Abstract
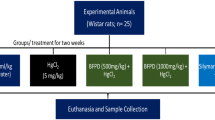
Lead (Pb) exposure is a global environmental problem that can deplete body antioxidant enzymes, causing damage to various macromolecules and ultimately cell death. Pb exposure could lead to serious renal damage. Baicalin, a traditional Chinese medicine, could protect against renal injury through inhibition of oxidative stress and apoptosis. This study was designed to investigate the protective efficacy of baicalin against Pb-induced nephrotoxicity in mice and to elucidate the potential mechanisms using animal experiment. The results revealed that baicalin decreased Pb-induced bodyweight loss, declined kidney coefficients, and ameliorated renal function and structure in a dose-dependent manner. Meanwhile, baicalin dose dependently increased Pb-induced activity of SOD and GSH-Px, while the content of MDA in the kidney was decreased. In addition, baicalin enhanced the Bcl-2/Bax ratio associated with apoptosis in the kidney. These data indicated that further investigation of the use of baicalin as a new natural chemopreventive agent against Pd poisoning is warranted.




Similar content being viewed by others
References
Kim Y, Harada K, Ohmori S, Lee BK, Miura H, Ueda A (1995) Evaluation of lead exposure in workers at a lead-acid battery factory in Korea: with focus on activity of erythrocyte pyrimidine 5′-nucleotidase (P5N). Occup Environ Med 52(7):484–488
DeRosa C (1994) Agency for Toxic Substances and Disease Registry’s toxicological profiles: contribution to public health. Toxicol Ind Health 10(3):117
Fadrowski JJ, Navas-Acien A, Tellez-Plaza M, Guallar E, Weaver VM, Furth SL (2010) Blood lead level and kidney function in US adolescents: the third National Health and Nutrition Examination Survey. Arch Intern Med 170(1):75–82. doi:10.1001/archinternmed.2009.417
Kwon SY, Bae ON, Noh JY, Kim K, Kang S, Shin YJ, Lim KM, Chung JH (2015) Erythrophagocytosis of lead-exposed erythrocytes by renal tubular cells: possible role in lead-induced nephrotoxicity. Environ Health Perspect 123(2):120–127. doi:10.1289/ehp.1408094
Pollack AZ, Mumford SL, Mendola P, Perkins NJ, Rotman Y, Wactawski-Wende J, Schisterman EF (2015) Kidney biomarkers associated with blood lead, mercury, and cadmium in premenopausal women: a prospective cohort study. J Toxic Environ Health Part A 78(2):119–131. doi:10.1080/15287394.2014.944680
Thamilselvan S, Khan SR (1998) Oxalate and calcium oxalate crystals are injurious to renal epithelial cells: results of in vivo and in vitro studies. J Nephrol 11(Suppl 1):66–69
Bokara KK, Brown E, McCormick R, Yallapragada PR, Rajanna S, Bettaiya R (2008) Lead-induced increase in antioxidant enzymes and lipid peroxidation products in developing rat brain. Biometals: Int J Role Metal Ions Biol, Biochem, Med 21(1):9–16. doi:10.1007/s10534-007-9088-5
Alya A, Ines DB, Montassar L, Najoua G, Saloua el F (2015) Oxidative stress, biochemical alterations, and hyperlipidemia in female rats induced by lead chronic toxicity during puberty and post puberty periods. Iranian Journal of Basic Medical Sciences 18(10):1034–1043
He L, Perkins GA, Poblenz AT, Harris JB, Hung M, Ellisman MH, Fox DA (2003) Bcl-xL overexpression blocks bax-mediated mitochondrial contact site formation and apoptosis in rod photoreceptors of lead-exposed mice. Proc Natl Acad Sci U S A 100(3):1022–1027. doi:10.1073/pnas.0333594100
Yuan G, Dai S, Yin Z, Lu H, Jia R, Xu J, Song X, Li L, Shu Y, Zhao X, Chen Z, Fan Q, Liang X, He C, Yin L, Lv C, Lei Q, Wang L, Mi Y, Yu X, Zhang M (2014) Sub-chronic lead and cadmium co-induce apoptosis protein expression in liver and kidney of rats. Int J Clin Exp Pathol 7(6):2905–2914
Patrick L (2006) Lead toxicity part II: the role of free radical damage and the use of antioxidants in the pathology and treatment of lead toxicity. Alternat Med Rev: J Clin Ther 11(2):114–127
Li L, Zhang Y, Ma J, Dong W, Song Q, Zhang J, Chu L (2014) Salvia miltiorrhiza injection ameliorates renal damage induced by lead exposure in mice. TheScientificWorldJOURNAL 2014:572697. doi:10.1155/2014/572697
Azoulay E (2005) Diagnosis and management of pleural effusions in critically ill patients. Rev Mal Respir 22(1 Pt 1):71–79
Flora SJ, Mittal M, Mehta A (2008) Heavy metal induced oxidative stress & its possible reversal by chelation therapy. Indian J Med Res 128(4):501–523
Flora SJ, Pachauri V (2010) Chelation in metal intoxication. Int J Environ Res Public Health 7(7):2745–2788. doi:10.3390/ijerph7072745
Cheng O, Li Z, Han Y, Jiang Q, Yan Y, Cheng K (2012) Baicalin improved the spatial learning ability of global ischemia/reperfusion rats by reducing hippocampal apoptosis. Brain Res 1470:111–118. doi:10.1016/j.brainres.2012.06.026
Cao Y, Mao X, Sun C, Zheng P, Gao J, Wang X, Min D, Sun H, Xie N, Cai J (2011) Baicalin attenuates global cerebral ischemia/reperfusion injury in gerbils via anti-oxidative and anti-apoptotic pathways. Brain Res Bull 85(6):396–402. doi:10.1016/j.brainresbull.2011.05.002
Guo M, Zhang N, Li D, Liang D, Liu Z, Li F, Fu Y, Cao Y, Deng X, Yang Z (2013) Baicalin plays an anti-inflammatory role through reducing nuclear factor-kappaB and p38 phosphorylation in S. aureus-induced mastitis. Int Immunopharmacol 16(2):125–130. doi:10.1016/j.intimp.2013.03.006
Li H, Hu J, Ma L, Yuan Z, Wang Y, Wang X, Xing D, Lei F, Du L (2010) Comprehensive study of baicalin down-regulating NOD2 receptor expression of neurons with oxygen-glucose deprivation in vitro and cerebral ischemia-reperfusion in vivo. Eur J Pharmacol 649(1–3):92–99. doi:10.1016/j.ejphar.2010.09.023
Guo M, Cao Y, Wang T, Song X, Liu Z, Zhou E, Deng X, Zhang N, Yang Z (2014) Baicalin inhibits Staphylococcus aureus-induced apoptosis by regulating TLR2 and TLR2-related apoptotic factors in the mouse mammary glands. Eur J Pharmacol 723:481–488. doi:10.1016/j.ejphar.2013.10.032
Yang B, Jain S, Ashra SY, Furness PN, Nicholson ML (2006) Apoptosis and caspase-3 in long-term renal ischemia/reperfusion injury in rats and divergent effects of immunosuppressants. Transplantation 81(10):1442–1450. doi:10.1097/01.tp.0000209412.77312.69
Liu YZ, Cao YG, Ye JQ, Wang WG, Song KJ, Wang XL, Wang CH, Li RT, Deng XM (2010) Immunomodulatory effects of proanthocyanidin A-1 derived in vitro from Rhododendron spiciferum. Fitoterapia 81(2):108–114. doi:10.1016/j.fitote.2009.08.005
de Burbure C, Buchet JP, Leroyer A, Nisse C, Haguenoer JM, Mutti A, Smerhovsky Z, Cikrt M, Trzcinka-Ochocka M, Razniewska G, Jakubowski M, Bernard A (2006) Renal and neurologic effects of cadmium, lead, mercury, and arsenic in children: evidence of early effects and multiple interactions at environmental exposure levels. Environ Health Perspect 114(4):584–590
Spector JT, Navas-Acien A, Fadrowski J, Guallar E, Jaar B, Weaver VM (2011) Associations of blood lead with estimated glomerular filtration rate using MDRD, CKD-EPI and serum cystatin C-based equations. Nephrol, Dial, Transplant: Off Publ Eur Dial Transpl Assoc—Eur Renal Assoc 26(9):2786–2792. doi:10.1093/ndt/gfq773
Zhang Y, Li H, Zhao Y, Gao Z (2006) Dietary supplementation of baicalin and quercetin attenuates iron overload induced mouse liver injury. Eur J Pharmacol 535(1–3):263–269. doi:10.1016/j.ejphar.2006.01.067
Tang YJ, Zhou FW, Luo ZQ, Li XZ, Yan HM, Wang MJ, Huang FR, Yue SJ (2010) Multiple therapeutic effects of adjunctive baicalin therapy in experimental bacterial meningitis. Inflammation 33(3):180–188. doi:10.1007/s10753-009-9172-9
Zhang XP, Tian H, Lai YH, Chen L, Zhang L, Cheng QH, Yan W, Li Y, Li QY, He Q, Wang F (2007) Protective effects and mechanisms of baicalin and octreotide on renal injury of rats with severe acute pancreatitis. World J Gastroenterol: WJG 13(38):5079–5089
Ademuyiwa O, Agarwal R, Chandra R, Behari JR (2009) Lead-induced phospholipidosis and cholesterogenesis in rat tissues. Chem Biol Interact 179(2–3):314–320. doi:10.1016/j.cbi.2008.10.057
Pal PB, Sinha K, Sil PC (2013) Mangiferin, a natural xanthone, protects murine liver in Pb(II) induced hepatic damage and cell death via MAP kinase, NF-kappaB and mitochondria dependent pathways. PLoS One 8(2):e56894. doi:10.1371/journal.pone.0056894
Kaur G, Singh HP, Batish DR, Mahajan P, Kohli RK, Rishi V (2015) Exogenous nitric oxide (NO) interferes with lead (Pb)-induced toxicity by detoxifying reactive oxygen species in hydroponically grown wheat (Triticum aestivum) roots. PLoS One 10(9):e0138713. doi:10.1371/journal.pone.0138713
Lakshmi SV, Padmaja G, Kuppusamy P, Kutala VK (2009) Oxidative stress in cardiovascular disease. Indian J Biochem Biophys 46(6):421–440
Zhang J, Gu HD, Zhang L, Tian ZJ, Zhang ZQ, Shi XC, Ma WH (2011) Protective effects of apricot kernel oil on myocardium against ischemia-reperfusion injury in rats. Food Chem Toxicol: Int J Publ Br Ind Biol Res Assoc 49(12):3136–3141. doi:10.1016/j.fct.2011.08.015
Anand KV, Mohamed Jaabir MS, Thomas PA, Geraldine P (2012) Protective role of chrysin against oxidative stress in d-galactose-induced aging in an experimental rat model. Geriatr Gerontol Int 12(4):741–750. doi:10.1111/j.1447-0594.2012.00843.x
Sharpe PC, Liu WH, Yue KK, McMaster D, Catherwood MA, McGinty AM, Trimble ER (1998) Glucose-induced oxidative stress in vascular contractile cells: comparison of aortic smooth muscle cells and retinal pericytes. Diabetes 47(5):801–809
Hsu PC, Guo YL (2002) Antioxidant nutrients and lead toxicity. Toxicology 180(1):33–44
Liu M, Xu Y, Han X, Liang C, Yin L, Xu L, Qi Y, Zhao Y, Peng J, Sun C (2014) Potent effects of flavonoid-rich extract from Rosa laevigata Michx fruit against hydrogen peroxide-induced damage in PC12 cells via attenuation of oxidative stress, inflammation and apoptosis. Molecules 19(8):11816–11832. doi:10.3390/molecules190811816
Shen M, Lin F, Zhang J, Tang Y, Chen WK, Liu H (2012) Involvement of the up-regulated FoxO1 expression in follicular granulosa cell apoptosis induced by oxidative stress. J Biol Chem 287(31):25727–25740. doi:10.1074/jbc.M112.349902
Faghiri Z, Bazan NG (2010) PI3K/Akt and mTOR/p70S6K pathways mediate neuroprotectin D1-induced retinal pigment epithelial cell survival during oxidative stress-induced apoptosis. Exp Eye Res 90(6):718–725. doi:10.1016/j.exer.2010.03.002
Jazvinscak Jembrek M, Hof PR, Simic G (2015) Ceramides in Alzheimer’s disease: key mediators of neuronal apoptosis induced by oxidative stress and Abeta accumulation. Oxidative Med Cell Longev 2015:346783. doi:10.1155/2015/346783
Kroemer G (1997) The proto-oncogene Bcl-2 and its role in regulating apoptosis. Nat Med 3(6):614–620
Osorio LM, De Santiago A, Aguilar-Santelises M, Mellstedt H, Jondal M (1997) CD6 ligation modulates the Bcl-2/Bax ratio and protects chronic lymphocytic leukemia B cells from apoptosis induced by anti-IgM. Blood 89(8):2833–2841
Shi L, Chen J, Yang J, Pan T, Zhang S, Wang Z (2010) MiR-21 protected human glioblastoma U87MG cells from chemotherapeutic drug temozolomide induced apoptosis by decreasing Bax/Bcl-2 ratio and caspase-3 activity. Brain Res 1352:255–264. doi:10.1016/j.brainres.2010.07.009
Lin M, Li L, Li L, Pokhrel G, Qi G, Rong R, Zhu T (2014) The protective effect of baicalin against renal ischemia-reperfusion injury through inhibition of inflammation and apoptosis. BMC Complement Alternat Med 14:19. doi:10.1186/1472-6882-14-19
Acknowledgments
This work was supported by a grant from the National Natural Science Foundation of China (Nos. 31272622 and 31472248) and Jilin Province Science Foundation for Youths (No. 20130522087JH).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All of the animal studies were conducted in accordance with the experimental practices and standards that were approved by the Animal Welfare and Research Ethics Committee at Jilin University under the approved protocol number JLUA-1309. The protocols were reviewed and approved by the committee. All of the animal studies were performed under isoflurane anesthesia.
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Zhang, Z., Gao, X., Guo, M. et al. The Protective Effect of Baicalin Against Lead-Induced Renal Oxidative Damage in Mice. Biol Trace Elem Res 175, 129–135 (2017). https://doi.org/10.1007/s12011-016-0731-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-016-0731-2