Abstract
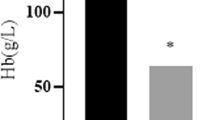
Studies have shown that men and women exhibit significant differences regarding iron status. However, the effects of sex on iron accumulation and distribution are not well established. In this study, female and male Sprague-Dawley rats were killed at 4 months of age. Blood samples were analyzed to determine the red blood cell (RBC) count, hemoglobin (Hb) concentration, hematocrit (Hct), and mean red blood cell volume (MCV). The serum samples were analyzed to determine the concentrations of serum iron (SI), transferrin saturation (TS), ferritin, soluble transferrin receptor (sTfR), and erythropoietin (EPO). The tissue nonheme iron concentrations were measured in the liver, spleen, bone marrow, kidney, heart, gastrocnemius, duodenal epithelium, lung, pallium, cerebellum, hippocampus, and striatum. Hepatic hepcidin expression was detected by real-time PCR analysis. The synthesis of ferroportin 1 (FPN1) in the liver, spleen, kidney, and bone marrow was determined by Western blot analysis. The synthesis of duodenal cytochrome B561 (DcytB), divalent metal transporter 1 (DMT1), FPN1, hephaestin (HP) in the duodenal epithelium was also measured by Western blot analysis. The results showed that the RBC, Hb, and Hct in male rats were higher than those in female rats. The SI and plasma TS levels were lower in male rats than in female rats. The levels of serum ferritin and sTfR were higher in male rats than in female rats. The EPO levels in male rats were lower than that in female rats. The nonheme iron contents in the liver, spleen, bone marrow, and kidney in male rats were also lower (56.7, 73.2, 60.6, and 61.4 % of female rats, respectively). Nonheme iron concentrations in the heart, gastrocnemius, duodenal epithelium, lung, and brain were similar in rats of both sexes. A moderate decrease in hepatic hepcidin mRNA content was also observed in male rats (to 56.0 % of female rats). The levels of FPN1 protein in the liver, spleen, and kidney were higher in male rats than in female rats. There was no significant change in FPN1 expression in bone marrow. Significant difference was also not found in DcytB, DMT1, FPN1, and HP protein levels in the duodenal epithelium between male and female rats. These data suggest that iron is distributed differently in male and female rats. This difference in iron distribution may be associated with the difference in the hepcidin level.




Similar content being viewed by others
References
von Drygalski A, Adamson JW (2012) Iron metabolism in man. JPEN J Parenter Enteral Nutr. doi:10.1177/0148607112459648
Tatala S, Svanberg U, Mduma B (1998) Low dietary iron availability is a major cause of anemia: a nutrition survey in the Lindi District of Tanzania. Am J Clin Nutr 68(1):171–178
Huang J, Jones D, Luo B, Sanderson M, Soto J, Abel ED, Cooksey RC, McClain DA (2011) Iron overload and diabetes risk: a shift from glucose to Fatty Acid oxidation and increased hepatic glucose production in a mouse model of hereditary hemochromatosis. Diabetes 60(1):80–87. doi:10.2337/db10-0593
Valenti L, Fracanzani AL, Rossi V, Rampini C, Pulixi E, Varenna M, Fargion S, Sinigaglia L (2008) The hand arthropathy of hereditary hemochromatosis is strongly associated with iron overload. J Rheumatol 35(1):153–158
Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL (1997) Prevalence of iron deficiency in the United States. JAMA 277(12):973–976
Wagnerberger S, Schafer C, Schwarz E, Bode C, Parlesak A (2008) Is nutrient intake a gender-specific cause for enhanced susceptibility to alcohol-induced liver disease in women? Alcohol Alcohol 43(1):9–14. doi:10.1093/alcalc/agm161
Harrison-Findik DD (2010) Gender-related variations in iron metabolism and liver diseases. World J Hepatol 2(8):302–310. doi:10.4254/wjh.v2.i8.302
Dekker LH, Nicolaou M, van der Daphne AD, Busschers WB, Brewster LM, Snijder MB, Stronks K, van Valkengoed IG (2013) Sex Differences in the Association Between Serum Ferritin and Fasting Glucose in Type 2 Diabetes Among South Asian Surinamese, African Surinamese, and Ethnic Dutch: The population-based SUNSET study. Diabetes Care 36(4):965–971. doi:10.2337/dc12-1243
Tamura T, Hou J, Goldenberg RL, Johnston KE, Cliver SP (1999) Gender difference in cord serum ferritin concentrations. Biol Neonate 75(6):343–349
Domellof M, Lonnerdal B, Dewey KG, Cohen RJ, Rivera LL, Hernell O (2002) Sex differences in iron status during infancy. Pediatrics 110(3):545–552
Wieringa FT, Berger J, Dijkhuizen MA, Hidayat A, Ninh NX, Utomo B, Wasantwisut E, Winichagoon P (2007) Sex differences in prevalence of anaemia and iron deficiency in infancy in a large multi-country trial in South-East Asia. Br J Nutr 98(5):1070–1076. doi:10.1017/S0007114507756945
Bergstrom E, Hernell O, Lonnerdal B, Persson LA (1995) Sex differences in iron stores of adolescents: what is normal? J Pediatr Gastroenterol Nutr 20(2):215–224
Ganz T, Olbina G, Girelli D, Nemeth E, Westerman M (2008) Immunoassay for human serum hepcidin. Blood 112(10):4292–4297. doi:10.1182/blood-2008-02-139915
Jian J, Pelle E, Huang X (2009) Iron and menopause: does increased iron affect the health of postmenopausal women? Antioxid Redox Signal 11(12):2939–2943. doi:10.1089/ARS.2009.2576
Heath AL, Skeaff CM, Williams S, Gibson RS (2001) The role of blood loss and diet in the aetiology of mild iron deficiency in premenopausal adult New Zealand women. Public Health Nutr 4(2):197–206
Park CH, Valore EV, Waring AJ, Ganz T (2001) Hepcidin, a urinary antimicrobial peptide synthesized in the liver. J Biol Chem 276(11):7806–7810. doi:10.1074/jbc.M008922200
Ganz T (2011) Hepcidin and iron regulation, 10 years later. Blood 117(17):4425–4433. doi:10.1182/blood-2011-01-258467
Wang SM, Fu LJ, Duan XL, Crooks DR, Yu P, Qian ZM, Di XJ, Li J, Rouault TA, Chang YZ (2010) Role of hepcidin in murine brain iron metabolism. Cell Mol Life Sci CMLS 67(1):123–133. doi:10.1007/s00018-009-0167-3
Guo P, Cui R, Chang YZ, Wu WS, Qian ZM, Yoshida K, Qiao YT, Takeda S, Duan XL (2009) Hepcidin, an antimicrobial peptide is downregulated in ceruloplasmin-deficient mice. Peptides 30(2):262–266. doi:10.1016/j.peptides.2008.09.017
Liu YQ, Chang YZ, Zhao B, Wang HT, Duan XL (2011) Does hepatic hepcidin play an important role in exercise-associated anemia in rats? Int J Sport Nutr Exerc Metab 21(1):19–26
Jaeggi T, Moretti D, Kvalsvig J, Holding PA, Tjalsma H, Kortman GA, Joosten I, Mwangi A, Zimmermann MB (2013) Iron status and systemic inflammation, but not gut inflammation, strongly predict gender-specific concentrations of serum hepcidin in infants in rural Kenya. PLoS One 8(2):e57513. doi:10.1371/journal.pone.0057513
McKie AT, Barrow D, Latunde-Dada GO, Rolfs A, Sager G, Mudaly E, Mudaly M, Richardson C, Barlow D, Bomford A, Peters TJ, Raja KB, Shirali S, Hediger MA, Farzaneh F, Simpson RJ (2001) An iron-regulated ferric reductase associated with the absorption of dietary iron. Science 291(5509):1755–1759. doi:10.1126/science.1057206
Gunshin H, Mackenzie B, Berger UV, Gunshin Y, Romero MF, Boron WF, Nussberger S, Gollan JL, Hediger MA (1997) Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature 388(6641):482–488. doi:10.1038/41343
Fleming MD, Romano MA, Su MA, Garrick LM, Garrick MD, Andrews NC (1998) Nramp2 is mutated in the anemic Belgrade (b) rat: evidence of a role for Nramp2 in endosomal iron transport. Proc Natl Acad Sci U S A 95(3):1148–1153
Donovan A, Brownlie A, Zhou Y, Shepard J, Pratt SJ, Moynihan J, Paw BH, Drejer A, Barut B, Zapata A, Law TC, Brugnara C, Lux SE, Pinkus GS, Pinkus JL, Kingsley PD, Palis J, Fleming MD, Andrews NC, Zon LI (2000) Positional cloning of zebrafish ferroportin1 identifies a conserved vertebrate iron exporter. Nature 403(6771):776–781. doi:10.1038/35001596
Vulpe CD, Kuo YM, Murphy TL, Cowley L, Askwith C, Libina N, Gitschier J, Anderson GJ (1999) Hephaestin, a ceruloplasmin homologue implicated in intestinal iron transport, is defective in the sla mouse. Nat Genet 21(2):195–199. doi:10.1038/5979
Chang YZ, Qian ZM, Du JR, Zhu L, Xu Y, Li LZ, Wang CY, Wang Q, Ge XH, Ho KP, Niu L, Ke Y (2007) Ceruloplasmin expression and its role in iron transport in C6 cells. Neurochem Int 50(5):726–733. doi:10.1016/j.neuint.2007.01.004
Liu YQ, Duan XL, Chang YZ, Wang HT, Qian ZM (2006) Molecular analysis of increased iron status in moderately exercised rats. Mol Cell Biochem 282(1–2):117–123. doi:10.1007/s11010-006-1522-4
Kong WN, Zhao SE, Duan XL, Yang Z, Qian ZM, Chang YZ (2008) Decreased DMT1 and increased ferroportin 1 expression is the mechanisms of reduced iron retention in macrophages by erythropoietin in rats. J Cell Biochem 104(2):629–641. doi:10.1002/jcb.21654
Kong WN, Chang YZ, Wang SM, Zhai XL, Shang JX, Li LX, Duan XL (2008) Effect of erythropoietin on hepcidin, DMT1 with IRE, and hephaestin gene expression in duodenum of rats. J Gastroenterol 43(2):136–143. doi:10.1007/s00535-007-2138-5
Qian ZM, Xiao DS, Tang PL, Yao FY, Liao QK (1999) Increased expression of transferrin receptor on membrane of erythroblasts in strenuously exercised rats. J Appl Physiol 87(2):523–529
Sheikh N, Batusic DS, Dudas J, Tron K, Neubauer K, Saile B, Ramadori G (2006) Hepcidin and hemojuvelin gene expression in rat liver damage: in vivo and in vitro studies. Am J Physiol Gastrointest Liver Physiol 291(3):G482–G490. doi:10.1152/ajpgi.00586.2005
Levy JE, Jin O, Fujiwara Y, Kuo F, Andrews NC (1999) Transferrin receptor is necessary for development of erythrocytes and the nervous system. Nat Genet 21(4):396–399. doi:10.1038/7727
Cooperman SS, Meyron-Holtz EG, Olivierre-Wilson H, Ghosh MC, McConnell JP, Rouault TA (2005) Microcytic anemia, erythropoietic protoporphyria, and neurodegeneration in mice with targeted deletion of iron-regulatory protein 2. Blood 106(3):1084–1091. doi:10.1182/blood-2004-12-4703
Shintani N, Kohgo Y, Kato J, Kondo H, Fujikawa K, Miyazaki E, Niitsu Y (1994) Expression and extracellular release of transferrin receptors during peripheral erythroid progenitor cell differentiation in liquid culture. Blood 83(5):1209–1215
R'Zik S, Loo M, Beguin Y (2001) Reticulocyte transferrin receptor (TfR) expression and contribution to soluble TfR levels. Haematologica 86(3):244–251
Coviello AD, Kaplan B, Lakshman KM, Chen T, Singh AB, Bhasin S (2008) Effects of graded doses of testosterone on erythropoiesis in healthy young and older men. J Clin Endocrinol Metab 93(3):914–919. doi:10.1210/jc.2007-1692
Guo W, Bachman E, Li M, Roy CN, Blusztajn J, Wong S, Chan SY, Serra C, Jasuja R, Travison TG, Muckenthaler MU, Nemeth E, Bhasin S (2013) Testosterone administration inhibits hepcidin transcription and is associated with increased iron incorporation into red blood cells. Aging Cell 12(2):280–291. doi:10.1111/acel.12052
Fonseca R, Rajkumar SV, White WL, Tefferi A, Hoagland HC (1998) Anemia after orchiectomy. Am J Hematol 59(3):230–233
Tran TN, Eubanks SK, Schaffer KJ, Zhou CY, Linder MC (1997) Secretion of ferritin by rat hepatoma cells and its regulation by inflammatory cytokines and iron. Blood 90(12):4979–4986
Prieto J, Barry M, Sherlock S (1975) Serum ferritin in patients with iron overload and with acute and chronic liver diseases. Gastroenterology 68(3):525–533
Courselaud B, Troadec MB, Fruchon S, Ilyin G, Borot N, Leroyer P, Coppin H, Brissot P, Roth MP, Loreal O (2004) Strain and gender modulate hepatic hepcidin 1 and 2 mRNA expression in mice. Blood Cells Mol Dis 32(2):283–289. doi:10.1016/j.bcmd.2003.11.003
Xu X, Wang Q, Zhang M (2008) Age, gender, and hemispheric differences in iron deposition in the human brain: an in vivo MRI study. NeuroImage 40(1):35–42. doi:10.1016/j.neuroimage.2007.11.017
Nicolas G, Chauvet C, Viatte L, Danan JL, Bigard X, Devaux I, Beaumont C, Kahn A, Vaulont S (2002) The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J Clin Invest 110(7):1037–1044. doi:10.1172/JCI15686
Mastrogiannaki M, Matak P, Mathieu JR, Delga S, Mayeux P, Vaulont S, Peyssonnaux C (2012) Hepatic hypoxia-inducible factor-2 down-regulates hepcidin expression in mice through an erythropoietin-mediated increase in erythropoiesis. Haematologica 97(6):827–834. doi:10.3324/haematol.2011.056119
Ganz T, Nemeth E (2012) Hepcidin and iron homeostasis. Biochim Biophys Acta 1823(9):1434–1443. doi:10.1016/j.bbamcr.2012.01.014
Knutson M, Wessling-Resnick M (2003) Iron metabolism in the reticuloendothelial system. Crit Rev Biochem Mol Biol 38(1):61–88. doi:10.1080/713609210
Knutson MD, Oukka M, Koss LM, Aydemir F, Wessling-Resnick M (2005) Iron release from macrophages after erythrophagocytosis is up-regulated by ferroportin 1 overexpression and down-regulated by hepcidin. Proc Natl Acad Sci U S A 102(5):1324–1328. doi:10.1073/pnas.0409409102
Delaby C, Pilard N, Goncalves AS, Beaumont C, Canonne-Hergaux F (2005) Presence of the iron exporter ferroportin at the plasma membrane of macrophages is enhanced by iron loading and down-regulated by hepcidin. Blood 106(12):3979–3984. doi:10.1182/blood-2005-06-2398
Ramey G, Deschemin JC, Durel B, Canonne-Hergaux F, Nicolas G, Vaulont S (2010) Hepcidin targets ferroportin for degradation in hepatocytes. Haematologica 95(3):501–504. doi:10.3324/haematol.2009.014399
Chaston T, Chung B, Mascarenhas M, Marks J, Patel B, Srai SK, Sharp P (2008) Evidence for differential effects of hepcidin in macrophages and intestinal epithelial cells. Gut 57(3):374–382. doi:10.1136/gut.2007.131722
Teruel JL, Cano T, Marcen R, Villafruela JJ, Rivera M, Fernandez-Juarez G, Ortuno J (1997) Decrease in the haemoglobin level in haemodialysis patients undergoing antiandrogen therapy. Nephrol Dial Transplant Off Publ Eur Dial Transplant Assoc Eur Renal Assoc 12(6):1262–1263
Vokurka M, Krijt J, Sulc K, Necas E (2006) Hepcidin mRNA levels in mouse liver respond to inhibition of erythropoiesis. Physiol Res Acad Scie Bohemoslovaca 55(6):667–674
Pak M, Lopez MA, Gabayan V, Ganz T, Rivera S (2006) Suppression of hepcidin during anemia requires erythropoietic activity. Blood 108(12):3730–3735. doi:10.1182/blood-2006-06-028787
Weiss G, Houston T, Kastner S, Johrer K, Grunewald K, Brock JH (1997) Regulation of cellular iron metabolism by erythropoietin: activation of iron-regulatory protein and upregulation of transferrin receptor expression in erythroid cells. Blood 89(2):680–687
Corradini E, Garuti C, Montosi G, Ventura P, Andriopoulos B Jr, Lin HY, Pietrangelo A, Babitt JL (2009) Bone morphogenetic protein signaling is impaired in an HFE knockout mouse model of hemochromatosis. Gastroenterology 137(4):1489–1497. doi:10.1053/j.gastro.2009.06.057
Papanikolaou G, Samuels ME, Ludwig EH, MacDonald ML, Franchini PL, Dube MP, Andres L, MacFarlane J, Sakellaropoulos N, Politou M, Nemeth E, Thompson J, Risler JK, Zaborowska C, Babakaiff R, Radomski CC, Pape TD, Davidas O, Christakis J, Brissot P, Lockitch G, Ganz T, Hayden MR, Goldberg YP (2004) Mutations in HFE2 cause iron overload in chromosome 1q-linked juvenile hemochromatosis. Nat Genet 36(1):77–82. doi:10.1038/ng1274
Kawabata H, Fleming RE, Gui D, Moon SY, Saitoh T, O'Kelly J, Umehara Y, Wano Y, Said JW, Koeffler HP (2005) Expression of hepcidin is down-regulated in TfR2 mutant mice manifesting a phenotype of hereditary hemochromatosis. Blood 105(1):376–381. doi:10.1182/blood-2004-04-1416
Wallace DF, Summerville L, Crampton EM, Frazer DM, Anderson GJ, Subramaniam VN (2009) Combined deletion of Hfe and transferrin receptor 2 in mice leads to marked dysregulation of hepcidin and iron overload. Hepatology 50(6):1992–2000. doi:10.1002/hep.23198
Nemeth E, Roetto A, Garozzo G, Ganz T, Camaschella C (2005) Hepcidin is decreased in TFR2 hemochromatosis. Blood 105(4):1803–1806. doi:10.1182/blood-2004-08-3042
Niederkofler V, Salie R, Arber S (2005) Hemojuvelin is essential for dietary iron sensing, and its mutation leads to severe iron overload. J Clin Invest 115(8):2180–2186. doi:10.1172/JCI25683
Babitt JL, Huang FW, Wrighting DM, Xia Y, Sidis Y, Samad TA, Campagna JA, Chung RT, Schneyer AL, Woolf CJ, Andrews NC, Lin HY (2006) Bone morphogenetic protein signaling by hemojuvelin regulates hepcidin expression. Nat Genet 38(5):531–539. doi:10.1038/ng1777
Ramey G, Deschemin JC, Vaulont S (2009) Cross-talk between the mitogen activated protein kinase and bone morphogenetic protein/hemojuvelin pathways is required for the induction of hepcidin by holotransferrin in primary mouse hepatocytes. Haematologica 94(6):765–772. doi:10.3324/haematol.2008.003541
Lin L, Valore EV, Nemeth E, Goodnough JB, Gabayan V, Ganz T (2007) Iron transferrin regulates hepcidin synthesis in primary hepatocyte culture through hemojuvelin and BMP2/4. Blood 110(6):2182–2189. doi:10.1182/blood-2007-04-087593
Ramos E, Kautz L, Rodriguez R, Hansen M, Gabayan V, Ginzburg Y, Roth MP, Nemeth E, Ganz T (2011) Evidence for distinct pathways of hepcidin regulation by acute and chronic iron loading in mice. Hepatology 53(4):1333–1341. doi:10.1002/hep.24178
Corradini E, Meynard D, Wu Q, Chen S, Ventura P, Pietrangelo A, Babitt JL (2011) Serum and liver iron differently regulate the bone morphogenetic protein 6 (BMP6)-SMAD signaling pathway in mice. Hepatology 54(1):273–284. doi:10.1002/hep.24359
Meynard D, Kautz L, Darnaud V, Canonne-Hergaux F, Coppin H, Roth MP (2009) Lack of the bone morphogenetic protein BMP6 induces massive iron overload. Nat Genet 41(4):478–481. doi:10.1038/ng.320
Krijt J, Niederkofler V, Salie R, Sefc L, Pelichovska T, Vokurka M, Necas E (2007) Effect of phlebotomy on hepcidin expression in hemojuvelin-mutant mice. Blood Cells Mol Dis 39(1):92–95. doi:10.1016/j.bcmd.2007.02.004
Ikeda Y, Tajima S, Izawa-Ishizawa Y, Kihira Y, Ishizawa K, Tomita S, Tsuchiya K, Tamaki T (2012) Estrogen regulates hepcidin expression via GPR30-BMP6-dependent signaling in hepatocytes. PLoS One 7(7):e40465. doi:10.1371/journal.pone.0040465
Bachman E, Feng R, Travison T, Li M, Olbina G, Ostland V, Ulloor J, Zhang A, Basaria S, Ganz T, Westerman M, Bhasin S (2010) Testosterone suppresses hepcidin in men: a potential mechanism for testosterone-induced erythrocytosis. J Clin Endocrinol Metab 95(10):4743–4747. doi:10.1210/jc.2010-0864
Latour C, Kautz L, Besson-Fournier C, Island ML, Canonne-Hergaux F, Loreal O, Ganz T, Coppin H, Roth MP (2013) Testosterone perturbs systemic iron balance through activation of EGFR signaling in the liver and repression of hepcidin. Hepatology. doi:10.1002/hep.26648
Acknowledgments
This project was supported by the National Natural Science Foundation of China (contract grant number, 10979025), the Natural Science Foundation of Hebei Province (contract grant number, C2012205082), and the Scientific Research Fund of Hebei Provincial Education Department (contract grant number, Q2012036).
Conflict of Interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Wei-Na Kong and Qiao-Man Niu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kong, WN., Niu, QM., Ge, L. et al. Sex Differences in Iron Status and Hepcidin Expression in Rats. Biol Trace Elem Res 160, 258–267 (2014). https://doi.org/10.1007/s12011-014-0051-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-014-0051-3