Abstract
Background
The Bernese periacetabular osteotomy (PAO) continues to be a commonly performed nonarthroplasty option to treat symptomatic developmental hip dysplasia, but there are few long-term followup studies evaluating results after PAO.
Questions/purposes
(1) What is the long-term survivorship of the hip after PAO? (2) What were the validated outcomes scores among patients who had PAO more than 14 years ago? (3) What factors are associated with long-term failure?
Methods
One hundred fifty-eight dysplastic hips (133 patients) underwent PAO between May 1991 and September 1998 by a single surgeon. Of those, 37 hips (34 patients [26%]) were lost to followup; an additional seven patients (5% [eight hips]) had not been seen in the last 5 years. The 121 hips (in 99 patients) were retrospectively evaluated at a mean of 18 years (range, 14–22 years). Survivorship was assessed using Kaplan-Meier analysis with total hip arthroplasty (THA) as the endpoint. Hips were evaluated for activity, pain, and general health using the UCLA Activity Score, modified Harris hip score, WOMAC, and Hip disability and Osteoarthritis Outcome Score (HOOS). Failure was defined as a WOMAC pain subscale score ≥ 10 or having undergone THA. Hips were divided into three groups: asymptomatic (did not meet any failure criteria at any point in time), symptomatic (met WOMAC pain failure criteria at previous or most recent followup), and replaced (having undergone THA). A multinomial logistic regression model using a general estimating equations approach was used to assess factors associated with failure.
Results
Kaplan-Meier analysis with THA as the endpoint revealed a survival rate (95% confidence interval [CI]) of 74% (66%–83%) at 18 years. Twenty-six hips (21%) underwent THA at an average of 9 ± 5 years from the surgery. Sixty-four hips (53%) remained asymptomatic and did not meet any failure criteria at most recent followup. Thirty-one hips (26%) were symptomatic and considered failed based on a WOMAC pain score of ≥ 10 with a mean ± SD of 11 ± 4 out of 20 at most recent followup. Although some failed initially by pain, their most recent WOMAC score may have been < 10. Of the 16 symptomatic hips that failed early by pain (reported a WOMAC pain subscale score ≥ 10 in the prior study), two were lost to followup, two underwent THA at 16 and 17 years, four still failed because of pain at most recent followup, and the remaining eight had WOMAC pain scores < 10 at most recent followup. Asymptomatic hips reported better UCLA Activity Scores (asymptomatic: mean ± SD, 7 ± 2; symptomatic: 6 ± 2, p = 0.001), modified Harris hip scores (pain, function, and activity sections; asymptomatic: 80 ± 11; symptomatic: 50 ± 15, p < 0.001), WOMAC (asymptomatic: 2 ± 2, symptomatic: 11 ± 4, p < 0.001), and HOOS (asymptomatic: 87 ± 11, symptomatic: 52 ± 20, p < 0.001) compared with symptomatic hips at long-term followup. Age older than 25 years at the time of PAO (symptomatic: odds ratio [OR], 3.6; 95% CI, 1.3–9.8; p = 0.01; replaced: OR, 8.9; 95% CI, 2.6–30.9; p < 0.001) and a preoperative joint space width ≤ 2 mm (replaced: OR, 0.3; 95% CI, 0.12–0.71; p = 0.007) or ≥ 5 mm (replaced: OR, 0.121; 95% CI, 0.03–0.56; p = 0.007) were associated with long-term failure while controlling for poor or fair preoperative joint congruency.
Conclusions
This study demonstrates the durability of the Bernese PAO at long-term followup. In a subset of patients, there was progression to failure over time. Factors of progression to THA or more severe symptoms include age older than 25 years, poor or fair preoperative hip congruency, and a preoperative joint space width that is less than 2 mm or more than 5 mm. Future studies should focus on evaluating the two failure groups that we have identified in our study: those that failed early and went on to THA and those that are symptomatic at long-term followup.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Developmental dysplasia of the hip (DDH) is a major cause of osteoarthritis in the young adult hip that can lead to THA at a young age [3, 15, 20, 35, 36, 45, 46]. The abnormal anatomy results in changes to the biomechanics of the hip that lead to axial overloading with decreased contact area, increased contact pressure, and maximum loading at the rim [22, 24, 30]. Joint preservation surgery continues to be a desirable option in the young adult because THA may be associated with early revision [10–12, 16, 18, 34].
There are few studies evaluating patients at long-term followup after Bernese periacetabular osteotomy (PAO) [2, 40]. Predicting which hips will remain asymptomatic continues to be a challenge and it is necessary to evaluate the long-term results to properly select patients who will have durable results. We previously reported on the 9-year average duration followup in a cohort of 135 hips in 109 patients who underwent PAO by a single surgeon (MM) [31]. The average age of patients at the time of surgery was 26 years (range, 10–45 years), and the cohort included 119 females (88%) and 16 males (12%). In the previous report, 17 hips were converted to arthroplasty and 16 had WOMAC pain scores ≥ 10. With conversion to THA or WOMAC pain score ≥ 10 as the endpoint, 76% of hips survived at an average of 9 years. As the PAO is becoming more widely used [5, 8, 26, 28, 30], knowledge of long-term outcomes is necessary to educate providers and stratify patients who will benefit from surgery. Predictors of failure and poor outcomes have been linked to advanced age, advanced preoperative arthrosis, flawed preoperative joint congruency, larger preoperative alpha angles, and postoperative impingement [2, 31, 40, 43]. Therefore, it was our purpose to evaluate these factors and to determine if other factors were associated with more severe symptoms and long-term failure.
We therefore asked: (1) What is the long-term survivorship of the hip after PAO? (2) What were the validated outcomes scores among patients who had PAO more than 14 years ago? (3) What factors are associated with long-term failure?
Patients and Methods
This is a retrospective study of 135 patients with DDH. Institutional review board approval was obtained for this study. Patients were located through review of our hospital database, REDCap, and further evaluated with chart review. REDCap is a prospectively maintained institutional database in the orthopaedic surgery department; it includes all patients who are treated with PAO. Inclusion criteria were all patients of the single surgeon (MM) who underwent PAO for DDH from May 1991 and September 1998. Exclusion criteria were prior hip trauma and neuromuscular or connective tissue disorder.
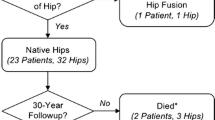
Patients with hip pain who presented to the senior author (MM) with radiographic evidence of femoral head uncovering and a lateral center-edge angle < 20° as well as closed triradiate cartilage were considered for PAO. Contraindication to PAO was osteoarthritis without remaining cartilage to correct into the weightbearing zone or prior hip trauma. A total of 189 PAOs were performed in 157 patients during the study period and 31 hips underwent PAO for reasons other than DDH. One hundred fifty-eight dysplastic hips were available for review, and of those, 37 hips were in patients who could not be reached or who had died (one patient). A total of 121 hips in 99 patients (74% followup) with DDH were reviewed and this is the group on which all of the analysis was based (Fig. 1). An additional seven patients (5% [eight hips]) had not been seen in the last 5 years. The average age at PAO was 27 years (range, 10–45 years). This group consisted of 86 female patients (106 hips) and 13 male patients (15 hips).
The PAO was considered a failure if the patient had undergone a THA on their surgically corrected hip or if the WOMAC pain subscale score was ≥ 10, a level previously described as correlating with significant pain [15]. Hips were stratified into three groups: asymptomatic (did not meet any failure criteria at any point in time), symptomatic (met WOMAC pain failure criteria at previous or most recent followup), and replaced (having undergone THA).
The surgical technique that has been previously reported [31, 32] was performed according to Ganz et al. [14] and, after 1993, modified to an abductor-sparing approach as described by Murphy and Millis [37]. Before September 1994, arthrotomy was not performed. A single surgeon (MM) performed all PAOs.
Activity, pain, and health-related quality-of-life outcomes were collected with the use of a mailed hip questionnaire that included the UCLA Activity Score, modified Harris hip score (pain, function, and activity sections), WOMAC pain score, and Hip disability and Osteoarthritis Outcome Score (HOOS) (Table 1). All of these are validated outcome scores for assessing patients with hip osteoarthritis [4, 6, 38, 41]. The WOMAC pain subscale score addressed pain attributable to the operative hip over the prior 4 weeks and comprised five activity areas: (1) walking on a flat surface; (2) climbing up or down stairs; (3) lying in bed at night; (4) sitting or lying; and (5) standing upright. Pain was scored as 0 (none), 1 (mild), 2 (moderate), 3 (severe), or 4 (extreme). In patients who had bilateral PAOs, they completed the series of questions for each hip individually. Clinical evaluations of patients who were unable to be examined by physicians at our institution were performed by telephone interview (13 patients) or by a mailed hip questionnaire (45 patients). A senior orthopaedic surgery resident (JW) made all phone calls independently of the treating surgeon using an institutional review board-approved standardized phone script.
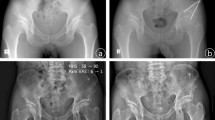
Preoperative, early postoperative, and late postoperative radiographs were evaluated for the lateral center-edge angle of Wiberg (LCEA), the acetabular roof angle as described by Tönnis, the minimum joint space measured in millimeters, joint congruency as described by Yasunaga, and osteoarthritis grade as described by Tönnis and measured on AP pelvis radiographs. The anterior center-edge angle of Lequesne and de Seze (ACEA) was measured on the false profile radiograph [29, 31, 42, 47, 48]. All patients with radiographs available were reviewed and none was excluded. The Tönnis classification of osteoarthritis was graded as 0 (no changes), 1 (widened sclerotic zone and minimal osteophyte formation), 2 (moderate loss of joint space and cyst formation), and 3 (< 1 mm of joint space or no joint space). Joint congruency was graded according to Yasunaga as excellent (if the radii of curvature of the acetabulum and the femoral head were identical and joint space was maintained), good (curvature of femoral head and acetabulum not identical but with preserved joint space), fair (joint space partially narrowed), and poor (loss of joint space) [48]. There were 53 hips available for late postoperative radiographic review at a mean ± SD time of 17 ± 2 years from PAO. A senior orthopaedic surgery resident (JW) made all radiographic measurements. Intraobserver reliability was assessed using the intraclass correlation coefficient (ICC) with a (2, 1) modeling scheme for continuous measurements and Fleiss’ kappa for ordinal measurements. All measurements were performed over a 2-week interval and demonstrated excellent reliability for joint space width (ICC = 0.95; 95% confidence interval [CI], 0.91–0.97), ACEA (ICC = 0.76; 95% CI, 0.58–0.85), and LCEA (ICC = 0.75; 95% CI, 0.598–0.85); good reliability for Tönnis grade (kappa = 0.71; 95% CI, 0.53–0.89); and fair reliability for Tönnis angle (ICC = 0.41; 95% CI, 0.16–0.62).
Twenty-seven hips underwent one or more osteotomies before the PAO and there were 25 hips that had simultaneous intertrochanteric osteotomy. For those hips that had osteotomies before the PAO, 13 underwent an innominate Salter osteotomy, nine underwent an intertrochanteric osteotomy, three had Pemberton osteotomies, one a Chiari osteotomy, and one a shelf osteotomy. For those hips that underwent simultaneous intertrochanteric osteotomy at the time of PAO, 23 had varus derotational osteotomies and two had valgus-producing osteotomies. There were no clinical or radiographic predictors of the need for an additional intertrochanteric osteotomy.
Of the 16 symptomatic hips that failed early by pain (reported a WOMAC pain subscale score ≥ 10 in the prior study [31]), two were lost to followup, two underwent THA at 16 and 17 years, four still failed by pain at most recent followup, and the remaining eight had WOMAC pain scores < 10 at most recent followup. The two hips that subsequently went on to THA continued to be part of the symptomatic group for purposes of the statistical analysis as well as the eight patients who reported a WOMAC of < 10 at most recent followup, because they initially failed because of pain.
Statistical Analysis
Continuous characteristics that followed approximately normal distributions (including age, ACEA, and Tönnis angle) were summarized by mean and SD and compared using Student’s t-test. Continuous characteristics that departed from normality (including minimum joint space and LCEA) were compared using the Mann-Whitney U test. Binary and categorical characteristics (age group [≤ 25 years and > 25 years], sex, laterality, dichotomized radiographic measurements, joint congruency, labral tear, and crossover sign) were compared using a chi square test or Fisher’s exact test, as appropriate. Tönnis grade and trichotomized radiographic measurements were compared across outcome groups using the Cochran-Armitage test for trend. Receiver operating characteristic (ROC) curve analysis was performed for age and for each continuous radiographic measurement outcome. Cutoffs that simultaneously maximized sensitivity and specificity were identified for measurement with respect to each failure outcome by Youden’s index. A multinomial logistic regression model using a general estimating equations (GEE) approach to model correlated responses for bilateral hips was applied to all demographic and radiographic characteristics to determine factors associated with asymptomatic, symptomatic, or replaced hips. ROC analysis indicated that dichotomizing age at PAO at 25 years gave optimal predictive power. In addition, a trichotomy of preoperative joint space width (≤ 2 mm, 2–5 mm, and ≥ 5 mm) and a dichotomy of preoperative joint congruency (poor/fair versus good/excellent) further strengthened the model. Model selection was conducted using a backward selection methodology based on Akaike’s Information Criteria [23]. An algorithm based on significant factors was created to predict the probability of an asymptomatic, symptomatic, or replaced hip [1].
Survivorship analysis for THA was performed using the Kaplan-Meier product-limit method to account for censoring. The 95% confidence limits about the survivor curve were estimated using the Greenwood formula [19]. In addition, hip characteristics, including age, sex, and body mass index as well as preoperative and postoperative radiographic measurements, including minimum joint space width, joint congruency, presence of labral tear, crossover sign, LCEA, ACEA, Tönnis angle, and Tönnis grade, were compared between hips that were lost to followup and those that were available for analysis. No differences were detected between groups, and thus all analyses were conducted under the assumption that the data were missing at random. All tests were two-sided and p values < 0.05 were considered significant.
Results
Kaplan-Meier analysis with THA as the endpoint revealed a survival rate (95% CI) of 85% (79%–92%) at 10 years, 80% (73%–88%) at 15 years, and 74% (66%–83%) at 18 years (Fig. 2). Sixty-four hips (53%) remained asymptomatic and did not meet any failure criteria at most recent followup (mean, 18 years; range, 14–22 years). Fifty-seven hips developed some level of treatment failure and were classified as replaced or symptomatic. Twenty-six hips (21%) went on to THA at an average of 9 ± 5 years from the surgery and 31 (26%) were symptomatic. Only five hips (12%) that were later converted to THA were in patients younger than 25 years of age at the time of the PAO. The mean age for asymptomatic hips was younger than that of symptomatic or replaced hips (Table 2).
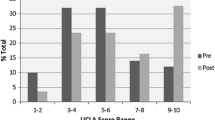
At an average of 18 ± 2 years, asymptomatic hips reported better UCLA Activity Scores (asymptomatic: mean ± SD, 7 ± 2; symptomatic: 6 ± 2, p = 0.001), modified Harris hip scores (asymptomatic: 80 ± 11; symptomatic: 50 ± 15, p < 0.001), WOMAC (asymptomatic: 2 ± 2, symptomatic: 11 ± 4, p < 0.001), and HOOS (asymptomatic: 87 ± 11, symptomatic: 52 ± 20, p < 0.001) compared with symptomatic hips at long-term followup (Table 3).
Based on the adjusted multinomial model controlling for preoperative joint congruency, hips that were older than 25 years at PAO had nearly nine times the odds, compared with hips younger than 25 years, of being replaced versus asymptomatic at followup (odds ratio [OR], 8.9; 95% CI, 2.6–30.9; p < 0.001; Table 4). However, hips that were older than 25 years at PAO had more than three times the odds of being symptomatic versus asymptomatic at followup (OR, 3.6; 95% CI, 1.3–9.8; p = 0.01). In addition, hips with a minimum joint space width ≥ 5 mm had an 88% decrease in odds compared with hips with a joint space width ≤ 2 mm of being replaced versus asymptomatic at followup (OR, 0.12; 95% CI, 0.03–0.56; p = 0.007). The degree of preoperative LCEA (symptomatic: p = 0.15, replaced: p = 0.09), ACEA (0.19, 0.50), and Tönnis angle (p = 0.73, 0.15) or postoperative LCEA (p = 0.82, 0.51), ACEA (p = 0.43, 0.48), and Tönnis angle (p = 0.82, 0.85) was not statistically different between the groups nor was it found to be prognostic. A probability algorithm based on the multinomial model indicated that a hip that is at most 25 years old at PAO has good or excellent joint congruency and has a minimum joint space width between 2 and 5 mm, has an 81% probability of being asymptomatic, 15% probability of being symptomatic, and 5% probability of being replaced at an average of 18 years of followup (Table 5).
Discussion
Few long-term outcomes after PAO have been reported and to our knowledge ours is among the largest; in it, we aimed to define and analyze factors associated with long-term failure [2, 7, 17, 21, 28, 31, 33, 40, 43]. Our data suggest that the ideal candidate is younger than 25 years of age with adequate joint space width and good hip congruency.
This study has limitations. First, this retrospective study represents a single surgeon’s experience in a high-volume center. This author (MM) is a master technician and as a single-surgeon series, this is a strength and weakness. The results may not be representative of low-volume surgeons or centers, which may limit the ability to generalize the results. In similar high-volume joint preservation centers, this study may help to guide surgeons. Second, intraoperative head and neck offset was not evaluated nor corrected, and postoperative radiographs were not analyzed for head and neck offset during the initial study surgical time period. Albers et al. [2], in their 10-year retrospective study, found that impingement adversely affected outcome. Unfortunately, we are unable to comment on the possibility of iatrogenic femoroacetabular impingement being a risk factor for failure.
We also note that this is a retrospective case series without a control group. This type of study can suffer from a variety of biases. Selection bias was mitigated by our inclusion criteria, which was well defined and because of such criteria, these results only apply to patients with symptomatic DDH without prior hip trauma or neuromuscular or connective tissue disease. Thirty-seven hips (34 patients [26%]) were lost to followup and although their preoperative characteristics were similar, postoperative survivorship and patient-reported outcomes were not available for these patients. Patients lost to followup allow for transfer bias and therefore these results represent a best case scenario because we are not able to report on the outcomes of those not accounted for. Also, there were eight hips in seven patients who had not been seen at our institution within the past 5 years. We kept these patients and included them in the analysis because our goal was to review a 15-year snapshot post-PAO. We must recognize that there were no comparative preoperative outcome measures available and this is also a limitation to this study. Another limitation is that long-term postoperative radiographs were available for only 35 (55%) of the 64 asymptomatic hips and 19 (61%) of the 31 symptomatic hips. Although radiographic data were not part of the failure criteria, long-term postoperative radiographs would have been useful for evaluation. Although bilateral hips were included in the analyses, we were able to adjust for any potential bias introduced by correlated measurements on the same subjects. In addition, when comparing the GEE-adjusted analysis with a standard general linear modeling analysis, the GEE model provided more accurate effect estimates with narrower CIs. Thus, we can assume that little bias was introduced by including bilateral hips and the hips in our study present unique cases of long-term PAO followup.
Historically, only conversion to a THA has been considered a failure [2, 8, 21, 40]. In a young adult population, this is not a good marker of PAO failure. We have shown that, despite not undergoing THA, some patients report pain and a diminished quality of life. Therefore, patient-reported outcomes are required to properly assess patient pain and function. The main outcome score and determinant of failure used in this and our initial report was the WOMAC pain subscale score (Fig. 3). A WOMAC pain subscale greater than or equal to 10 has been shown to be a clinically accurate criterion in evaluating hip osteoarthritis as well as those patients undergoing nonarthroplasty hip surgery [9, 13, 25, 27, 39]. Patient-acceptable symptom state and minimal clinically important improvement are important factors when choosing a subjective outcome measure. This WOMAC pain cutoff is useful in this regard and can correctly identify subjects who are satisfied and unsatisfied [13]. We have shown that symptomatic hips (those that failed as a result of WOMAC pain score ≥ 10) reported significantly (p < 0.001) worse pain, activity, and quality-of-life outcomes than asymptomatic hips in all outcome measures used.
DDH is a known cause of pain and is a substantial cause of morbidity in the young adult population [2, 5, 17]. Few studies have reported on activity-related and quality-of-life outcomes after PAO. Beaulé et al. [5] in their 2014 series on dysplastic hips reported a preoperative UCLA score of 5.3 with an improvement to 6.6 at a median of 5 years postoperative followup. van Bergayk and Garbuz [44] reported on quality of life and sports-specific outcome measures on a small cohort of 22 patients with followup of 2 years. They found a clinically important improvement in WOMAC and SF-36 scores at short-term followup. In our study, the mean long-term postoperative UCLA Activity Score was 7 ± 2 for the asymptomatic hips and 6 ± 2 for symptomatic hips. These results are comparable to Beaulé et al.’s [5] and van Bergayk and Garbuz’ [44]. We are able to show at long-term followup that patients undergoing PAO whether asymptomatic or symptomatic are able to remain regularly active.
Steppacher et al. [40] reported on the mean 20-year followup of 58 hips. Forty-one hips (60%) remained preserved and did not undergo THA, and eight hips (20%) that remained preserved were graded as fair or poor according to their mean Merle d’Aubigne scores. Several variables were identified as prognostic. These included age older than 30 years, lower preoperative Merle d’Aubigne and Postel score, positive preoperative anterior impingement test, preoperative limp, greater preoperative arthrosis according to Tönnis grade, and postoperative extrusion index [40]. Our study found that age older than 25 years is an independent predictor of failure whether by results of WOMAC pain subscale score ≥ 10 or conversion to THA. In addition to age, preoperative joint space and preoperative joint congruency further strengthened a prediction model. We were unable to find any postoperative characteristics that were independent predictors of failure. We constructed a simplified table for easy reference to display the long-term prognosis after PAO (Table 5). A patient who is at most 25 years old at PAO has good or excellent joint congruency and has a minimum joint space width between 2 and 5 mm has an 81% probability of being asymptomatic, 15% probability of being symptomatic, and 5% probability of being replaced at an average of 18 years of followup. Our analysis can help guide surgeons to choose patients who might benefit from PAO and thus help improve outcomes.
In summary, we found that the majority of hips (77%) at an average of 18 years are preserved and had not undergone THA. A subset of patients was identified as having worse outcome measures at long-term followup and were classified as symptomatic (26%). Three factors of having a symptomatic or replaced outcome were identified: preoperative age older than 25 years, preoperative minimum joint space width less than 2 mm or greater than 5 mm, and a poor or fair preoperative hip congruency. Based on these findings, we believe that proper selection of patients is crucial in optimizing outcomes for patients who may benefit from PAO as well as identifying patients who would be better treated with THA. It is important to understand that although we found age older than 25 years to be associated with failure, it should not be used as an age cutoff for surgery, because older patients may benefit from PAO by virtue of other favorable preoperative variables. Future studies should be focused on patients who undergo early replacement or have symptomatic hips despite the identified favorable factors. These patients may have additional poor prognostic features that are not yet apparent.
References
Agresti A. Categorical Data Analysis. New York, NY, USA: Wiley; 1990:165–300.
Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614.
Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986;35:119–128.
Ashby E, Grocott MPW, Haddad FS. Outcome measures for orthopaedic interventions on the hip. J Bone Joint Surg Br. 2008;90:545–549.
Beaulé PE, Dowding C, Parker G, Ryu J-J. What factors predict improvements in outcomes scores and reoperations after the Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2015;473:615–622.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840.
Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–259.
Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052.
Davidson D, Yen Y-M, Jette AM, Olarsch S, Kim Y-J. Responsiveness of the SF-36 and WOMAC following periacetabular osteotomy for acetabular dysplasia. J Bone Joint Surg Am. 2011;93:2214–2218.
Devitt A, O’Sullivan T, Quinlan W. 16- to 25-year follow-up study of cemented arthroplasty of the hip in patients aged 50 years or younger. J Arthroplasty. 1997;12:479–489.
Dorr LD, Kane TJ, Conaty JP. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger. A 16-year follow-up study. J Arthroplasty. 1994;9:453–456.
Duffy GP, Berry DJ, Rowland C, Cabanela ME. Primary uncemented total hip arthroplasty in patients < 40 years old. J Arthroplasty. 2001;16:140–144.
Emerson Kavchak AJ, Cook C, Hegedus EJ, Wright AA. Identification of cut-points in commonly used hip osteoarthritis-related outcome measures that define the patient acceptable symptom state (PASS). Rheumatol Int. 2013;33:2773–2782
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36.
Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 2008;466:264–272.
Garellick G, Kärrholm J, Rogmark C. Swedish Hip Arthroplasty Register: Annual Report 2012. Gothenburg, Sweden: Goran Garellick; 2012.
Garras DN, Crowder TT, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007;89:721–724.
Georgiades G. Charnley low-friction arthroplasty in young patients with osteoarthritis outcomes at a minimum of twenty-two years. J Bone Joint Surg Am. 2009;91:2846–2851.
Harris EK, Albert A. Survivorship Analysis for Clinical Studies. New York, NY, USA: Dekker; 1991:29–49.
Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33.
Hartig-Andreasen C, Troelsen A, Thillemann TM, Søballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res. 2012;470:2978–2987.
Hipp JA, Millis MB, Murphy SB. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res. 1999;364:134–143
Hosmer DW, Lemeshow W. Applied Logisted Regression. 2nd ed. New York, NY, USA: Wiley; 2000:91–142.
Jessel RH. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120–1129.
Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013;41:2065–2073.
Kim Y-J. Nonarthroplasty hip surgery for early osteoarthritis. Rheum Dis Clin North Am. 2008;34:803–814.
Konan S, Tahmassebi J, Haddad FS. The development and validation of a more discriminating functional hip score for research. HSS J. 2012;8:198–205.
Kralj M, Mavčič B, Antolič V, Iglič A, Kralj-Iglič V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840.
Lequesne M, de Seze S. [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies] [in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652.
Leunig M, Ganz R. The evolution and concepts of joint-preserving surgery of the hip. J Bone Joint Surg Br. 2014;96:5–18.
Matheney T. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123.
Matheney T, Kim Y-J, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2010;92(Suppl 1):115–129.
Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;363:21–32.
McAuley JP, Szuszczewicz ES, Young A, Engh CA Sr. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125.
Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989.
Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–223.
Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98.
Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and Osteoarthritis Outcome Score (HOOS)–validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10.
Paulsen A, Pedersen AB, Overgaard S, Roos EM. Feasibility of 4 patient-reported outcome measures in a registry setting. Acta Orthop. 2012;83:321–327.
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644.
Terwee CB, Bouwmeester W, van Elsland SL, de Vet HCW, Dekker J. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis Cartilage. 2011;19:620–633.
Tönnis DD, Heinecke AA. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770.
Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179.
van Bergayk AB, Garbuz DS. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br. 2002;84:339–343.
Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61:334–338.
Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–76.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand Suppl. 1939;83(Suppl 1):S2–7.
Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006;88:1915–1919.
Acknowledgments
We thank Michelle Heinz and Laura Mercado Torres.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Wells, J., Millis, M., Kim, YJ. et al. Survivorship of the Bernese Periacetabular Osteotomy: What Factors are Associated with Long-term Failure?. Clin Orthop Relat Res 475, 396–405 (2017). https://doi.org/10.1007/s11999-016-4887-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-4887-z