Abstract
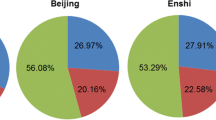
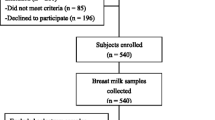
The required selenium intake for optimal health in Chinese residents was published in 2014. However, the adequate intake (AI) value for Chinese infants 0–3 months old is not established. This study assessed the current selenium nutritional status of 264 lactating Chinese women from three geographical locations with different Se levels (Liangshan in Sichuan province, Enshi in Hubei province, and Xicheng District in Beijing), to screen mothers with optimal Se intake, and to modify the AI value of Se for Chinese infants 0–3 months old. Milk and plasma Se concentrations were determined by inductively coupled plasma mass spectrometry (ICP-MS) and glutathione peroxidase 3 (GPx3), and plasma selenoprotein P (SEPP1) was measured by ELISA. Daily Se intake (Y, μg/day) in lactating Chinese woman was calculated from plasma Se concentrations (X, μg/L) using the formula logY = 1.623 log(X) + 3.433. Plasma Se concentrations in lactating Chinese women were 78.19 ± 25.71, 112.48 ± 24.57, and 183.83 ± 45.81 μg/L from Se-deficient, Se-moderate, and seleniferous areas, respectively. Se intakes calculated from concentrations of plasma Se were 45.6 ± 21.69, 80.03 ± 27.69, and 223.10 ± 50.95 μg/day, respectively. An optimal dietary Se intake is not lower than the recommended nutrient intake (RNI) but not more than the tolerable upper intake level (UL). A range of 78–400 μg Se/day was defined as the optimal daily Se intake for lactating Chinese women. The percentages of mothers within this range in Sichuan, Beijing, and Enshi were 8.11, 45.13, and 6.06%, respectively. Based on milk Se concentrations of mothers with optimal daily Se intake, the adequate Se intake value and a safe range for Chinese infants 0–3 months of age were calculated as 15.29 and 8–35 μg Se/day, respectively. The Se status of Chinese lactating women has improved, particularly in traditionally Se-deficient and Se-toxic regions. A safe range for daily Se intake in Chinese infants may be regarded as a guideline for infant formula.


Similar content being viewed by others
References
Chen J (2012) An original discovery: selenium deficiency and Keshan disease (an endemic heart disease). Asia Pac J Clin Nutr 21:320–326. https://doi.org/10.6133/apjcn.2012.21.3.01.
Levander OA (1997) Selenium requirements as discussed in the 1996 joint FAO/IAEA/WHO expert consultation on trace elements in human nutrition. Biomed Environ Sci 10:214–219
Food and Nutrition Board, Institute of Medicine (2000) Dietary Reference Intakes for vitamin C, vitamin E, selenium and carotenoids. National Academies Press, Washington
Kipp AP, Strohm D, Brigelius-Flohé R, Schomburg L, Bechthold A, Leschik-Bonnet E, Heseker H, German Nutrition Society (DGE) (2015) Revised reference values for selenium intake. J Trace Elem Med Biol 32:195–199. https://doi.org/10.1016/j.jtemb.2015.07.005
Hurst R, Collings R, Harvey LJ, King M, Hooper L, Bouwman J, Gurinovic M, Fairweather-Tait SJ (2013) EURRECA—estimating selenium requirements for deriving dietary reference values. Crit Rev Food Sci Nutr 53:1077–1096. https://doi.org/10.1080/10408398.2012.742861
Dodge ML, Wander RC, Xia Y, Butler JA, Wanger PD (1998) Glutathione peroxidase activity modulates fatty acid profiles of plasma and breast milk in Chinese women. J Trace Elem Med Biol 12:221–230. https://doi.org/10.1016/S0946-672X(99)80062-5.
Xia Y, Hill KE, Li P, Xu J, Zhou D, Motley AK, Wang L, Byrne DW, Burk RF (2010) Optimization of selenoprotein P and other plasma selenium biomarkers for the assessment of the selenium nutritional requirement: a placebo-controlled, double-blind study of selenomethionine supplementation in selenium-deficient Chinese subjects. Am J Clin Nutr 92:525–531. https://doi.org/10.3945/ajcn.2010.29642
Hurst R, Armah CN, Dainty JR, Hart DJ, Teucher B, Goldson AJ, Broadley MR, Motley AK, Fairweather-Tait SJ (2010) Establishing optimal selenium status: results of a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 91:923–931. https://doi.org/10.3945/ajcn.2009.28169
Yang GQ, Zhu LZ, Liu SJ, Gu LZ, Qian PC, Huang JH, Lu M-D (1989) Human selenium requirements in China. In: Combs GF Jr, Levander OA, Spallholz JE, Oldfield JE (eds) Selenium in Biology and Medicine. Churchill Livingstone Press, New York, pp 589–607
Duffield AJ, Thomson CD, Hill KE, Williams S (1999) An estimation of selenium requirements for New Zealanders. Am J Clin Nutr 70:896–903. https://doi.org/10.1093/ajcn/70.5.896
Chinese Nutrition Society (2014) Chinese dietary reference intakes (DRIs). Science press, Beijing, pp 250–256 (in Chinese)
Christopher CJ, Fiona MF, Margaret PR (2010) Symposium on ‘Geographical and geological influences on nutrition’ Factor controlling the distribution of selenium in the environment and their impact on health and nutrition. Proc Nutr Soc 69:119–132
Dinh QT, Cui ZW, Huang J, Tran TAT, Wang D, Yang WX, Zhou F, Wang MK, Yu DS, Liang DL (2018) Selenium distribution in the Chinese environment and its relationship with human health. Environ Int 112:294–309
Yang G, Yin S, Zhou R, Gu L, Yan B, Liu Y (1989) Studies of safe maximal daily dietary Se-intake in a seleniferous area in China. Part II: relation between Se-intake and the manifestation of clinical signs and certain biochemical alterations in blood and urine. J Trace Elem Electrolytes Health Dis 3:123–130
Liu X, Piao J, Li M, Zhang Y, Yun C, Yang C and Yang X (2015) Assessment of selenium nutritional status of school-age children from rural areas of China in 2002 and 2012. Euro J Clin Nutr: 1–4. https://doi.org/10.1038/ejcn.2015.194
European Food Safety Authority (EFSA) (2014) Scientific opinion on dietary reference values for selenium EFSA Panel on dietetic products, nutrition and allergies (NDA). EFSA J 10:3846–3913. https://doi.org/10.2903/j.efsa.2014.3846
Levander OA, Moser PB, Morris VC (1987) Dietary selenium intake and selenium concentrations of plasma, erythrocytes, and breast milk in pregnant and postpartum lactating and nonlactating women. Am J Clin Nutr 46:694–698. https://doi.org/10.1093/ajcn/46.4.694
Chen H, Wang P, Han Y, Ma J, Troy FA 2nd, Wang B (2012) Evaluation of dietary intake of lactating women in China and its potential impact on the health of mothers and infants. BMC Womens Health 16:12–18. https://doi.org/10.1186/1472-6874-12-18.
Ning Y, Wang X, Wang S, Zhang F, Zhang L, Lei Y, Guo X (2015) Is it the appropriate time to stop applying selenium enriched salt in Kashin-Beck disease areas in China? Nutrients 7:6195–6212. https://doi.org/10.3390/nu7085276
Wang Q, Sun LC, Liu YQ, Liu JX, Han F, Huang ZW (2016) The synergistic effect of serine with selenocompounds on the expression of SelP and GPx in HepG2 cells. Biol Trace Elem Res 173:291–296. https://doi.org/10.1007/s12011-016-0665-8
Chan SM, Nelson EA, Leung SS, Cheung PC, Li CY (2000) Special postpartum dietary practices of Hong Kong Chinese women. Eur J Clin Nutr 54:797–802. https://doi.org/10.1038/sj.ejcn.1601095
Fowles ER, Walker LO (2006) Correlates of dietary quality and weight retention in postpartum women. J Community Health Nurs 23:183–197. https://doi.org/10.1207/s15327655jchn2303_5
Boghossian NS, Yeung EH, Lipsky LM, Poon AK, Albert PS (2013) Dietary patterns in association with postpartum weight retention. Am J Clin Nutr 97:1338–1345. https://doi.org/10.3945/ajcn.112.048702
Moore MA, Wander RC, Xia YM, Du SH, Butler JA, Whanger PD (2000) Selenium supplementation of Chinese women with habitually low selenium intake increases plasma selenium, plasma glutathione peroxidase activity, and milk selenium, but not milk glutathione peroxidase activity. J Nutr Biochem 11:341–347. https://doi.org/10.1016/S0955-2863(00)00089-9.
Liu X, Piao J, Li M, Zhang Y, Yun C, Yang C, Yang X (2016) Assessment of selenium nutritional status of school-age children from rural areas of China in 2002 and 2012. Eur J Clin Nutr 70:405–408. https://doi.org/10.1038/ejcn.2015.194
Zhou J, Huang K, Lei XG (2013) Selenium and diabetes—evidence from animal studies. Free Radic Biol Med 65:1548–1556. https://doi.org/10.1016/j.freeradbiomed.2013.07.012
Ogawa-Wong AN, Berry MJ, Seale LA (2016) Selenium and metabolic disorders: an emphasis on type 2 diabetes risk. Nutrients 8:80–98. https://doi.org/10.3390/nu8020080
Sasaki S (2008) Dietary reference intakes (DRIs) in Japan. Asia Pac J Clin Nutr 17(Suppl 2):420–444. https://doi.org/10.6133/apjcn.2008.17.s2.07
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2014) Scientific opinion on dietary reference values for selenium. EFSA J 12:3846–3912. https://doi.org/10.2903/j.efsa.2014.3846
National Health and Medical Research Council, Australian Government Department of Health and Ageing, New Zealand ministry of health (2017) Nutrient reference values for Australia and New Zealand including recommended dietary intakes (version 1.2). National Health and Medical Research Council Press, Sydney
Zachara BA, Pilecki A (2000) Selenium concentration in the milk of breast-feeding mothers and its geographic distribution. Environ Health Perspect 108:1043–1046
White L, Romagné F, Müller E, Erlebach E, Weihmann A, Parra G, Andrés AM, Castellano S (2015) Genetic adaptation to levels of dietary selenium in recent human history. Mol Biol Evol 32:1507–1518. https://doi.org/10.1093/molbev/msv043
Lothrop AP, Ruggles EL, Hondal RJ (2009) No selenium required: reactions catalyzed by mammalian thioredoxin reductase that are independent of a selenocysteine residue. Biochemistry 48:6213–6223. https://doi.org/10.1021/bi802146w
Xu XM, Turanov AA, Carlson BA, Yoo MH, Everley RA, Nandakumar R, Sorokina I, Gygi SP, Gladyshev VN, Hatfield DL (2010) Targeted insertion of cysteine by decoding UGA codons with mammalian selenocysteine machinery. Proc Natl Acad Sci U S A 107:21430–21434. https://doi.org/10.1073/pnas.1009947107
Turanov AA, Everley RA, Hybsier S, Renko K, Schomburg L, Gygi SP, Hatfield DL, Gladyshev VN (2015) Regulation of Selenocysteine content of human selenoprotein P by dietary selenium and insertion of cysteine in place of selenocysteine. PLoS One 10:e0140353. https://doi.org/10.1371/journal.pone.0140353
Levander OA (1989) Upper limit of selenium in infant formulas. J Nutr 119:1869–1872
Zeng MS, Li X, Liu Y, Zhao H, Zhou JC, Li K, Huang JQ, Sun LH, Tang JY, Xia XJ, Wang KN, Lei XG (2012) A high-selenium diet induces insulin resistance in gestating rats and their offspring. Free Radic Biol Med 52:1335–1342. https://doi.org/10.1016/j.freeradbiomed.2012.01.017
Funding
This work was financially supported by the Chinese Nutrition Society Nutrition Scientific Research Funds—Yili Nutrition and Health Research Fund (No. 2013-013) and the National Natural Science Foundation of China under the Grant No. 81372989.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The present study was conducted according to guidelines stated in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Ethics Committee of The National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention.
Conflict of Interest
The authors declare no conflict of interests.
Rights and permissions
About this article
Cite this article
Han, F., Liu, L., Lu, J. et al. Calculation of an Adequate Intake (AI) Value and Safe Range of Selenium (Se) for Chinese Infants 0–3 Months Old Based on Se Concentration in the Milk of Lactating Chinese Women with Optimal Se Intake. Biol Trace Elem Res 188, 363–372 (2019). https://doi.org/10.1007/s12011-018-1440-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1440-9