Abstract
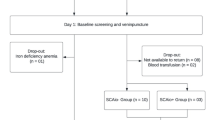
Although a 40 % absorption of a standard reference dose corresponds to iron (Fe) absorption in borderline Fe-deficient subjects, this percentage is currently applied to all subjects independent of Fe status: (a) to assess the use of the 40 % of Fe absorption of the reference dose (FeRD%) for subjects with iron-depleted stores (IDS), normal Fe status (NIS), Fe deficiency without anemia (IDWA), and Fe deficiency anemia (IDA) and (b) to explore relationships between Fe status biomarkers and FeRD%. Six hundred forty-six participants (582 women and 64 men) were selected from multiple Fe bioavailability studies and classified into four groups based on Fe status: NIS, IDS, IDWA, and IDA. All men were classified as normal. The absorption from FeRD% was calculated in each group and correlated with Fe status biomarkers. (a) Women with IDS absorbed 40 (18.9–84.7) % of the reference dose; (b) for male subjects with NIS, the absorption of the reference dose was 19 (9.8–36.1) %, while for females, absorption was observed as to be 34 (16.7–68.6)%. In the case of subjects with IDWA, a 43 (19.7–92.5) % absorption was observed, while subjects with IDA demonstrated 67 (45.2–98.6) % absorption. Serum ferritin (SF) had the strongest inverse correlation with FeRD% (r = −0.41, p < 0.001). A transferrin saturation (TS) <15 % increases the probability that the FeRD% will be highly elevated (OR, 5.05; 95 % CI, 2.73, 9.31; p < 0.001). A 40 % absorption as reference dose is only appropriate to assess Fe absorption in subjects with IDS and IDWA. SF had an inverse correlation with FeRD%, and TS increases the probability that the FeRD% will be elevated by over fivefold.

Similar content being viewed by others
References
Olivares M, Walter T, Hertrampf E, Pizarro F (1999) Anaemia and iron deficiency disease in children. Br Med Bull 55:534–543
DeMaeyer E, Adiels-Tegman M (1985) The prevalence of anaemia in the world. World Health Stat Q 38:302–316
World Health Organization (2001) Iron deficiency anemia: assessment, prevention and control. A guide for programme managers. Document WHO/NHD/01.3. Geneva, Switzerland.
Pan American Health Organization (2001) Iron fortification: guidelines and recommendations for Latin America and the Caribbean. Pan American Health Organization, Washington, DC
Layrisse M, Cook J, Martinez-Torres C, Roche M, Kuhn I, Walker R et al (1969) Food iron absorption: a comparison of vegetable and animal foods. Blood 33:430–443
Magnusson B, Bjorn-Rasmussen E, Hallberg L, Rossander L (1981) Iron absorption in relation to iron status. Model proposed to express results of food iron absorption measurement. Scand J Hematol 27:201–208
Eakins J, Brown D (1966) An improved method for the simultaneous determination of iron-55 and iron-59 in blood by liquid scintillation counting. Int J Appl Radiact Isotopes 17:191–197
Bothwell T, Finch C (1962) Iron metabolism. Little Brown, Boston
Nadler S, Hidalgo J, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51:224–232
Fischer D, Price D (1964) A simple serum iron method using the new sensitive chromogen tripiridyl-s-triasine. Clin Chem 10:21–31
International Anemia Consultative Group (1985) Measurement of iron status: a report of the International Anemia Consultative Group. The Nutrition Foundation, Washington, DC
Centers for Disease Control and Prevention CDC (1998) Recommendations to prevent and control iron deficiency in the United States. MMWR 47:3
Hallberg L (1981) Bioavailability of dietary iron in man. Annu Rev Nutr 1:123–147
Cook J, Dassenko S, Lynch S (1991) Assessment of the role of non heme iron availability in iron balance. Am J Clin Nutr 54:717–722
Fairweather-Tait S (2001) Bioavailability of nutrients and other bioactive components from dietary supplements. J Nutr 131:1383–1386
WHO, UNU, UNICEF (1993) Master Protocol. Population studies of the relative effectiveness of weekly and daily iron supplementation in pregnant women, adolescent girls, and preschool age children. Geneva.
Hallberg L, Brune M, Rossander L (1989) Iron absorption in man: ascorbic acid and dose-dependent inhibition by phytate. Am J Clin Nutr 49:140–144
Olivares M, Pizarro F, Pineda O, Name J, Hertrampf E, Walter T (1997) Milk inhibits and ascorbic acid favors ferrous bis-glycine chelate bioavailability in humans. J Nutr 7:1407–1411
Murray-Kolb L, Welch R, Theil E, Beard J (2003) Women with low iron stores absorb iron from soybeans. Am J Clin Nutr 77:180–184
Disler P, Lynch S, Charlton R, Torrance J, Bothwell T, Walker B, Mayet F (1975) The effect of tea on iron absorption. Gut 16:193–200
Monsen E, Hallberg L, Layrisse M, Hegsted D, Cook J, Mertz W (1978) Estimation of available dietary iron. Am J Clin Nutr 31:134–141
Monsen E, Balintfy J (1982) Calculating dietary iron bioavailability, refinement and computerization. J Am Diet Assoc 80:307–311
Tseng M, Chakraborty H, Robinson D, Mendez M, Kohlmeyer L (1997) Adjustment for iron intake for dietary enhancers and inhibitors in population studies: bioavailable iron in rural and urban residing Russian women and children. J Nutr 127:1456–1468
Reddy M, Hurrell R, Cook J (2000) Estimation of nonheme-iron bioavailability from meal composition. Am J Clin Nutr 71:937–943
Hallberg L, Hulthén L (2000) Prediction of dietary iron absorption: an algorithm for calculating absorption and bioavailability of dietary iron. Am J Clin Nutr 71:1147–1160
Acknowledgments
CV, MO, and FP conceptualized and designed the study; MO and FP collected and analyzed the data; all authors interpreted the data; CV and AB wrote the manuscript. The authors gratefully acknowledge the technical assistance of María Angélica Letelier for her laboratory work and Juliana Haber and Sotiris Chaniotakis for their assistance in reviewing the English in this manuscript. All authors approved the final version of the manuscript. All authors declare no general, financial, or institutional competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valenzuela, C., Olivares, M., Brito, A. et al. Is a 40 % Absorption of Iron from a Ferrous Ascorbate Reference Dose Appropriate to Assess Iron Absorption Independent of Iron Status?. Biol Trace Elem Res 155, 322–326 (2013). https://doi.org/10.1007/s12011-013-9797-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-013-9797-2