Ferrara P (2014) Increased levels of neurotrophins in the cerebrospinal fluid of children with Epstein-Barr virus meningoencephalitis. Int J Infect Dis 20:52–57. https://doi.org/10.1016/j.ijid.2013.11.006
Klein AB, Williamson R, Santini MA, Clemmensen C, Ettrup A, Rios M, Knudsen GM, Aznar S (2011) Blood BDNF concentrations reflect brain-tissue BDNF levels across species. Int J Neuropsychopharmacol 14(3):347–353. https://doi.org/10.1017/S1461145710000738
Riikonen RS, Söderström S, Korhonen LT, Lindholm DB (1998) Overstimulation of nerve growth factors in postinfectious and autoimmune diseases. Pediatr Neurol 18(3):231–235. https://doi.org/10.1016/s0887-8994(97)00204-x
Oestreicher AB, De Graan PN, Gispen WH, Verhaagen J, Schrama LH (1997) B-50, the growth associated protein-43: modulation of cell morphology and communication in the nervous system. Prog Neurobiol 53(6):627–686. https://doi.org/10.1016/s0301-0082(97)00043-9
Ying Z, Najm I, Nemes A, Pinheiro-Martins AP, Alexopoulos A, Gonzalez-Martinez J (2014) Bingaman W (2014) Growth-associated protein 43 and progressive epilepsy in cortical dysplasia. Ann Clin Transl Neurol 1(7):453–461. https://doi.org/10.1002/acn3.69
Gower-Winter SD, Levenson CW (2012) Zinc in the central nervous system: From molecules to behavior. BioFactors 38(3):186–193. https://doi.org/10.1002/biof.1012
Steering Committee on Quality Improvement and Management, Subcommittee on Febrile Seizures American Academy of Pediatrics (2008) Febrile seizures: clinical practice guideline for the long-term management of the child with simple febrile seizures. Pediatrics 121(6):1281-6. https://doi.org/10.1542/peds.2008-0939
El-Masry HMA, Sadek AA, Hassan MH, Ameen HH, Ahmed HA (2018) Metabolic profile of oxidative stress and trace elements in febrile seizures among children. Metab Brain Dis 33(5):1509–1515. https://doi.org/10.1007/s11011-018-0258-7
Cokyaman T, Kasap T, Şehitoğlu H (2020) Serum brain-derived neurotrophic factor in the diagnosis of febrile seizure. Pediatr Int. https://doi.org/10.1111/ped.14567
Gruber HE, Hoelscher GL, Bethea S, Hanley EN Jr (2012) Interleukin 1-beta upregulates brain-derived neurotrophic factor, neurotrophin 3 and neuropilin 2 gene expression and NGF production in annulus cells. Biotech Histochem 87(8):506–511. https://doi.org/10.3109/10520295.2012.703692
Feng B, Chen Z (2016) Generation of febrile seizures and subsequent epileptogenesis. Neurosci Bull 32(5):481–492. https://doi.org/10.1007/s12264-016-0054-5
Shetty AK, Zaman V, Shetty GA (2003) Hippocampal neurotrophin levels in a kainate model of temporal lobe epilepsy: a lack of correlation between brain-derived neurotrophic factor content and progression of aberrant dentate mossy fiber sprouting. J Neurochem 87(1):147–159. https://doi.org/10.1046/j.1471-4159.2003.01979.x
Denny JB (2006) Molecular mechanisms, biological actions, and neuropharmacology of the growth-associated protein GAP-43. Curr Neuropharmacol 4(4):293–304. https://doi.org/10.2174/157015906778520782
Nemes AD, Ayasoufi K, Ying Z, Zhou QG, Suh H, Najm IM (2017) Growth associated protein 43 (GAP-43) as a novel target for the diagnosis, treatment and prevention of epileptogenesis. Sci Rep 7(1):17702. https://doi.org/10.1038/s41598-017-17377-z
Takeda A (2001) Zinc homeostasis and functions of zinc in the brain. Biometals 14(3–4):343–351. https://doi.org/10.1023/a:1012982123386
Jarosz M, Olbert M, Wyszogrodzka G, Młyniec K, Librowski T (2017) Antioxidant and anti-inflammatory effects of zinc. Zinc-dependent NF-κB signaling Inflammopharmacology 25(1):11–24. https://doi.org/10.1007/s10787-017-0309-4
Arul J, Kommu PPK, Kasinathan A, Ray L, Krishnan L (2020) Zinc status and febrile seizures: results from a cross-sectional study. J Neurosci Rural Pract 11(4):597–600. https://doi.org/10.1055/s-0040-1715992
Heydarian F, Nakhaei AA, Majd HM, Bakhtiari E (2020) Zinc deficiency and febrile seizure: a systematic review and meta-analysis. Turk J Pediatr 62(3):347–358. https://doi.org/10.24953/turkjped.2020.03.001
Funding
This study was partially funded by Faculty of Medicine, South Valley University, Qena83523, Egypt.
Author information
Authors and Affiliations
Contributions
Study concept and design: M. H. H.; patients’ selection and clinical evaluation and follow-up of patients: A. H. B., M. M. M., P. R. H., and N. I. R.; blood sampling and biochemical assays: M. H. H. and S. A. E.-S.; statistical analysis: M. H. H., M. M. M., P. R. H., A. E.-A. A., A. H. B., and S. A. E.-S.; literature research: M. H. H., S. A. E.-S., M. M. M., P. R. H., and N. I. R.; first manuscript drafting: M. H. H.; the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the local Ethics Committee of Medical Research of the Faculty of Medicine, South Valley University, Qena, Egypt (Ethical approval code: SVU-MED-PED-2021–07), and was conducted in accordance with the Declaration of Helsinki. Informed written consent was obtained from every participant’s caregiver.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bakri, A.H., Hassan, M.H., Ahmed, A.EA. et al. Biochemical Assessments of Neurotrophin-3 and Zinc Involvement in the Pathophysiology of Pediatric Febrile Seizures. Biol Trace Elem Res 200, 2614–2619 (2022). https://doi.org/10.1007/s12011-021-02886-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02886-w