Abstract
Background
A primary concern of younger, more active patients who have undergone total hip arthroplasty (THA) is the longevity of the implant. Cementless fixation and hard-on-hard bearings are recognized as options to enhance THA durability. Earlier, we published a series of 83 cementless primary THAs using 28-mm metal-on-metal (MoM) bearings in patients aged 50 years or younger; here we provide concise followup on that same group after an additional 8-year survey period.
Questions/purposes
(1) What is the long-term survivorship of cementless primary THA using 28-mm MoM bearings in patients aged 50 years or younger? (2) What are the clinical and radiographic results of cementless THA in this active patient population? (3) Can any of the observed implant failures or adverse events be attributed to the metallic nature of the bearing couple?
Methods
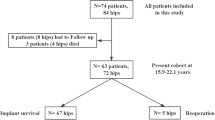
We retrospectively reviewed 83 cementless THAs performed in three institutions over a decade (1995–2004) in 68 patients with 28-mm MoM articulation. All patients (15 bilateral) had a median age of 42 years (range, 24–50 years) at the time of the index procedure and 56 of them (82% [70 hips]) had activity level graded Devane 4 or 5 before significant hip pain. A 28-mm Metasul™ articulation was used with an Alloclassic-SL™ cementless stem in all cases paired with three different cementless titanium acetabular components (one threaded and two press-fit cups) from the same manufacturer. Survivorship analysis was calculated according to Dobbs life table, patient clinical results were evaluated with use of the Postel-Merle d’Aubigné scoring system, radiographic analysis was performed by independent observers, and cobalt level was determined in whole blood.
Results
The 15-year survivorship (33 hips at risk) for revision for any reasons (four hips) and for aseptic loosening (one hip) was 96% (95% confidence interval [CI], 81%–99%) and 99% (95% CI, 85%–99.9%), respectively. The median Merle d’Aubigné-Postel score remained stable at 17 points (range, 10–18). Thus far, we have not observed pseudotumors or other adverse reactions to metallic debris. Eight hips have undergone reoperation: trochanteric suture removal (one), psoas tendon impingement (two), and five revisions for periprosthetic fracture (one), late infection (two), acetabular osteolysis (one, as a result of polyethylene backside wear), and one hydroxyapatite-coated cup for aseptic loosening. None of the complications, failures, or revisions observed so far could directly be related to the metallic nature of the 28-mm Metasul bearings used in this selected group of patients.
Conclusions
The current survey at 13-year median followup has not yet indicated any long-term deleterious effects related to dissemination of metallic ions. Two senior authors continue to use 28- or 32-mm Metasul™ bearings with cementless THA components in young and active patient populations. Longer followup with a more sophisticated imaging study is necessary to confirm this so far positive report.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because of the well-established success of primary THA, it has been used in younger patients for some time. The 2013 Swedish Hip Arthroplasty Register (SHAR) reported that 7% of men and 4% of women were younger than 50 years of age when getting their primary surgery, and this proportion of patients has stayed relatively constant over the last 20 years (1992–2013) [14]. Nevertheless, the longevity of their arthroplasty is a major concern for younger and active patients with longer life expectancies undergoing THA. The risk of aseptic loosening increases by 1.8% for each year of age reduction at the time of index surgery [38].
The most recent 2013 analysis from the SHAR notes that young age (ie, younger than 50 years) substantially reduces the survival of all types of primary THAs. In this analysis, the rates of revision for all diagnoses and all reasons were 57% and 59% for female and male patients, respectively [14]. Moreover, high activity level is recognized as the major factor affecting prosthetic reconstruction durability as a result of conventional polyethylene (PE) wear [43]. As a consequence, the use of hard-on-hard bearings has been proposed as an alternative to traditional low-friction arthroplasty.
In 2004, a large data-based matched case-control study indicated that metal-on-metal (MoM) bearings in conventional THA could demonstrate a lower risk of aseptic stem and/or cup loosening than metal-on-PE (MoP) bearings in the general population [40]. In addition, it is currently advised that patients with implanted MoM bearings should receive regular and standardized monitoring of metal ion concentrations [23]. Experience in France with Metasul™ (Zimmer-Biomet, Winterthur, Switzerland) 28-mm bearings started in 1994 [10]. Midterm results of this series were published in 2008 [11]. At that time, after a median followup of 7 years, we observed no radiographic evidence of component loosening and the 10-year survivorship with revision for any reason as the endpoint was 100% (95% confidence interval, 90%–100%). Here, we provide a concise followup on those same patients with an additional survey period of 8 years and the addition of cobalt blood level analysis performed in two institutions that was incomplete at the time of our 2008 publication. We focused particular attention on survivorship, clinical and radiographic results, and any complication that might be related to the metallic nature of the bearing couple.
Specifically, we asked: (1) What is the long-term survivorship of cementless primary THA using 28-mm Metasul bearings in patients aged 50 years or younger? (2) What are the patient-reported outcomes of cementless implants in this population? (3) Can any of the observed implant failures or adverse events be attributed to the metallic nature of the bearing couple?
Patients and Methods
This retrospective study was carried out in three orthopaedic settings, one private and two university teaching departments. Between January 1995 and December 2004, we performed 5730 primary THAs. On 419 occasions (7.3%), we used 28-mm Metasul bearings; of those Metasul THAs, 110 (26.3%) were performed in patients aged 50 years or younger, mostly with cementless implant fixation. During the inclusion study period, we used no other hard-on-hard bearings (either MoM or ceramic-on-ceramic). To reduce heterogeneity in the patient population, we excluded patients with at least one cemented implant, low activity level, rheumatoid arthritis, juvenile arthritic hips, and high dysplasia (greater than Crowe II). Finally, 27 (25%) of the 110 Metasul THAs performed in patients aged 50 years or younger were excluded for the following reasons: 15 hips according to the study criteria (dysplasia, five; inflammatory disease, 10); two patients died (three hips) in the first postoperative year; and nine patients (nine hips) had no adequate followup. That left 68 patients (83 hips; 75% of the 110 THAs performed in patients aged 50 years or younger) available at a median 13-year followup (range, 2–19 years). Seven male patients (eight hips, 10% of the index cohort) died of causes unrelated to their arthroplasty: two lung cancer (one at 18 months postsurgery), three postcirrhotic hepatic neoplasms, one suicide (two hips), and one ischemic heart attack. Eleven THAs (13%) have not been reviewed in the last 5 years (since 2010).
The 55 male and 13 female patients (sex ratio 4.2:1) had a median age of 42 years (range, 23–50 years) and were graded Charnley A, B, and C for 33, 30, and five patients, respectively, at the time of their primary THA. Using the classification of Devane et al. [16], 70 hips in 56 patients (82%) demonstrated preoperative activity level graded 4 and 5, and 13 hips were in 12 Grade 3 patients (18%). Preoperative diagnoses included aseptic necrosis in 35 hips (42%), secondary arthritis in 29 hips (dysplasia Crowe I and II, 23; posttrauma, four; Legg–Calvé–Perthes disease, two), and primary osteoarthritis in 19 hips. Previous surgery was noted in 15% of hips.
In all cases, a cementless Alloclassic-SL™ grit-blasted titanium femoral component (Zimmer-Biomet) was implanted with 28-mm Metasul bearings forged in high-carbide cobalt-chromium alloy Protasul-21 WF (ISO 5832-12, Metasul™; Zimmer-Biomet). All acetabular components were cementless titanium metal-backed cups from the same manufacturer (Zimmer-Biomet): 59 were hemispheric press-fit cups (40 of the Armor-Allofit® design with titanium mesh in Lille and 19 hydroxyapatite-coated in Strasbourg) and 24 were conical threaded rings (grit-blasted titanium Alloclassic-CSF® in Longjumeau; see previous report for more details) [11]. All surgeries were performed by four senior surgeons (CPD, AD, HM, FB) experienced in hip replacement (one in Longjumeau, two in Lille, and one in Strasbourg).
Clinical results were graded according to the Postel-Merle d’Aubigné (PMA) scoring system [36]. Component stability and osseointegration were assessed according to the method described by Engh et al. [19] (calcar atrophy, spot welds, stress shielding, and pedestal) on the femoral side and osteolysis was measured by the DeLee and Charnley method on the socket side [13]. Heterotopic ossification was graded according to the Brooker classification [4]. Conventional radiographic analysis was performed in each center by an independent observer not involved in the index surgeries (SP, BP, MB). More extensive imaging by ultrasound or CT scan was performed only in case of clinical concern. Cobalt levels were measured in whole blood but in only two centers (Lille and Longjumeau), initially by atomic absorption spectrometry (AAS) and more recently by the highly precise inductively coupled plasma/mass spectrometer (ICP/MS) technique. In case of reoperation-revision, we noted macroscopic aspect of the bearings, presence of metallosis, and degree of damage to surrounding soft tissue.
Statistical Analysis
Survivorship analysis was conducted according to the Dobbs life table with 95% confidence intervals calculated with the Wilson quadratic method [17].
Results
In this selected population, THA performed with Metasul bearings continued to demonstrate high survivorship. The 15-year survivorship rates with 33 hips at risk (40% of the index cohort) for the endpoints—hip reoperation for any cause (eight procedures), revision (defined as exchange of at least one prosthetic component) for any reasons (three hips during the 15-year period and one 17 years after primary THA for hematogenous infection; Table 1), and revision for aseptic loosening (one hip)—were 91% (95% confidence interval [CI], 72%–98%), 96% (95% CI, 81%–99%), and 99% (95% CI, 85%–99.9%), respectively. At the current 13-year median followup review, the revision percent observed component-years was 0.37.
Validated patient outcomes and radiographic results with cementless implants remained satisfactory when compared with our earlier results. The median PMA score, 17 in our 2007 review, remains stable at 17 points (range, 10–18) with a very good to excellent global score (16–18 points) for the 72 hips of the 59 nonrevised and living patients. Femoral osseointegration was confirmed by radiographic evidence of periprosthetic spot welds in 62% of hips and calcar lysis (round neck) in 23%. Heterotopic ossification was noted around 23 hips (32%) and classified as Brooker I in 17 hips (74%) and II and III in six hips (26%, three hips each). On the acetabular side, we noted 14 lucent lines (10 in Zone 1 and four in Zone 3) and five osteolytic lesions. Four were behind empty screw holes (one Armor-Allofit and three press-fit hydroxyapatite cups suggesting backside wear) and one more aggressive lesion was seen in Zone I at 11 years above a CSF-threaded cup implanted in 1997 in a 47-year-old woman.
At the time of our previous report, two hips had already undergone reoperation (one for trochanteric suture removal and another for psoas tendon release impingement) and no revision was necessary [11]. Since then, we performed two further reoperations for another psoas tendon release impingement; one Vancouver B1 periprosthetic fracture 5 years after index THA that healed uneventfully with cerclages; and four revisions (Table 1). Of those, two revisions were performed for hematogenic deep infection; the first infected hip (streptococcus G equisimilis septicemia) was fully revised at 6 years and the second for acute joint infection (methicillin-sensitive Staphylococcus aureus from a severe stomatologic osteitis) 17 years after the index THA was treated in two stages with conservation of the nonbearing components. The hip with asymptomatic osteolytic lesion above a CSF-threaded cup was also the result of PE backside wear (Fig. 1) and was treated by curettage, allograft, and retention of the stable stem and cup with new Metasul components and an excellent clinical result at 5.10 years. Finally, one hydroxyapatite-coated cup was revised for aseptic loosening 10 years after the initial THA performed for avascular head necrosis in a 48-year-old man. In all reoperation or revision procedures, no visual evidence of macroscopic metallosis was reported. We encountered two other complications: one sciatic nerve palsy with partial recovery and one late dislocation (at 8 years) treated by close reduction with no recurrence thus far.
(A) Prerevision AP radiograph shows an expansile osteolysis in Zone I above a Metasul threaded cup 11 years after primary THA in a 58-year-old active woman with no clinical symptoms; (B) prerevision tomodensitometric view; (C) aspect of the hip at revision surgery: note the macroscopic absence of any metallosis, tissue necrosis, nor creamy-like swelling; (D) aspect of the backside of the polyethylene inlay with obvious surface deterioration; (E) radiographic aspect 5.10 years after grafting and new 28-mm Metasul components.
For the 56 hips with available data, the last sample of whole blood cobalt level was ≤ 1 g/L for 28 hips (50%) and < 5 µg/L in all other hips except one (median, 1.5 µg/L; range, 0.4–8 µg/L). Median blood cobalt level was 1.4 µg/L for 38 patients with unilateral MoM THA and 1.76 µg/L for nine patients with bilateral MoM THA (+26%). The higher cobalt level (8 µg/L) was detected at 61 months postindex surgery performed in an alcoholic 45-year-old patient, who described clinical signs of subluxation but refused further followup and died in 2004 of postcirrhotic hepatic neoplasm.
Discussion
In its last electronic 2013 issue, the Swedish Hip Registry showed survivorship of approximately 75% at 15 years in patients younger than 50 years of age [14]. Reduced implant survivorship has long been noted in young patients. Because of longstanding concerns regarding the durability of MoP bearings, we began using hard-on-hard bearings in 1994 as an alternative to traditional low-friction arthroplasty. Our survival rate for THA revision of 96% at 15 years with cementless 28-mm MoM THA components indicates a substantial improvement in this selected group of young and active patients. We believe that our exclusion criteria, which select not only young but highly active patients, allows a clearer test of the effectiveness of cementless THAs with 28-mm Metasul bearings in improving THA longevity.
This study has obvious limitations. Acetabular implants are of three different types with three different surface treatments, although all are from the same manufacturer. This small group of patients was initially followed in three different centers. Since our first review, we created a centralized database that was completed and improved with time. This has corrected missing or wrong information and explains some variation in demographic data (median age, bilateral THAs) compared with those published in 2008 with no effect on the overall results and main observations. Currently, eight of the nine patients with insufficient followup to be included in the 2007 study group have been regularly reviewed since but were omitted from the 2015 study group to avoid possible skewing of results. Biologic surveys were not performed in one center and results came from two different laboratories with different techniques over the study period. Finally, although we observed no pseudotumor or other adverse reaction to metallic debris at reoperation-revision, we note that ultrasound, CT scan, or MRI investigations were not systematically performed; thus, asymptomatic soft tissue lesions might have escaped our survey [27].
We found generally high Merle d’Aubigné-Postel scores and reliable osseointegration with these cementless prosthesis designs. Femoral component fixation in patients younger than 50 years old is less debated today than at the onset of our experience. Modern cementing techniques and cementless femoral components showed good results with 10-year survival rates regularly greater than 95% [1, 5, 31, 33, 35, 46–48]. In this study, none of the 83 Alloclassic-SL stems have been revised for aseptic loosening after a median followup of 13 years in situ indicating that this cementless grit-blasted titanium straight taper design was well adapted to the standard femoral configuration selected according to the inclusion criteria. Atrophy and possibly light osteolytic lesion in the calcar area are frequently reported with this implant with no deleterious effect as confirmed by postmortem study of femoral osteolysis associated with well-functioning Alloclassic-SL MoM articulation [25]. In a meta-analysis comparing cemented and cementless THA fixation in patients younger than 50 years, only two studies fulfill the British NICE criteria (followup of > 10 years and survival of ≥ 90%) with a majority of inflammatory hip diseases and dysplasia [9]. Recently, the Nordic Arthroplasty Register Association (NARA) database indicated an overall 10-year survival of 83% for cementless stems with a relative risk of revision for aseptic loosening of 0.55 (0.44–0.69) compared with cemented THA [41]. The situation is quite different on the acetabular bearing side with disappointing results of conventional PE, either monobloc [20, 21, 30, 32, 42, 48, 50] or in modular metal-backed [7, 18, 37]. As a result, there has been substantial interest in use of hard-on-hard bearings (MoM or ceramic-on-ceramic [CoC]) or highly crosslinked PE [45], recently vitamin E-doped. Cemented low-friction arthroplasty cannot achieve sufficient long-lasting outcome in patients younger than 50 years old. Even in skilled hands, survival for all causes was 85.4% ± 5% at 20 years, 76% (cup only) at 22 years, and 81% at 30 years [21, 32, 42]. In a series of matched patients younger than 50 years of age comparing Metasul 28-mm with ceramic-on-PE, better survivorship was achieved with the MoM combination [37]. In the meantime, other experiences with high-carbide 28-mm MoM bearings paired with conventional cementless THAs in patients 50 years of age and younger were reported with thus far excellent results. In a Korean study, 28-mm Metasul on cementless CLS® stem-Wagner® cup (Zimmer-Biomet) showed 13-year survival of 99% and 98% for revision resulting from any reason and attributable to the development of osteolysis for any lesion, respectively [26]. In another series from Germany, 28-mm Metasul on cementless CLS stem-press fit titanium cup (Zimmer-Biomet) provided 13-year survival of 91% and 99% for revision as a result of any reason and resulting from aseptic implant loosening, respectively [28]; our results are in the same range. In an observational meta-analysis (29 studies) in patients younger than 55 years old (4085 patients) comparing bearing articulations, the 10-year survival rate was 95%, 92%, and 89% for THAs using MoM, MoP, and CoC, respectively, supporting the use of MoM articulations in young active patients [44]. In one prospective randomized study comparing 28-mm Metasul with CoC-Cerasul bearings at 9 years, neither bearing outperformed the other radiographically or clinically [15]. These data indicated that, provided osseointegration of the acetabular component is achieved, satisfactory long-term results can be obtained in younger and active patients with high-carbide 28-mm Metasul articular bearing surfaces through a variety of cementless shell profiles.
MoM bearings were mainly used in English-speaking communities for young and active patients through hip resurfacing (HR) and large head (LH) THA. Short-term results of HR in patients younger than 50 years were somehow disappointing with 94% survivorship at 5-year followup [2]. However, more importantly, various highly concerning events, mainly resulting from previously nearly unknown adverse reactions to metal debris, hypersensitivity, acute lymphocytic perivascular infiltration, pseudotumor, and potentially induced systemic adverse effects, in conjunction with high failure rates of some specific implants (ASR® hip resurfacing; DePuy, Warsaw, IN, USA), induced a very poor general and media leaders’ opinion about MoM bearings [6]. These concerns led to a dramatic reduction in HR and LH THA use by the worldwide orthopaedic community [22, 39]. MoM bearings are associated with the potential risk of systemic dissemination of metallic ions [12, 29]. This is of particular concern for young and active patients who are then exposed to higher levels of ions for a longer lifetime. Conversely, blood and serum cobalt and chromium ion levels are not markedly affected by patient activity [24]. Measured systemic metal levels must be used to monitor MoM hip arthroplasties [30], but the methodology is demanding and controversy remains with respect to analytic techniques, units, and acceptable range level [12]. In 2012, an European consensus recommended circulating metallic ion determination in whole blood by AAS or ICP/MS (both techniques used in our study) with a reference value within the range of 2 to 7 µg/L [22]. In our study, the latest available blood cobalt level was on all occasions below the 7-µg/L threshold value for clinical concern. Although Type IV hypersensitivity reactions have been described around failed MoM THAs [8, 49], carcinogenic concern has lost consistency considering epidemiologic data reported in the Nordic population [34]. An additional 8-year survey has not yet detected any deleterious effects associated with metallic ion chronic dissemination. When MoM bearings are being considered, whether in THA or with surface replacement arthroplasty, risks and benefits should be carefully balanced preoperatively, particularly in younger individuals. Besides renal insufficiency and patients with allergic disposition, women of childbearing age are not recommended candidates as a result of transplacental transfer of metallic ions [3, 51].
None of the complications, failures, or revisions observed in this series could directly be related to the metallic nature of the 28-mm Metasul bearings. These data indicated that our initial (2005) hypothesis about the good performance of cementless THA implant with 28-mm hard-on-hard metallic bearings remains valid 10 years later. Nevertheless, at this 2015 review, the median age of the 59 living and nonrevised patients is only 55 years with a large range, from 34 to 65 years, thus indicating for a majority of them a predictable life expectancy over 30 years. Indeed, improving THA longevity in active patients aged 50 years and younger still remains a challenge. Two senior authors (CD, HM) are still currently using 28- or 32-mm Metasul bearings in active (Devane 4 and 5) mostly male patients aged 65 years and younger. Obviously, continuous followup and longer term results with extensive imaging (ultrasound, metallic artifact reduction software MRI) are necessary to confirm our so far satisfying experience with cementless THA and 28-mm Metasul articulation.
References
Aldinger PR, Thomsen M, Mau H, Ewerbeck V, Breusch SJ. Cementless Spotorno tapered titanium stems: excellent 10-15-year survival in 141 young patients. Acta Orthop Scand. 2003;74:253–258.
Amstutz HC, Ball ST, Le Duff MJ, Dorey FJ. Resurfacing THA for patients younger than 50 years. Clin Orthop Relat Res. 2007;460:159–164.
Brodner W, Grohs JG, Bancher-Todesca D, Dorotka R, Meisinger V, Gottsauner-Wolf F, Kotz R. Does the placenta inhibit the passage of chromium and cobalt after metal-on-metal total hip arthroplasty? J Arthroplasty. 2004;19(Suppl 3):102–106.
Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632.
Capello WN, D’Antonio JA, Feinberg JR, Manley MT. Ten-year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old. A concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85:885–889.
Cohen D. How safe are metal-on-metal implants? BMJ. 2012;344:e1410.
Crowther JD, Lachiewicz PF. Survival and polyethylene wear of porous coated acetabular components in patients less than fifty years old: results at nine to fourteen years. J Bone Joint Surg Am. 2002;84:729–735.
Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005;87:18-27.
DeKam DCJ, Busch VJJF, Veth RPH, Schreurs BW. Total hip arthroplasties in young patients under 50 years: limited evidence for current trends. A descriptive literature review. Hip Int. 2011;21:518–585.
Delaunay C. Metal-on-metal bearings in cementless primary total hip arthroplasty. J Arthroplasty. 2004;19(Suppl 3):35–40.
Delaunay C, Bonnomet F, Clavert P, Laffargue P, Migaud H. THA using metal-on-metal articulation in active patients younger than 50 years. Clin Orthop Relat Res. 2008;466:340–346.
Delaunay C, Petit I, Learmonth ID, Oger P, Vendittoli PA. Metal-on metal bearings total hip arthroplasty: the cobalt and chromium ions release concern. Orthop Traumatol Surg Res. 2010;96:894–904.
DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32.
Department of Orthopaedics, Sahlgrenska University Hospital. The Swedish Hip Arthroplasty Register: Annual Report 2013. Available at: www.jru.orthop.gu.se. Accessed May 2015.
Desmarchelier R, Viste A, Chouteau J, Lerat J-L, Fessy M-H. Metasul versus Cerasul bearings. A prospective, randomized study at 9 years. J Arthroplasty. 2013;28:296.
Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis. Factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256–266.
Dorey F, Nasser S, Amstutz HC. The need for confidence intervals in the presentation of orthopaedic data. J Bone Joint Surg Am. 1993:1844–1852.
Duffy GP, Prpa B, Rowland CM, Berry DJ. Primary uncemented Harris-Galante acetabular components in patients 50 years old or younger: results at 10 to 12 years. Clin Orthop Relat Res. 2004;427:157–161.
Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128.
Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0-22 years. Acta Orthop. 2005;76:28–41.
Halley DK, Glassman AH. Twenty- to twenty-six-year radiographic review in patients 50 years of age or younger with cemented Charnley low-friction arthroplasty. J Arthroplasty. 2003;18(Suppl 1):79–85.
Hannemann F, Hartmann A, Schmitt J, Lützner J, Seidler A, Campbell P, Delaunay CP, Drexler H, Ettema HB, Garcia-Cimbrelo E, Huberti H, Knahr K, Kunze J, Langton DJ, Lauer W, Learmonth I, Lohmann CH, Morlock M, Wimmer MA, Zagra L, Günther KP. European multidisciplinary consensus statement on the use and monitoring of metal-on-metal bearings for total hip replacement and hip resurfacing. Orthop Traumatol Surg Res. 2013;99:263–271.
Hartmann A, Hennemann F, Lützner J, Seidler A, Drexler H, Günther K-P, Schmitt J. Metal ion concentrations in body fluids after implantation of hip replacements with metal-on-metal bearings—systematic review of clinical and epidemiological studies. PLoS One. 2013;8 e70359:1–25.
Heisel C, Silva M, Skipor AK, Jacobs JJ, Schmalzried TP. The relationship between activity and ions in patients with metal-on-metal bearing hip prostheses. J Bone Joint Surg Am. 2005;87:781–787.
Huber M, Reinisch G, Zenz P, Zweymüller K, Lintner F. Postmortem study of femoral osteolysis associated with metal-on-metal articulation in total hip replacement. An analysis of nine cases. J Bone Joint Surg Am. 2010;92:1720–1731.
Hwang KT, Kim YH, Kim YS, Choi IY. Cementless total hip arthroplasty with a metal-on-metal bearing in patients younger than 50 years. J Arthroplasty. 2011;26:1481–1487.
Hwang KT, Kim YH, Kim YS, Ryu JA. Prevalence of a soft-tissue lesion after small head metal-on-metal total hip replacement:13- to 19-year follow-up study. Bone Joint J. 2014;96:1594–1599.
Innmann MM, Gotterbarm T, Kretzer JP, Merle C, Ewerbeck V, Weiss S, Aldinger PR, Streit M. Minimum ten-year results of a 28-mm metal-on-metal bearing in cementless total hip arthroplasty in patients fifty years of age and younger. Int Orthop. 2014;38:920–934.
Jacobs JJ, Hallab NJ, Urban RM, Wimmer MA. Wear particles. J Bone Joint Surg Am. 2006;88(Suppl 2):99–102.
Jacobs JJ, Skipor AK, Campbell PA, Hallab NJ, Urban RM, Amstutz HC. Can metal levels be used to monitor metal-on-metal hip arthroplasties? J Arthroplasty. 2004;19(Suppl 3):59–65.
Keener JD, Callaghan JJ, Goetz DD, Pederson DR, Sullivan PM, Johnston RC. Twenty five-year results after Charnley total hip arthroplasty in patients less than fifty years old: a concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85:1066–1072.
Kerboull L, Hamadouche M, Courpied JP, Kerboull M. Long-term results of Charnley-Kerboull hip arthroplasty in patients younger than 50 years. Clin Orthop Relat Res. 2004;418:112–118.
Lewthwaite SC, Squires B, Gie GA, Timperley AJ, Ling RS. The Exeter Universal hip in patients 50 years or younger at 10-17 years’ followup. Clin Orthop Relat Res. 2008;466:324–331.
Mäkela KT, Visuri T, Pulkkinen P, Eskelinen A, Remes V, Virolainen P, Junnila M, Pukkala E. Cancer incidence and cause-specific mortality in patients with metal-on-metal hip replacements in Finland. A population-based study with a mean follow-up of 4.6 (1-11) years. Acta Orthop. 2014;85:32–38.
McAuley JP, Szuszczewicz ES, Young A, Engh CA Sr. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125.
Merle D’Aubigné R. [Numerical classification of the function of the hip. 1970] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:371–374.
Migaud H, Putman S, Krantz N, Vasseur L, Girard J. Cementless metal-on-metal versus ceramic-on-polyethylene hip arthroplasty in patients less than fifty years of age: a comparative study with twelve to fourteen-year follow-up. J Bone Joint Surg Am. 2011;93(Suppl 2):137–142.
Muller U, Gautier E, Roeder C, Busato A. The relationship between cup design and the radiological signs of aseptic loosening in total hip arthroplasty. J Bone Joint Surg Br. 2003;85:31–36.
National Joint Registry Web site for England and Wales. National Joint Registry Annual Report. Available at: www.njrcentre.org.uk. Accessed May 18, 2015.
Naudie D, Roeder CP, Parvizi J, Berry DJ, Eggli S, Busato A. Metal-on-metal versus metal-on-polyethylene bearings in total hip arthroplasty: a matched case-control study. J Arthroplasty. 2004;19(Suppl 2):35–41.
Pedersen AB, Mehnert F, Havelin LI, Furnes O, Herberts P, Kärrholm J, Garellick G, Mäkela K, Eskelinen A, Overgaard S. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age. Results from the Nordic Arthroplasty Register Association. Osteoarthritis Cartilage. 2014;22:659–667.
Porter M. Long term outcome of the Charnley hip replacement in the young. Hip Int. 2003;13(Suppl 2):S28–S30.
Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Favae F, McKellop HA, McClung CD, Martell J, Moreland JR, Amstutz HC. Wear is a function of use, not time. Clin Orthop Relat Res. 2000;381:36–46.
Shetty V, Shitole B, Shetty G, Thakur H, Bhandari M. Optimal bearing surfaces for total hip replacement in the young patient: a meta-analysis. Int Orthop. 2011;35:1281–1287.
Shia DS, Clohisy JC, Schinsky MF, Martell JM, Maloney WJ. THA with highly cross-linked polyethylene in patients 50 years or younger. Clin Orthop Relat Res. 2009;467:2059–2065.
Singh S, Trikha SP, Edge AJ. Hydroxyapatite ceramic-coated femoral stems in young patients. A prospective ten-year study. J Bone Joint Surg Br. 2004;86:1118–1123.
Smith SE, Estok DM, Harris WH. 20-year experience with cemented primary and conversion total hip arthroplasty using so-called second-generation cementing techniques in patients aged 50 years or younger. J Arthroplasty. 2000;15:263–273.
Vervest TMJS, Anderson PG. The Zweymüller cementless total hip prosthesis in patients aged 50 years and younger. Hip Int. 2005;15:1–11.
Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28–36.
Wroblewski BM, Siney PD, Fleming PA. Charnley low-frictional torque arthroplasty in patients under the age of 51 years. Follow-up to 33 years. J Bone Joint Surg Br. 2002;84:540–543.
Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJW. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty. A controlled study. J Bone Joint Surg Br. 2007;89:301–305.
Acknowledgments
Professor Antoine Duquesnoy performed some of the Metasul THAs of the Lille series.
Funding
Research funding provided by Zimmer-Biomet, Warsaw, ID.
Author information
Authors and Affiliations
Corresponding author
Additional information
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Clinique de l’Yvette, Longjumeau, France.
About this article
Cite this article
Delaunay, C.P., Putman, S., Puliéro, B. et al. Cementless Total Hip Arthroplasty With Metasul Bearings Provides Good Results in Active Young Patients: A Concise Followup. Clin Orthop Relat Res 474, 2126–2133 (2016). https://doi.org/10.1007/s11999-016-4920-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-4920-2