Abstract
Background
Osteoporosis may complicate surgical fixation and healing of proximal humerus fractures and should be assessed preoperatively. Peripheral quantitative CT (pQCT) and the Tingart measurement are helpful methods, but both have limitations in clinical use because of limited availability (pQCT) or fracture lines crossing the area of interest (Tingart measurement). The aim of our study was to introduce and validate a simple cortical index to assess the quality of bone in proximal humerus fractures using AP radiographs.
Questions/purposes
We asked: (1) How do the deltoid tuberosity index and Tingart measurement correlate with each other, with patient age, and local bone mineral density (BMD) of the humeral head, measured by pQCT? (2) Which threshold values for the deltoid tuberosity index and Tingart measurement optimally discriminate poor local bone quality of the proximal humerus? (3) Are the deltoid tuberosity index and Tingart measurement clinically applicable and reproducible in patients with proximal humerus fractures?
Methods
The deltoid tuberosity index was measured immediately above the upper end of the deltoid tuberosity. At this position, where the outer cortical borders become parallel, the deltoid tuberosity index equals the ratio between the outer cortical and inner endosteal diameter. In the first part of our study, we retrospectively measured the deltoid tuberosity index on 31 patients (16 women, 15 men; mean age, 65 years; range, 22–83 years) who were scheduled for elective surgery other than fracture repair. Inclusion criteria were available native pQCT scans, AP shoulder radiographs taken in internal rotation, and no previous shoulder surgery. The deltoid tuberosity index and the Tingart measurement were measured on the preoperative internal rotation AP radiograph. The second part of our study was performed by reviewing 40 radiographs of patients with proximal humerus fractures (31 women, nine men; median age, 65 years; range, 22–88 years). Interrater (two surgeons) and intrarater (two readings) reliabilities, applicability, and diagnostic accuracy were assessed.
Results
The correlations between radiograph measurements and local BMD (pQCT) were strong for the deltoid tuberosity index (r = 0.80; 95% CI, 0.63–0.90; p < 0.001) and moderate for the Tingart measurement (r = 0.67; 95% CI, 0.42–0.83; p < 0.001). There was moderate correlation between patient age and the deltoid tuberosity index (r = 0.65; p < 0.001), patient age and the Tingart measurement (r = 0.69; p < 0.001), and patient age and pQCT (r = 0.73; p < 0.001). The correlation between the deltoid tuberosity index and the Tingart measurement was strong (r = 0.84; p < 0.001). We determined the cutoff value for the deltoid tuberosity index to be 1.44, with the area under the curve = 0.87 (95% CI, 0.74–0.99). This provided a sensitivity of 0.88 and specificity of 0.80. For the Tingart measurement, we determined the cutoff value to be 5.3 mm, with the area under the curve = 0.83 (95% CI, 0.67–0.98), which resulted in a sensitivity of 0.81 and specificity of 0.85. The intraobserver reliability was high and not different between the Tingart measurement (intraclass correlation coefficients [ICC] = 0.75 and 0.88) and deltoid tuberosity index (ICC = 0.88 and 0.82). However, interobserver reliability was higher for the deltoid tuberosity index (ICC = 0.96; 95% CI, 0.93–0.98) than for the Tingart measurement (ICC = 0.85; 95% CI, 0.69–0.93).The clinical applicability on AP radiographs of fractures was better for the deltoid tuberosity index (p = 0.025) because it was measureable on more of the radiographs (77/80; 96%) than the Tingart measurement (69/80; 86%).
Conclusions
The deltoid tuberosity index correlated strongly with local BMD measured on pQCT and our study evidence shows that it is a reliable, simple, and applicable tool to assess local bone quality in the proximal humerus. We found that deltoid tuberosity index values consistently lower than 1.4 indicated low local BMD of the proximal humerus. Furthermore, the use of the deltoid tuberosity index has important advantages over the Tingart measurement regarding clinical applicability in patients with proximal humerus fractures, when fracture lines obscure the Tingart measurement landmarks. However, further studies are needed to assess the effect of the deltoid tuberosity index measurement and osteoporosis on treatment and outcome in patients with proximal humerus fractures.
Level of Evidence
Level IV, diagnostic study.
Similar content being viewed by others
Introduction
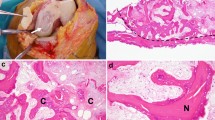
The influence of local bone mineral density (BMD) on the outcome of proximal humerus fractures is controversial and not sufficiently addressed in the literature [7, 12, 13]. However, several studies have shown that osteoporosis may negatively affect surgical fixation or healing of proximal humerus fractures after open reduction and internal fixation (ORIF). For example Fankhauser et al. [7] found low BMD to negatively affect the stability of ORIF of the proximal humerus in their cadaver study. However Krappinger et al. [13] found low BMD to be a predictor for later failure of ORIF in their clinical study. Thus they agree with other authors that bone quality should be part of the preoperative assessment [7, 10, 13, 19, 20]. Dual-energy x-ray absorptiometry (DXA) is the gold standard for assessing osteoporosis in patients, however it is valid only for specific anatomic sites which do not include the proximal humerus. There is evidence, however, that the BMD of the upper limb (distal radius) is less than that of typically measured sites (such as the proximal femur and lumbar spine) in patients with proximal humerus fractures [27]. Thus, preoperative assessment of BMD of the proximal humerus has become the focus of some studies, with methods ranging from measuring the cortical thickness on AP radiographs, to calculating BMD on peripheral quantitative CT (pQCT) scans [6, 8, 9, 14, 16, 21, 25, 26]. Barnett and Nordin [3] were the first to invent a cortical index to assess local bone quality of the hand and femur. The combined cortical thickness (Tingart measurement [18]) is the most frequently reported method used to measure bone quality on AP radiographs of the shoulder (Fig. 1).
The two levels of combined cortical thickness are level 1, at the proximal diaphysis where the medial and the lateral endosteal cortical borders become parallel; and level 2, which is 2 cm distal to level 1. The sum of the means of the two levels is calculated and must be corrected for magnification error.
The Tingart measurement has been proven to correlate with DXA measurements of different anatomic sites [16], however, it has not been validated for patients with proximal humerus fractures. Furthermore, with that injury, the landmarks required for the Tingart measurement often are involved in the fracture (Figs. 1 and 2). Another disadvantage of the Tingart measurement is that the absolute value in millimeters needs to be corrected for radiographic magnification errors and a reference is not always available on the radiograph. However, being more distant to the fracture site, the deltoid tuberosity usually is well outlined (Fig. 2), as seen in the analysis of fracture from AP radiographs, possibly owing to the internally rotated, relieving posture of the arm.
An AP radiograph shows a proximal humerus fracture in a 75-year-old patient. The proximal diaphysis is fractured, which complicates the definition of the levels for the Tingart measurement. The deltoid tuberosity index is measured directly proximal to the deltoid tuberosity (asterisks), where the outer cortical borders become parallel. At this level, the ratio between the outer cortical and the inner endosteal diameter is calculated (a/b).
Our aims in this study are to define and validate an easy, one-step cortical index close to the deltoid tuberosity to simplify measurement of bone quality in proximal humerus fractures. Specifically, we asked (1) How do the deltoid tuberosity index and the Tingart measurement correlate with each other, with patient age, and local BMD of the humeral head, measured by pQCT? (2) Which threshold values for the deltoid tuberosity index and the Tingart measurement optimally discriminate poor local bone quality of the proximal humerus? (3) Are the deltoid tuberosity index and the Tingart measurement clinically applicable and reproducible in patients with proximal humerus fractures?
Patients and Methods
Measurement of the Deltoid Tuberosity Index
To measure the deltoid tuberosity index on an AP radiograph of the shoulder, the arm has to be internally rotated (lying on the abdomen) as it usually is with proximal humerus fractures. The location for calculating the deltoid tuberosity index is defined as directly proximal to the deltoid tuberosity where the outer cortical borders become parallel. It is calculated by dividing the outer cortical by the inner endosteal diameter at this level (Fig. 2). Measurements were done electronically with the length-measuring tool provided by IMPAX™ (AGFA HealthCare Corporation, Greenville, SC, USA).
First Part of the Study (Not Fractured Shoulders): Accuracy of Deltoid Tuberosity Index and Tingart Measurement
In the first part of the study, we determined the accuracy of the deltoid tuberosity index and the Tingart measurement in predicting local bone quality of the humeral head. Therefore, we retrospectively analyzed radiographic data of patients without fractures. These patients either had a stabilization procedure or shoulder arthroplasty planned in our institution between May and December 2013. Our standard preoperative investigations for these procedures include pQCT and a series of shoulder radiographs (AP in internal rotation, AP in neutral rotation, axial and lateral/outlet views). Thus, inclusion criteria were available native pQCT scans, digital AP internal rotation radiograph (with reference for correction of magnification error), and no previous shoulder surgery. A total of 31 patients could be included (16 women, 15 men; eight with instability, 23 with arthritis; mean age, 65 years; range, 22–83 years). The deltoid tuberosity index and the Tingart measurement were measured on the internal rotation radiograph by the first author (CS) and the Tingart measurement was corrected for the radiographic magnification error. A radiologist (NK) independently analyzed the BMD of the same shoulders on pQCT, using a validated protocol for the proximal humerus [14]. Measurement of the cancellous bone of the humeral head was used as the standard of reference for local BMD, as this area is the most common location of failure after ORIF for proximal humerus fractures [11, 24]. Correlations between the deltoid tuberosity index and the Tingart measurement, between the deltoid tuberosity index and the Tingart measurement and BMD of the humeral head, and between the deltoid tuberosity index and Tingart measurement and age were calculated. Furthermore, a threshold value for diagnosis of low local BMD was defined using a pQCT cutoff value less than 80 mg/cm3 [2].
Second Part of the Study (Fractured Shoulders): Clinical Reproducibility and Applicability of the Deltoid Tuberosity Index and Tingart Measurement
In the second part of the study, we assessed the clinical reproducibility and reliability of the deltoid tuberosity index and the Tingart measurement. Therefore, we retrospectively analyzed patients with radiographically confirmed proximal humerus fractures who were treated operatively (locking plate ORIF) in our institution between January 2008 and December 2010. Inclusion criteria were available digital AP radiographs of the fracture and no previous shoulder surgery or injury. Using these criteria, a total of 134 patients could be included. Of these, we randomly chose 40 patients (31 women, nine men; mean age, 65 years; range, 22–88 years) for further radiographic analysis, which was thought to be an adequate number for assessment of intra- and interobserver correlations (no power analysis was performed). These patients were randomly selected from the total using their anonymized identification numbers. The first author (CS) then classified the fractures based on the AP and lateral radiographs according to the Neer classification [17, 18]: there were 29 two-part fractures, five three-part fractures, and six four-part fractures. Two orthopaedic consultants (CS and EB) independently measured the (Fig. 2) deltoid tuberosity index and the Tingart measurement [25] twice on the AP radiographs. The interval between the two readings was more than 4 weeks. We did not correct the Tingart measurement for the magnification error as not all of the AP radiographs had a specific reference. Based on results of the readings, intra- and interobserver correlations were calculated.
To test the clinical applicability of the deltoid tuberosity index and the Tingart measurement on fracture radiographs, both observers had to decide which of the two techniques was possible for each case in each reading. However, only the results of the first reading of each observer were used for further statistical analysis (total n = 80), as the second reading was considered not completely independent.
Statistics
Statistical analysis was performed using R (R Foundation for Statistical Computing, Vienna, Austria) [22].
First Part of the Study (Not Fractured Shoulders): Accuracy of the Deltoid Tuberosity Index and the Tingart Measurement
Correlations (deltoid tuberosity index, Tingart measurement, age, BMD (pQCT)) were calculated using the Pearson product moment correlation. Correlations were considered strong for r greater than 0.75, moderate for 0.5 < r < 0.75, poor for 0.25 < r < 0.5 and no correlation for r < 0.25. We performed receiver operating characteristic (ROC) curve analysis [1] based on the cutoff value of BMD less than 80 mg/cm3. The area under the curve (AUC), diagnostic accuracy, and optimal threshold values for the deltoid tuberosity index and the Tingart measurement were calculated. We used the method of Delong et al. [5] for two correlated ROC curves to test if the differences were significant.
Second Part of the Study (Fractured Shoulders): Clinical Reproducibility and Applicability of the Deltoid Tuberosity Index and the Tingart Measurement
The intra- and interobserver reliabilities of the deltoid tuberosity index and Tingart measurement were estimated with intraclass correlation coefficients (ICC) (ICC Model 2 for intraobserver and ICC Model 2k for interobserver variability) [23].
A chi-square test with a p less than 0.05 was used to compare the total numbers of readings where the deltoid tuberosity index and/or the Tingart measurement were applicable.
Ethics
The institutional review board approved this study and all patients gave informed consent to use and publish their anonymized data.
Results
First Part of the Study (Not Fractured Shoulders): Accuracy of the Deltoid Tuberosity Index and the Tingart Measurement
Median values (SD) for the 31 patients without fracture were: deltoid tuberosity index 1.44 (0.19), Tingart measurement 5.4 mm (1.4 mm), and BMD 85.5 mg/ cm3 (31.5 mg/ cm3).
The correlations between radiograph measurements and local BMD (pQCT) were strong for the deltoid tuberosity index (r = 0.80; 95% CI, 0.63–0.90; p < 0.001) and moderate for the Tingart measurement (r = 0.67; 95% CI, 0.42–0.83; p < 0.001) (Fig. 3). There was moderate correlation between patient age and the deltoid tuberosity index (r = 0.65; p < 0.001), patient age and the Tingart measurement (r = 0.69; p < 0.001), and patient age and pQCT (r = 0.73; p < 0.001). The correlation between the deltoid tuberosity index and the Tingart measurement was strong (r = 0.84; p < 0.001) (Fig. 4).
We determined the cutoff value for the deltoid tuberosity index to be 1.44 (AUC = 0.87; 95% CI, 0.74–0.99). This provided a sensitivity of 0.88 and specificity of 0.80. For the Tingart measurement, we determined the cutoff value to be 5.3 mm (AUC = 0.83; 95% CI, 0.67–0.98), which resulted in a sensitivity of 0.81 and a specificity of 0.85. Comparing the AUCs between the deltoid tuberosity index and Tingart measurement revealed no difference (DeLong’s test, p = 0.51) (Fig. 5).
Second Part of the Study (Fractured Shoulders): Clinical Reproducibility and Applicability of the Deltoid Tuberosity Index and the Tingart Measurement
The median deltoid tuberosity index values (SD) were 1.44 (0.10) for Reader 1 (CS) and 1.47 (0.12) for Reader 2 (EB). The intraobserver reliability was high and not different between the Tingart measurement (ICC = 0.75 and 0.88) and deltoid tuberosity index (ICC = 0.88 and 0.82). However, the interobserver reliability was higher for the deltoid tuberosity index (ICC = 0.96; 95% CI, 0.93–0.98) than for the Tingart measurement (ICC = 0.85; 95% CI, 0.69–0.93). The clinical applicability to AP fracture radiographs was significantly better for the deltoid tuberosity index (p = 0.025) because it was measureable on more of the radiographs (77/80; 96%) than the Tingart measurement (69/80; 86%).
Discussion
Preoperative assessment of local BMD should be part of the treatment plan for patients with proximal humerus fractures [10, 19, 20] and therefore the calculation should be quick and simple on a fracture radiograph. The methods in use have some limitations; for example, the DXA measurement, the gold standard for assessment of osteoporosis, is not specific for the proximal humerus and often not available in case of acute fracture [27]. However, pQCT can be used for local analysis, but the calculation is complicated and special training is needed to perform it [14]. Furthermore, the Tingart measurement as a helpful tool to assess local bone quality on AP radiographs seems to have some major drawbacks in proximal humerus fractures as the fracture lines may obscure the levels of measurement. Thus, we believe the deltoid tuberosity index is a simple radiographic tool specific for proximal humerus fractures. We wished to compare the deltoid tuberosity index with the Tingart measurement in terms of potential to predict local BMD and in terms of clinical use in proximal humerus fractures.
This study has some limitations which require explanations. First, the WHO has no accepted threshold value for osteoporosis of the proximal humerus nor for local DXA or pQCT measurements; therefore, threshold values in our study are approximations for clearly reduced bone quality and their clinical relevance must be further assessed.
Second, the literature regarding the clinical relevance of local BMD on outcome of proximal humerus fracture treatment is scarce and controversial [7, 10, 12, 13]. Some of the clinical studies are biased because most of the included patients with this fracture have osteoporosis [12, 20]. However, we think the deltoid tuberosity index with its easy use may be a helpful tool for further clinical studies on this topic.
Third, the protocol used to analyze pQCT does not imply different regions of interest of the proximal humerus [14]. Thus the correlations could be made only to cancellous bone in the middle of the humeral head; however, the area is representative and an important region, as screws find purchase specifically there [4].
Fourth, the selection of patients with proximal humerus fractures for the second part of the study was done by randomly choosing anonymized identification numbers. It appears that we have a high percentage of two-part fractures in this collective which might be attributable to the strict use of the Neer criteria [17, 18] defining a part only as such if displacement is greater than 1 cm or greater than 45°. However, the difficulties of proximal humerus fracture classifications have not been addressed further as this was not the scope of our study.
Finally, we are not able to provide the absolute Tingart measurement values of our patients with fractures included in the second part of the study, as the reference for correction of magnification was not available on each of the older fracture radiographs. However, this does not affect the results of the ICC calculations where these data were used.
The deltoid tuberosity index and the Tingart measurement correlated strongly with each other, which is not a surprise as the deltoid tuberosity index level of measurement is usually close to level 2 of the Tingart measurement and both techniques measure cortical thickness or the ratio between cortical and endosteal bone. Furthermore, both radiographic measurements correlated moderately to patient age. Mantila Roosa et al. [15] described the osseous changes of the humeral shaft with age. They stated that the outer cortical diameter grows owing to periosteal bone apposition but the inner diameter grows even faster. This might explain the correlation of the radiographic measurements in this area to age and justifies use of a simple ratio between the outer cortical and the inner endosteal diameter to calculate the deltoid tuberosity index. The correlation we found between pQCT and patient age was comparable that reported by to Krappinger et al. [14]. This underlines the good reproducibility of their pQCT protocol for the proximal humerus. In terms of correlation to local BMD, the deltoid tuberosity index performed slightly better than the Tingart measurement. Whereas the latter has been proven to correlate well to DXA measurements of other anatomic sites (distal radius, proximal femur) [16], our study is the first, to our knowledge, to compare the Tingart measurement with local BMD measured by pQCT of the proximal humerus. A possible explanation why the Tingart measurement was at a disadvantage to the deltoid tuberosity index in this respect could be that Tingart defined different regions of interest in the proximal humerus and found the best correlation to BMD of the greater tuberosity [25, 26]. We were not able to account specifically for this region of interest with the pQCT protocol used in our study [14].
We found clinically useful threshold values for the deltoid tuberosity index less than 1.4 and for the Tingart measurement less than 5 mm for determination of low bone quality of the proximal humerus. However, the values need to be considered in light of the fact that there are no accepted pQCT threshold values specific to the proximal humerus. Therefore, we empirically used the pQCT cutoff value less than 80 mg/cm3 to calculate the ROC curve analysis. According to the guidelines of the American College of Radiology, this is meant to be the pQCT value for osteoporosis in the lumbar spine and proximal femur and represents low local bone quality [2]. Therefore, the threshold value less than 1.4 for the deltoid tuberosity index may be only an approximation for low local bone quality of the proximal humerus and further investigations are needed to ensure its clinical relevance in the treatment of fractures. Regarding the Tingart measurement, the originally proposed threshold value (< 4 mm) [25] showed very low sensitivity (only 0.45) in our setting, which is in accordance with findings by Mather et al. [16]. They suggested a possible threshold value less than 6 mm for the Tingart measurement to predict osteoporosis of the proximal femur and the lumbar spine. However, our ROC curve analysis for the Tingart measurement revealed that a threshold value of 5 mm would lead to fair test performance (sensitivity 0.81 and specificity 0.85).
The deltoid tuberosity index and the Tingart measurement showed good inter- and intraobserver reliability, although the deltoid tuberosity index was applicable in more cases when fracture lines obscured the landmarks for the Tingart measurement. Therefore it was our intent to find the simplest possible method to measure local bone quality specifically on AP radiographs of proximal humerus fractures. We are aware that the definition of a cortical index is not new, as others indices have been defined for the proximal humerus [8, 9]; however, we believe the simplicity and the specificity of AP radiographs of fractures are clinical advantages of the deltoid tuberosity index. Furthermore, our study is the first to investigate the Tingart measurement for its clinical use in proximal humerus fractures. The need to correct magnification to calculate the absolute value of the Tingart measurement is a drawback as not every radiograph has the needed reference. Another disadvantage of the Tingart measurement is defining the height of level 1, which is imperative for determining level 2 [25]. This proximal diaphyseal area is often part of the fracture, which makes measurement difficult. The deltoid tuberosity index, on the contrary, is measured in an area seldom affected by fracture and, according to our study, still correlates well with the bone quality of the humeral head.
The deltoid tuberosity index and the Tingart measurement correlated well to local BMD of the proximal humerus measured by pQCT. Compared with the Tingart measurement, the deltoid tuberosity index showed advantages in terms of clinical applicability and thus was an easy and reliable tool to get a quick impression of local bone quality on an AP radiograph of a fracture. As the relevance of local BMD on the outcome of treatment of proximal humerus fractures is controversial and not well discussed in the literature, we think the clinical simplicity of the deltoid tuberosity index may be helpful for further investigations on this topic.
References
Altman DG. Diagnostic tests. Practical Statistics for Medical Research. Boca Raton, FL: CRC Press; 1990:417–418.
American College of Radiology. Practice Parameter for the Performance of Quantitative Computed Tomography (QCT) Bone Densitometry. Available at: http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/QCT.pdf. Accessed March 30, 2015.
Barnett E, Nordin BE. The radiological diagnosis of osteoporosis: a new approach. Clin Radiol. 1960;11:166–174.
Brianza S, Röderer G, Schiuma D, Schwyn R, Scola A, Gebhard F, Tami AE. Where do locking screws purchase in the humeral head? Injury. 2012;43:850–855.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845.
Diederichs G, Korner J, Goldhahn J, Linke B. Assessment of bone quality in the proximal humerus by measurement of the contralateral site: a cadaveric analyze. Arch Orthop Trauma Surg. 2006;126:93–100.
Fankhauser F, Schippinger G, Weber K, Heinz S, Quehenberger F, Boldin C, Bratschitsch G, Szyszkowitz R, Georg L, Friedrich A. Cadaveric-biomechanical evaluation of bone-implant construct of proximal humerus fractures (Neer type 3). J Trauma. 2003;55:345–349.
Giannotti S, Bottai V, Dell’osso G, Donati D, Bugelli G, De Paola G, Guido G. Indices of risk assessment of fracture of the proximal humerus. Clin Cases Miner Bone Metab. 2012;9:37–39.
Hepp P, Theopold J, Osterhoff G, Marquass B, Voigt C, Josten C. Bone quality measured by the radiogrammetric parameter “cortical index” and reoperations after locking plate osteosynthesis in patients sustaining proximal humerus fractures. Arch Orthop Trauma Surg. 2009;129:1251–1259.
Hertel RW. Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int. 2005;16(suppl 2):S65–72.
Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22:542–549.
Kralinger F, Blauth M, Goldhahn J, Kach K, Voigt C, Platz A, Hanson B. The influence of local bone density on the outcome of one hundred and fifty proximal humeral fractures treated with a locking plate. J Bone Joint Surg Am. 2014;96:1026–1032.
Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283–1288.
Krappinger D, Roth T, Gschwentner M, Suckert A, Blauth M, Hengg C, Kralinger F. Preoperative assessment of the cancellous bone mineral density of the proximal humerus using CT data. Skeletal Radiol. 2012;41:299–304.
Mantila Roosa SM, Hurd AL, Xu H, Fuchs RK, Warden SJ. Age-related changes in proximal humerus bone health in healthy, white males. Osteoporos Int. 2012;23:2775–2783.
Mather J, MacDermid JC, Faber KJ, Athwal GS. Proximal humerus cortical bone thickness correlates with bone mineral density and can clinically rule out osteoporosis. J Shoulder Elbow Surg. 2013;22:732–738.
Neer CS 2nd. Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089.
Neer CS 2nd. Displaced proximal humeral fractures: II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52:1090–1103.
Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD. Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am. 2007;89(suppl 3):44–58.
Olerud P, Ahrengart L, Söderqvist A, Saving J, Tidermark J. Quality of life and functional outcome after a 2-part proximal humeral fracture: A prospective cohort study on 50 patients treated with a locking plate. J Shoulder Elbow Surg. 2010;19:814–822.
Osterhoff G, Diederichs G, Tami A, Theopold J, Josten C, Hepp P. Influence of trabecular microstructure and cortical index on the complexity of proximal humeral fractures. Arch Orthop Trauma Surg. 2012;132:509–515.
R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. 2012: ISBN 3-900051-07-0. Available at: http://www.R-project.org/. Accessed April 15, 2015.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428.
Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M. The PHILOS plate for proximal humeral fractures: risk factors for complications at one year. J Trauma Acute Care Surg. 2012;72:783–792.
Tingart MJ, Apreleva M, Stechow von D, Zurakowski D, Warner JJ. The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus. J Bone Joint Surg Br. 2003;85:611–617.
Tingart MJ, Lehtinen J, Zurakowski D, Warner JJ, Apreleva M. Proximal humeral fractures: Regional differences in bone mineral density of the humeral head affect the fixation strength of cancellous screws. J Shoulder Elbow Surg. 2006;15:620–624.
Wilson J, Bonner TJ, Head M, Fordham J, Brealey S, Rangan A. Variation in bone mineral density by anatomical site in patients with proximal humeral fractures. J Bone Joint Surg Br. 2009;91:772–775.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Spross, C., Kaestle, N., Benninger, E. et al. Deltoid Tuberosity Index: A Simple Radiographic Tool to Assess Local Bone Quality in Proximal Humerus Fractures. Clin Orthop Relat Res 473, 3038–3045 (2015). https://doi.org/10.1007/s11999-015-4322-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4322-x