Abstract
Background
Considering the cost and risk associated with revision Total knee arthroplasty (TKAs) and Total hip arthroplasty (THAs), steps to prevent these operations will help patients and reduce healthcare costs. Revision risk calculators for patients may reduce revision surgery by supporting clinical decision-making at the point of care.
Questions/purposes
We sought to develop a TKA and THA revision risk calculator using data from a large health-maintenance organization’s arthroplasty registry and determine the best set of predictors for the revision risk calculator.
Methods
Revision risk calculators for THAs and TKAs were developed using a patient cohort from a total joint replacement registry and data from a large US integrated healthcare system. The cohort included all patients who had primary procedures performed in our healthcare system between April 2001 and July 2008 and were followed until January 2014 (TKAs, n = 41,750; THAs, n = 22,721), During the study period, 9% of patients (TKA = 3066/34,686; THA=1898/20,285) were lost to followup and 7% died (TKA= 2350/41,750; THA=1419/20,285). The outcome of interest was revision surgery and was defined as replacement of any component for any reason within 5 years postoperatively. Candidate predictors for the revision risk calculator were limited to preoperative patient demographics, comorbidities, and procedure diagnoses. Logistic regression models were used to identify predictors and the Hosmer-Lemeshow goodness-of-fit test and c-statistic were used to choose final models for the revision risk calculator.
Results
The best predictors for the TKA revision risk calculator were age (odds ratio [OR], 0.96; 95% CI, 0.95–0.97; p < 0.001), sex (OR, 0.84; 95% CI, 0.75–0.95; p = 0.004), square-root BMI (OR, 1.05; 95% CI, 0.99–1.11; p = 0.140), diabetes (OR, 1.32; 95% CI, 1.17–1.48; p < 0.001), osteoarthritis (OR, 1.16; 95% CI, 0.84–1.62; p = 0.368), posttraumatic arthritis (OR, 1.66; 95% CI, 1.07–2.56; p = 0.022), and osteonecrosis (OR, 2.54; 95% CI, 1.31–4.92; p = 0.006). The best predictors for the THA revision risk calculator were sex (OR, 1.24; 95% CI, 1.05–1.46; p = 0.010), age (OR, 0.98; 95% CI, 0.98–0.99; p < 0.001), square-root BMI (OR, 1.07; 95% CI, 1.00–1.15; p = 0.066), and osteoarthritis (OR, 0.85; 95% CI, 0.66–1.09; p = 0.190).
Conclusions
Study model parameters can be used to create web-based calculators. Surgeons can enter personalized patient data in the risk calculators for identification of risk of revision which can be used for clinical decision making at the point of care. Future prospective studies will be needed to validate these calculators and to refine them with time.
Level of Evidence
Level III, prognostic study.
Similar content being viewed by others
Introduction
Total joint arthroplasty is a high-volume and high-cost procedure that can reduce pain and restore function in patients with osteoarthritis [8, 29, 36]. Although most joint arthroplasties can last 15 to 20 years, some fail earlier because of wear and osteolysis, instability, infection, or other causes [1, 10, 32, 34]. These failures often result in revision surgery, which is associated with a greater risk of morbidity and mortality than primary total joint arthroplasty [4, 27]. Not only do revision procedures have a greater risk for complications and mortality, but they also are costly, with complicated revisions sometimes resulting in charges approaching or exceeding USD 100,000 [7, 24].
To minimize the demand of revision total joint arthroplasties, risk factors for failures leading to revisions must be identified. Various factors associated with revision total knee arthroplasty (THAs) and total hip arthroplasty (TKAs) have been reported, including age, sex, diagnosis, BMI, and comorbidities [13, 19, 21, 31, 40]. These known risk factors provide a basis for developing clinical decision aids for patients and surgeons to decide on treatment options after assessing patient-specific risk factors and consequently reduce the risk of revision surgery and enhance quality of care.
Risk calculators are a type of clinical tool that can be used to predict the probability of complications or revisions. Although risk calculators have been created for various diagnoses, procedures, and outcomes, and are used in a range of settings [2, 3, 5, 6, 16, 18, 22, 26, 35, 42–45], risk calculators for total joint arthroplasties have not been developed and fully integrated in large healthcare settings. One risk calculator for periprosthetic joint infection and mortality after THA has been developed however, it was developed only for the Medicare population [5].
The purpose of our study is to describe the development and integration of patient risk calculators, one for revision after THA and one for revision after TKA, for use in a large integrated healthcare system, and to highlight the value of a population-based total joint replacement registry. Although we have used the risk calculators in our large integrated healthcare system (Kaiser Permanente), the results and model parameters were not published. Additional followup for our study population provided an opportunity to update our model parameters and share them for external use and validation. In this study, we sought to develop a TKA and a THA revision risk calculator, using data from a large health-maintenance organization’s arthroplasty registry and determine the best set of predictors for the revision risk calculator.
Materials and Methods
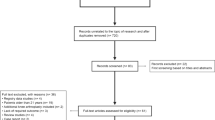
We developed revision risk calculators by means of cross-sectional analyses of prospectively collected data from Kaiser Permanente’s Total Joint Replacement Registry, comprising data for hip and knee arthroplasties. Kaiser Permanente is an integrated health care system in eight regions of the United States: Northern California, Southern California, Colorado, Northwest, Hawaii, Mid-Atlantic States, Ohio, and Georgia. Registry data collection and validation methods have been described [33, 34]. In brief, the registry uses electronic and paper-based data collection methods to identify patient characteristics, implant, and surgical information. All procedures performed at our institution are captured by the registry . Chart review is conducted to validate the outcomes of interest, including revision. All patients undergoing TKAs (Fig. 1) and TKAs (Fig. 2) registered in the total joint replacement registry between April 2001 and July 2008 were included in the study and followed for a 5-year period (TKAs, n = 41,750; THAs, n =22,721). During the study period, 9% of patients (TKA = 3066/34,686; THA =1898/20,285) were lost to followup owing to membership termination and 7% of patients (TKA = 2350/41,750; THA = 1419/20,285) died. Records with a missing value for any candidate predictor were handled using multiple imputation with Markov chain Monte Carlo method. M = six imputations were created. For the model building step, the M-imputed datasets were stacked into one and a 1/M weight was used to account for the missing data in each covariate. Parameters in the final models were combined with Rubin’s rule. Prediction models were developed using a sample that had at least 5 years followup from the available data for the corresponding registry [14]. The sample included 20,592 primary THAs, of which 641 (3.1%) were revised within 5 years postoperatively, and 38,071 primary TKAs, of which 1238 (3.3%) were revised within 5 years postoperatively. Followup for patients with THAs was mean 7.6 years (SD, 1.9) and median 7.4 years (interquartile range [IQR], 6.1–9.0). Followup for patients with TKAs was mean 7.6 years (SD, 1.9) and median 7.2 years (IQR, 6.0–8.8). The cumulative incidence curves for revision TKA (Fig. 3) and THA are provided (Fig. 4). Institutional review board approval was obtained for this study.
We solicited input from Kaiser Permanente lead arthroplasty registry surgeons from each of the eight regions (Northern California, Southern California, Hawaii, Northwest, Colorado, Mid-Atlantic, Georgia and Ohio) regarding what variables to consider for use in our revision risk calculators. Variables for possible use were discussed on the basis of aiming to produce a first-generation revision risk calculator that would be as simple and intuitive as possible, consistent with predictive power, that would involve only variables known or knowable at a presurgical office consultation. Candidate predictors included age, sex, BMI, diabetes (yes/no), osteoarthritis (yes/no), inflammatory arthritis (yes/no), posttraumatic arthritis (yes/no), rheumatoid arthritis (yes/no), and osteonecrosis (yes/no). On this basis, the American Society of Anesthesiologists score, for example, although having apparent predictive power but not available before the time of the procedure, could not be considered for these prediction models.
For hips and knees individually, various subsets of candidate predictors were examined. Those with higher predictive power were input to a program, the mfp (multivariable fractional polynomial) macro [30, 39], to see what functional form of each continuous predictor (BMI, age) might be best for our prediction models. The mfp macro can test a wide variety of prespecified functional forms for each continuous predictor, such as linear, second and third powers, square and cube roots, inverse and log transforms, and two-term sums of such transformations, and it can select an optimal model based on default or specified selection criteria. Although use of restricted cubic splines would be an alternative approach to capturing functional form, the mfp approach provided the prospect of combining flexible functional form modeling with being able to understand the functional form involved in terms of a relatively simple, small number of standard polynomial, and other familiar mathematical forms [38]. Some interaction terms were examined.
Given its status, unlike some other candidate risk factors as potentially modifiable before surgery, we aimed to assess the role of BMI in predicting revision as carefully as possible to facilitate insight in how weight reduction might possibly decrease the risk of revision surgery. We used the mfp macro to examine a large variety of possible functional forms for BMI in particular; for our knee risk predictor, for example, we checked functions of BMI through the fifth power and the fourth power with various functional forms for age and various transforms of BMI on cases with restricted ranges of BMI values.
Both of our calculators model the risk of a first subsequent revision of any cause within 5 years postoperatively and do not consider any possible subsequent revisions of the same procedure. Risk of revision was modeled by logistic regression. Although a wide variety of methods for developing prediction models is available, our approach was guided with the intent to combine predictive ability with understanding and assessing the clinical plausibility and relevance of the contribution of each predictor used in our models, which could facilitate acceptance and use among surgeons and patients. We therefore avoided predictive models that do not provide insights regarding the parameter being approximated. Candidate predictors were selected from preoperative patient characteristics on the basis of clinical knowledge with an additional criterion of being readily available from an integrated healthcare system’s routinely collected data (for example, outpatient and inpatient electronic health record, administrative data, and Geographically Enriched Member Sociodemographics data) or easily determinable at the time of consultation.
We used the c-statistic in combination with the Hosmer-Lemeshow goodness-of-fit criterion to do initial sorting of candidate models. Second-round selection of models was based on assessment by the c-statistic criterion alone. Cross-validation for model checking and final selection from among the five prediction models with the best c-statistic was done using 90% to 95% subsamples, specifically, 10 samples each consisting of 95% of the original data (simple random sampling) were used to evaluate the models [14]. In addition, the observed and predicted numbers of revisions by revision risk probability deciles were compared.
Sensitivity Analysis
Adjustment for patient clustering (some patients had both knees or both hips replaced) had no effect on results and therefore was not included in final models. Interaction terms were tested but not retained because they did not improve any of the models.
All analyses were performed in SAS® 9.1.3 (SAS Institute Inc, Cary, NC, USA).
Results
Knee Revision Risk Calculator
Predictors selected for the final model included age, BMI, gender, diabetes (yes/no), osteoarthritis (yes/no), posttraumatic arthritis (yes/no), and osteonecrosis (yes/no). The square-root of BMI was used, whereas age was incorporated as a linear term (Table 1). Our knee model predicted well in the lowest and midrange decile of risk, lowest: 56 revisions predicted versus an observed 60, and 6th decile: 119 revision predicted versus and 117 observed, and did least well in the highest decile (Table 2). Patients in the highest decile of risk were four times more likely to have a revision TKA than those in the lowest decile of risk, with the most risky 10% of patients experiencing 22% of all revisions and the least risky 10% undergoing 5% of all revisions (Fig. 5).
Hip Revision Risk Calculator
Predictors selected for the final model were gender, BMI, age, and osteoarthritis. Similar to the final knee risk prediction model, the square-root of BMI and linear term of age were used (Table 3).The hip model predicted less well in the highest decile than the knee model, 99 predicted cases versus an observed 104, but better in the midrange and lowest decile, where it predicted 43 cases versus an observed 56 (Table 2). Patients in the highest decile of risk were 1.9 times more likely to have a revision THA than those in the lowest decile of risk, with the most risky 10% of patients experiencing 16% of all revisions and the least risky 10% undergoing 9% of all revisions (Fig. 6).
Application Development
Model parameters were entered in Excel (Microsoft® Inc, Redmond, WA, USA) spreadsheet algorithms to allow creation of limited-use websites at which Kaiser Permanente orthopaedic surgeons can now enter patient data to obtain a predicted revision probability. This is given as an absolute risk rather than as any kind of relative risk or odds ratio. For instance, an 81-year-old female, 5 feet, 5 inches tall, 130 pounds (BMI = 21.6 kg/m2) with ostheoarthritis and diabetes, is expected to have a 1.9% risk of revision within 5 years after a TKA. A 50-year-old male, 6 feet tall, 225 pounds (BMI = 30.5 kg/m2), with diabetes, is expected to have a 4.0% risk of revision within 5 years after a THA. The model parameters for the revision risk calculators are provided for external use and validation (Fig. 7).
Other Relevant Findings
Odds ratios for the predictors in the revision risk calculators are shown (Tables 1 and 3). The odds ratios for BMI in each model are not simple to interpret because they represent the increase in odds of revision for a one-unit increase in the square root of BMI. Thus, an increase of BMI from 25 to 26 would involve a √26 − √25 = 5.09902 − 5 = 0.09902 unit increase in square root BMI. Because (1.067322)0.09902 = 1.006472, this increase in BMI represents an approximately 1% increase in the odds of having a revision TKA. For further comparison, a BMI of 40 kg/m2 represents an increase in odds of a knee revision of approximately 6% compared with a BMI of 30 kg/m2.
Discussion
The risks and demands associated with revision TKA and THA are a significant healthcare concern for patients, clinicians, healthcare systems, and payers. Methods to prevent or reduce revision rates can improve care and reduce healthcare costs. This study identified a set of predictor variables for TKA and THA revision risk calculators from a large integrated healthcare system. The model parameters from this study can be used for other patients’ revision risk calculation and validation.
Since the revision risk calculators were based on available data from our integrated healthcare system, generalizability beyond our healthcare system has not been established and is a limitation of the study. However, our patient membership has been shown to reflect the sociodemographic makeup of the entire corresponding census region population for large regional subsets [23]. More extensive validation outside the integrated healthcare system is still necessary to ensure generalizability of these revision risk calculators. The model parameters are specifically included in this study for use and validation of the models beyond our organization and for development and refinement of revision risk calculators in other settings. Another potential limitation of this study is the focus on all-cause revision. Predictors of revisions may differ associated with the mechanism of failure and should be examined in future studies. However, all-cause revision is a standard endpoint for many registry-related studies. Missing BMI values (3%) also were a study limitation but they were addressed using multiple imputation. Finally, the study focused on 5-year revision rates and does not evaluate longer-term (eg, 10-20 years) risk of revision.
Similar to other studies that have examined revision risk factors, we identified sex, age, BMI, diagnosis, and diabetes as patient risk factors of revision [17, 28, 40, 41]. Two studies [5, 37] examined predictors for inclusion in total joint arthroplasty risk calculators. One study [5] investigated periprosthetic joint infection and mortality but was limited to Medicare administrative data and did not evaluate longer-term risk of revision [5]. Another study [37] examined perioperative risk predictors for use in a risk calculator but was limited to one institution and did not evaluate risk of revision. THA and TKA revision rates in our study were similar to published rates [9, 11, 12, 15]. Revision per 100 observation-years was slightly lower than those reported by other national registries [25]. In addition, revision burden was lower than that reported by Medicare [20, 24]. The similarities in findings suggest that our revision risk calculators may generalize to other settings.
The THA and TKA risk calculators are used in our system for clinical decision making at the point of care. Clinical applications of these calculators include weight counseling to show the reduction in risk associated with ideal versus current weight, management of preoperative anxiety by providing patients with their personalized risk so they understand the procedure and their potential results, addressing diabetic concerns regarding complication risks so they know complication risk may be slightly higher but that they are candidates for good outcomes, and setting patient expectations, such as for younger patients in particular who want to know how long the prosthesis will last.
The next versions of these revision risk calculators should benefit from surgeon feedback concerning additional candidate predictors to examine, such as prior knee surgery for the knee revision risk calculator, steroid use, hemoglobin A1c levels, and ways to improve calculator web site interface design. They also will have more risk data from more cases, with several years more followup, and with reduced numbers of missing data in predictors such as BMI. They also may benefit from the availability of substantially expanded amounts of information in registry data on comorbidities (and racial/ethnic classification), which creates the possibility of including some of these variables as predictors. In addition, implant and surgical technique variables may further expand the predictive use of these tools to consider a range of possible options for surgery for a given patient. Finally, the incorporation of implant, procedure, surgeon, and/or site-specific information that becomes available at or after the time of surgery may facilitate the development of postoperative risk calculators that lead to more refined surveillance and monitoring after a joint arthroplasty.
TKA and THA revision risk calculators were predictive of revision and were integrated in our healthcare setting using a web-based system. The model parameters are presented for use by other patients and clinicians in various settings and for external validation. Identification of risk factors to influence treatment decisions may reduce revision total joint arthroplasties and enhance quality of care.
References
Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2014. Adelaide, 2014. Available at https:// https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2014. Accessed July 27, 2015.
Bilimoria KY, Liu Y, Paruch JL, Zhou L, Kmiecik TE, Ko CY, Cohen ME. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217:833–842.e1-3.
Bolland MJ, Siu AT, Mason BH, Horne AM, Ames RW, Grey AB, Gamble GD, Reid IR. Evaluation of the FRAX and Garvan fracture risk calculators in older women. J Bone Miner Res. 2011;26:420–427.
Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am. 2005;87:570–576.
Bozic KJ, Ong K, Lau E, Berry DJ, Vail TP, Kurtz SM, Rubash HE. Estimating risk in Medicare patients with THA: an electronic risk calculator for periprosthetic joint infection and mortality. Clin Orthop Relat Res. 2013;471:574–583.
D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753.
DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2007;165:1–209.
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963–974.
Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, Havelin LI. Early failures among 7,174 primary total knee replacements: a follow-up study from the Norwegian Arthroplasty Register 1994–2000. Acta Orthop Scand. 2002;73:117–129.
Garellick G, Kärrholm J, Rogmark C, Herberts P. Swedish Hip Arthroplasty Register Annual Report 2009. Gothenburg, 2010. Available at http://www.shpr.se/en/Publications/DocumentsReports.aspx. Accessed June 29, 2015.
Gioe TJ, Killeen KK, Grimm K, Mehle S, Scheltema K. Why are total knee replacements revised?: analysis of early revision in a community knee implant registry. Clin Orthop Relat Res. 2004;428:100–106.
Graves SE, Davidson D, Ingerson L, Ryan P, Griffith EC, McDermott BF, McElroy HJ, Pratt NL. The Australian Orthopaedic Association National Joint Replacement Registry. Med J Aust. 2004;180(5 suppl):S31–34.
Hagen TP, Vaughan-Sarrazin MS, Cram P. Relation between hospital orthopaedic specialisation and outcomes in patients aged 65 and older: retrospective analysis of US Medicare data. BMJ. 2010;340:c165.
Harrell FE Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York, NY: Springer; 2001.
Herberts P, Malchau H. Long-term registration has improved the quality of hip replacement: a review of the Swedish THR Register comparing 160,000 cases. Acta Orthop Scand. 2000;71:111–121.
Jelovsek JE, Chagin K, Brubaker L, Rogers RG, Richter HE, Arya L, Barber MD, Shepherd JP, Nolen TL, Norton P, Sung V, Menefee S, Siddiqui N, Meikle SF, Kattan MW; Pelvic Floor Disorders Network. A model for predicting the risk of de novo stress urinary incontinence in women undergoing pelvic organ prolapse surgery. Obstet Gynecol. 2014;123:279–287.
Julin J, Jamsen E, Puolakka T, Konttinen YT, Moilanen T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis: a follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop. 2010;81:413–419.
Kang M, Jeong CW, Choi WS, Park YH, Cho SY, Lee S, Lee SB, Ku JH, Hong SK, Byun SS, Jeong H, Kwak C, Kim HH, Lee E, Lee SE; Seoul National University-Uro-Oncology Group. Pre- and post-operative nomograms to predict recurrence-free probability in Korean men with clinically localized prostate cancer. PLoS One. 2014;9:e100053.
Katz JN, Mahomed NN, Baron JA, Barrett JA, Fossel AH, Creel AH, Wright J, Wright EA, Losina E. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56:568–574.
Katz JN, Wright EA, Wright J, Malchau H, Mahomed NN, Stedman M, Baron JA, Losina E. Twelve-year risk of revision after primary total hip replacement in the U.S. Medicare population. J Bone Joint Surg Am. 2012;94:1825–1832.
Khatod M, Cafri G, Namba RS, Inacio MCS, Paxton EW. Risk factors for total hip arthroplasty aseptic revision. J Arthroplasty. 2014;29:1412–1417.
Kim JY, Mlodinow AS, Khavanin N, Hume KM, Simmons CJ, Weiss MJ, Murphy RX Jr, Gutowski KA. Individualized risk of surgical complications: an application of the Breast Reconstruction Risk Assessment Score. Plast Reconstr Surg Glob Open. 2015;3:e405.
Koebnick C, Langer-Gould AM, Gould MK, Chao CR, Iyer RL, Smith N, Chen W, Jacobsen SJ. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16:37–41.
Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, Karrholm J, Garellick G, Havelin LI, Furnes O, Malchau H, Lau E. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(suppl 3):144–151.
Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293–297.
Lo JC, Pressman AR, Chandra M, Ettinger B. Fracture risk tool validation in an integrated healthcare delivery system. Am J Manag Care. 2011;17:188–194.
Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85:27–32.
Malinzak RA, Ritter MA, Berend ME, Meding JB, Olberding EM, Davis KE. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24(6 suppl):84–88.
Meding JB, Meding LK, Ritter MA, Keating EM. Pain relief and functional improvement remain 20 years after knee arthroplasty. Clin Orthop Relat Res. 2012;470:144–149.
Meier-Hirmer C, Ortseifen C, Sauerbrei W. Macro mfp8, Version 6.5. 2003. Available at: http://people.musc.edu/~hille/2009BMTRY755_Website/LectureNotes/Diagnostics2/MFP2neu/mfp8.sas. Accessed July 7, 2015.
Namba RS, Cafri G, Khatod M, Inacio MC, Brox TW, Paxton EW. Risk factors for total knee arthroplasty aseptic revision. J Arthroplasty. 2013;28(8 suppl):122–127.
National Joint Registry for England, Wales and Northern Ireland. 11th Annual Report 2014. Surgical data to 13 December 2013. Available at http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/11th_annual_report/NJR%2011th%20Annual%20Report%202014.pdf. Accessed June 29, 2015.
Paxton EW, Kiley ML, Love R, Barber TC, Funahashi TT, Inacio MC. Kaiser Permanente implant registries benefit patient safety, quality improvement, cost-effectiveness. Jt Comm J Qual Patient Saf. 2013;39:246–252.
Paxton EW, Namba RS, Maletis GB, Khatod M, Yue EJ, Davies M, Low RB Jr, Wyatt RW, Inacio MC, Funahashi TT. A prospective study of 80,000 total joint and 5000 anterior cruciate ligament reconstruction procedures in a community-based registry in the United States. J Bone Joint Surg Am. 2010;92(suppl 2):117–132.
Puopolo KM, Draper D, Wi S, Newman TB, Zupancic J, Lieberman E, Smith M, Escobar GJ. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics. 2011;128:e1155–1163.
Rolfson O, Karrholm J, Dahlberg LE, Garellick G. Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J Bone Joint Surg Br. 2011;93:867–875.
Romine LB, May RG, Taylor HD, Chimento GF. Accuracy and clinical utility of a peri-operative risk calculator for total knee arthroplasty. J Arthroplasty. 2013;28:445–448.
Royston P, Moons KG, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model. BMJ. 2009;338:b604.
Royston P, Sauerbrei W. Multivariable Model-Building: A Pragmatic Approach to Regression Analysis Based on Fractional Polynomials forModelling Continuous Variables. West Sussex, England: Wiley; 2008.
Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428–436.
Schrama JC, Espehaug B, Hallan G, Engesaeter LB, Furnes O, Havelin LI, Fevang BT. Risk of revision for infection in primary total hip and knee arthroplasty in patients with rheumatoid arthritis compared with osteoarthritis: a prospective, population-based study on 108,786 hip and knee joint arthroplasties from the Norwegian Arthroplasty Register. Arthritis Care Res (Hoboken). 2010;62:473–479.
Shabir S, Halimi JM, Cherukuri A, Ball S, Ferro C, Lipkin G, Benavente D, Gatault P, Baker R, Kiberd B, Borrows R. Predicting 5-year risk of kidney transplant failure: a prediction instrument using data available at 1 year posttransplantation. Am J Kidney Dis. 2014;63:643–651.
Sheridan S, Pignone M, Mulrow C. Framingham-based tools to calculate the global risk of coronary heart disease: a systematic review of tools for clinicians. J Gen Intern Med. 2003;18:1039–1052.
Sherman SK, Hrabe JE, Charlton ME, Cromwell JW, Byrn JC. Development of an improved risk calculator for complications in proctectomy. J Gastrointest Surg. 2014;18:986–994.
Watts NB, Lewiecki EM, Miller PD, Baim S. National Osteoporosis Foundation 2008 Clinician’s Guide to Prevention and Treatment of Osteoporosis and the World Health Organization Fracture Risk Assessment Tool (FRAX): what they mean to the bone densitometrist and bone technologist. J Clin Densitom. 2008;11:473–477.
Acknowledgments
We thank all the Kaiser Permanente orthopaedic surgeons who contribute to the Total Joint Replacement Registry and the Surgical Outcomes and Analysis Department, which coordinates Registry operations.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Kaiser Permanente, San Diego, CA, USA.
About this article
Cite this article
Paxton, E.W., Inacio, M.C.S., Khatod, M. et al. Risk Calculators Predict Failures of Knee and Hip Arthroplasties: Findings from a Large Health Maintenance Organization. Clin Orthop Relat Res 473, 3965–3973 (2015). https://doi.org/10.1007/s11999-015-4506-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4506-4