Abstract
Background
Restoration of posterior condylar offset during TKA is believed to be important to improving knee kinematics, maximizing ROM, and minimizing flexion instability. However, controversy exists regarding whether there are important anatomic differences between sexes and whether a unisex knee prosthesis can restore the anatomy of knees in males and females.
Questions/purposes
The purposes of our study were to determine if sex differences exist in (1) absolute posterior condylar offset size, (2) relative posterior condylar offset size in relation to total condylar height, and (3) posterior condylar articular cartilage thickness.
Methods
We identified 100 patients (50 men and 50 women) without a history of arthritis, deformity, dysplasia, osteochondral defect, fracture, or surgery about the knee who had MRI of the knee performed. All MR images were ordered by primary care medical physicians for evaluation of nonspecific knee pain. Using a previously described three-dimensional MRI protocol, we measured posterior condylar offset, total condylar height, and articular cartilage thickness at the medial and lateral femoral condyles and compared values to evaluate for potential sex differences. We performed an a priori power calculation using a 2-mm posterior condylar offset difference as the minimum clinically important difference; with 2n = 100, our power to detect such a difference was 99.8%.
Results
Compared with females, males had greater medial posterior condylar offset (30 mm [95% CI, 29.3–30.7 mm; SD, 2.5 mm] vs 28 mm [95% CI, 27.0–28.5 mm; SD, 2.7 mm]), lateral posterior condylar offset (27 mm [95% CI, 26.2–27.3 mm; SD, 2.0 mm] vs 25 mm [95% CI, 24.2–25.4 mm; SD, 2.0 mm]), medial condylar height (63 mm [SD, 3.2 mm] vs 57 mm [SD, 4.4 mm]), and lateral condylar height (71 mm [SD, 5.2 mm] vs 65 mm [SD: 4.0 mm]) (all p values < 0.001). However, the mean ratio of medial posterior condylar offset to medial condylar height (0.48 [SD, 0.04] vs 0.49 [SD, 0.05]) and the mean ratio of lateral posterior condylar offset to lateral condylar height (0.38 [SD, 0.05] vs 0.38 [SD, 0.03]) were not different between sexes (p = 0.08 and p = 0.8, respectively). There also was no sex difference in mean articular cartilage thickness at either condyle (medial condyle: 2.7 mm [SD, 0.5 mm] vs 2.5 mm [SD, 0.7 mm]; lateral condyle: 2.6 mm [SD, 0.6 mm] vs 2.5 mm [SD, 0.8 mm]) (both p values ≥ 0.1).
Conclusions
Results of our study showed that knees in males exhibited greater posterior condylar offset and greater total condylar height at the medial and lateral femoral condyles, however, there were no sex differences in the ratio of posterior condylar offset to condylar height at either condyle.
Clinical Relevance
These findings suggest that a unisex knee prosthesis design is adequate to recreate the normal posterior condylar offsets for men and women.
Similar content being viewed by others
Introduction
The concept of restoration of the posterior condylar offset of the knee during TKA to maximize ROM and avoid impingement originally was described by Bellemans et al. [2]. They defined posterior condylar offset as “the maximal thickness of the posterior condyle, projected posteriorly to the tangent of the posterior cortex of the femoral shaft” as measured on true lateral radiographs [2]. Subsequent studies have shown that restoration of the relationship between the posterior articular surface of the femur and the femoral shaft is important to prevent impingement, improve knee kinematics, maximize ROM, and minimize flexion instability [1, 13–15, 17, 18]. Sex differences in distal femoral anatomy have been reported in several anatomic studies [5, 10, 12, 16]. Lonner et al. [12] found that the aspect ratio or ratio between the AP and mediolateral dimensions of the distal femur was larger in women than in men. This sexual dimorphism provided the theoretic basis for introduction and marketing of sex-specific knee implants. However, controversy exists regarding whether these sex differences are anthropomorphic or whether they are merely attributable to differences in relative femoral size. Li et al. [11] reported no sex differences in aspect ratio or total condylar height, and Fehring et al. [9] found no sex differences in the anatomy of the anterior condyles of the knee. Therefore, the question remains: Do we really need a sex-specific knee implant to restore normal anatomy?
To our knowledge, there are no studies that evaluate sex differences for posterior condylar offset of the knee. Additionally, traditional methods for measuring posterior condylar offset relied on perfect lateral plain radiographs or CT scans of the knee and did not take into account articular cartilage thickness or imperfections in radiographic technique. In contrast, three-dimensional (3-D) MRI can show articular cartilage and eliminate imprecisions related to magnification and obliquity, allowing for more accurate measurements. We previously developed a protocol to determine the posterior condylar offset of the medial and lateral femoral condyles using 3-D MRI reconstruction sequences designed to coordinate axial, coronal, and sagittal MR images [22].
Therefore, the purpose of our study was to determine if sex differences exist in (1) absolute posterior condylar offset size, (2) relative posterior condylar offset size with relation to total condylar height, and (3) posterior condylar articular cartilage thickness.
Patients and Methods
Before data collection, a power analysis was performed to determine the minimum number of patients needed for inclusion in the study to detect a minimum clinically important difference (MCID) in posterior condylar offset of 2 mm. We selected 2 mm as the MCID for posterior condylar offset since Bellemans et al. [2] reported that for every 2 mm decrease in posterior condylar offset after TKA, the maximal obtainable flexion was reduced by a mean of 12.2°. Since the MCID for knee ROM has been cited between 10° and 15° [13], we thought it was appropriate to select a posterior condylar offset MCID that corresponded to that difference in ROM. Additionally, because most TKA implant systems allow for up and down shifting of the femoral component by up to 2 mm for a given size, this value has clinical applicability. The a priori power calculation revealed that 17 patients were needed in each study group (men and women) to have 80% power to detect a 2 mm difference in posterior condylar offset. Given that we ultimately included 50 men and 50 women in our study, our power to detect a 2-mm difference in posterior condylar offset was 99.8%.
Using our institutional online searchable radiology database, we identified 142 patients (70 men and 72 women) who had knee MRI performed at our institution between March 2011 and February 2012. We selected only patients between 20 and 40 years old to minimize the likelihood of age-related degenerative joint disease in our study population. We excluded patients with a history of arthritis, deformity, dysplasia, osteochondral defect, fracture, or surgery about the knee; patient history was determined by examining office and inpatient progress notes, operative reports, and radiology reports. All MR images were ordered by primary care medical physicians for evaluation of nonspecific knee pain. After the exclusion process, we had a study population of 50 men and 50 women. Of the included patients, 57 had no knee disorder identified on MR images, 23 had isolated meniscus tears, 15 had partial medial collateral ligament tears, and five had partial or complete ACL tears. The mean height for included males was 69 inches (range, 64–75 inches; SD, 3 inches), and the mean height for included females was 65 inches (range, 61–71 inches; SD, 4 inches) (p value < 0.01). The mean BMI was similar between sexes: 23 kg/m2 for males (range, 15–34 kg/m2; SD, 4 kg/m2) and 24 kg/m2 for females (range, 14–35 kg/m2; SD, 5 kg/m2) (p value = 0.3). Of these 100 patients, 49 were Caucasian, 27 were African American, 16 were Asian, and eight were Hispanic.
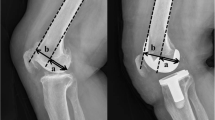
Our previously described 3-D protocol designed to coordinate axial, coronal, and sagittal MR images was used to make all measurements (Fig. 1) [22]. In brief, the technique was performed using multiplanar reformatted images created from isovoxel 3-D sampling perfection with application optimized contrasts using different flip angle evolutions (3-D SPACE) proton density-weighted fat-suppressed MRI sequences. Articular cartilage is clearly visible on these proton density sequences as it is intermediate in signal; the high-signal joint fluid and low-signal subchondral cortex provide excellent contrast [4]. A multiplanar viewing platform (iNtuition™ EMV [Enterprise Medical Viewer], TeraRecon, Inc, Foster City, CA, USA) was used to create default orthogonal axial, sagittal, and coronal planes. First, we identified the axial cut (Fig. 1), which showed the surgical transepicondylar axis of the femur (Fig. 1A, green line). Using the axial slice, we rotated the plane of the coronal images to be parallel to the transepicondylar axis and the plane of the sagittal images to be perpendicular to the transepicondylar axis (Fig. 1A, green line = coronal plane; blue line = sagittal plane). Using a single sagittal image through the center of the femoral shaft, the plane of the oblique images was angled to parallel the posterior cortex of the femoral shaft. In effect, this creates an oblique coronal plane that represents the posterior femoral cortex tangent line propagated medially and laterally along a line that parallels the transepicondylar axis. On sagittal images, the perpendicular distance between the position of this plane (Fig. 1B, red line) and the most posterior aspect of the medial femoral condyle (Fig. 1B, magenta line) was measured yielding the medial posterior condylar offset value. The same technique then was repeated for the lateral posterior condylar offset (Fig. 1C and D). Using the same sagittal images used to obtain the posterior condylar offset values, we measured total condylar height (defined as the total anterior-to-posterior dimension at the level of the posterior condylar offset at each femoral condyle, and articular cartilage thickness at the most posterior aspect of each femoral condyle. All measurements were performed by an orthopaedic surgery resident (PBV) using the aforementioned technique, which was developed by a radiologist with expertise in musculoskeletal radiology (JWS).
(A) A representative axial cut of a knee MR image shows the surgical transepicondylar axis of the femur (green line) and a line perpendicular to the transepicondylar axis intersecting the most posterior aspect of the medial femoral condyle (blue line). (B) A sagittal cross-section shows the medial posterior condylar offset (green line), which is the perpendicular distance between a line drawn along the posterior aspect of the femoral shaft (red line) and a parallel line intersecting the most posterior aspect of the medial femoral condyle (magenta line). (C) A representative axial cut of a knee MRI shows the surgical transepicondylar axis of the femur (green line) and a line perpendicular to the transepicondylar axis intersecting the most posterior aspect of the lateral femoral condyle (blue line). (D) A sagittal cross-section shows the lateral posterior condylar offset (light blue line), which is the perpendicular distance between a line drawn along the posterior aspect of the femoral shaft (dark blue line) and a parallel line intersecting the most posterior aspect of the medial femoral condyle (green line). (Published with kind permission from Springer Science+Business Media: Voleti PB, Stephenson JW, Lotke PA, Lee GC. Plain radiographs underestimate the asymmetry of the posterior condylar offset of the knee compared with MRI. Clin Orthop Relat Res. 2014;472:155–161.)
An isovoxel 3-D sequence such as the 3-D SPACE proton density-weighted fat-suppressed MRI sequences used in this study is unlike a traditional standard two-dimensional MR sequence. Similar to a helical CT data set, an isovoxel MR data series can be reformatted to any plane or obliquity of the operator’s choosing without losing image resolution or without gaps or stair-step artifact between adjacent voxels. As a result, these MR data sets allow us to prescribe an oblique sagittal plane that is realigned with respect to the anatomic axis of the femur. This correction means that the measurements generated are not affected by the initial acquisition plane or patient leg position as long as they are made on a single intact rigid structure (eg, the femur). In support of this notion, we identified two patients—one male and one female—who each had two MRI studies performed on the same knee at different times. For each patient, the center locus and leg position were slightly different between MRI studies. Nevertheless, our technique yielded identical posterior condylar offset measurements for both patients.
We compared the medial and lateral posterior condylar offset values obtained from male and female patients to evaluate for potential sex differences. We also compared the ratios of posterior condylar offset with the total condylar height at the medial and lateral femoral condyles to determine if any sex differences in posterior condylar offset size were proportional to femoral size. By selecting a fixed anatomic reference point, we sought to account for the contribution of femoral condyle size to the posterior condylar offset. Finally, we compared the thickness of the posterior condylar articular cartilage at both femoral condyles. All statistical comparisons were made using two-tailed, paired t-tests.
Results
Compared with females, males exhibited greater medial posterior condylar offset (30 mm [95% CI, 29.3–30.7 mm; SD, 2.5 mm] vs 28 mm [95% CI, 27.0–28.5 mm; SD, 2.7 mm] p < 0.001) and lateral posterior condylar offset (27 mm [95% CI, 26.2–27.3 mm; SD, 2.0 mm) vs 25 mm [95% CI, 24.2–25.4 mm; SD, 2.0 mm] p < 0.001]) (Table 1). Similarly, the total condylar height was greater in males than in females at the medial femoral condyle (63 mm [95% CI, 62.3–64.0 mm; SD, 3.2 mm] vs 57 mm [95% CI, 55.5–58.0 mm; SD, 4.4 mm], p < 0.001) and at the lateral femoral condyle (71 mm [95% CI, 69.2–72.1 mm; SD, 5.2 mm] vs 65 mm [95% CI, 63.6–65.8 mm; SD, 4.0 mm], p < 0.001) (Table 1).
The mean ratio of medial posterior condylar offset to medial condylar height was not different between males and females (0.48 [30 mm/63 mm] vs 0.49 [28 mm/57 mm]; odds ratio [OR], 0.96 [95% CI, 0.44–2.11; p = 0.08]) (Table 2). Similarly, the mean ratio of lateral posterior condylar offset to lateral condylar height was not different between sexes (0.38 [27 mm/71 mm] vs 0.38 [25 mm/65 mm]; OR, 1.00 [95% CI, 0.45–2.24; p = 0.8]) (Table 2).
There was no difference by sex in posterior condylar articular cartilage thickness at the medial femoral condyle (2.7 mm [SD, 0.5 mm] in males vs 2.5 mm [SD, 0.7 mm] in females; p = 0.1]) or at the lateral femoral condyle (2.6 mm [SD, 0.6 mm] in males vs 2.5 mm [SD, 0.8 mm] in females; p value = 0.5]) (Table 3). For all patients the mean thickness of the posterior condylar articular cartilage was 2.6 mm (SD, 0.7 mm) at the medial condyle and 2.5 mm (SD, 0.7 mm) at the lateral condyle.
Discussion
Despite improvements in surgical technique and prosthetic design during the past three decades, a physiologic TKA remains elusive [7, 8], and a substantial number of patients (approximately 20%) remain dissatisfied after knee replacement [3]. Although the threshold and clinical importance of failure to restore posterior condylar offset during TKA are incompletely defined, if the goal of the implant design is to reproduce normal anatomy and kinematics, then appropriate restoration of the normal posterior condylar offset may aid in optimal joint function. Controversy exists regarding whether there are true anthropomorphic differences between the distal femoral condyles of the male and female knee [5, 9–12, 16]; it remains unclear whether the articular surfaces and their relationships to the femur are consistent in males and females. Although some authors have described sex differences in distal femoral anatomy [5, 10, 12, 16], others have not found differences in the shape and position of the articular surface in the male and female knee [9, 11]. Therefore, the purpose of our study was to determine if sex differences exist in (1) absolute posterior condylar offset size, (2) relative posterior condylar offset size in relation to total condylar height, and (3) posterior condylar articular cartilage thickness.
This study has some limitations. First, our study population was relatively small and thus susceptible to sampling bias. Although our sample size easily exceeded the minimum number determined in our a priori power analysis, all imaging studies were obtained at one urban tertiary care medical center; thus, the bone-articular relationships observed in our study may not be widely generalized to all patient populations. Larger study populations are needed to further delineate the anthropomorphic differences in posterior condylar offset across the sexes and/or ethnicities. Our limited study population was underpowered to evaluate the contributions of ethnicity, height, age, and BMI on morphologic features of the knee. Second, we evaluated only nonarthritic knees, and therefore the results may not be fully applicable to severely arthritic knees requiring TKA. However, if the goal is to restore normal anatomy during TKA, then normal anatomy must be defined. Additional studies comparing nonarthritic and arthritic knees can further detail anatomic changes that occur because of joint degeneration. Third, our study population was not completely normal as all patients had knee pain. Nevertheless, the disorders observed on MR images (meniscus tears, medial collateral ligament tears, and ACL tears) are not expected to influence femoral anatomy or the size of the posterior condylar offset. Fourth, we used a nonvalidated method to normalize the posterior condylar offset in relation to the size of the knee. However, taking the ratio of posterior condylar offset to the total condylar height (both fixed anatomic points) is a mathematical maneuver that enables evaluation of the contribution of overall knee size to posterior condylar offset. Finally, our technique for measuring posterior condylar offset using MRI has not been validated using cadaveric studies. However, a cadaveric study has its own hurdles and complications. In this instance, a cadaveric validation study would require MRI studies on several cadaveric specimens and then splitting these femora perfectly in the sagittal planes corresponding to the maximum posterior condylar offsets at both condyles to measure the medial and lateral posterior condylar offset. Such a study would be technically difficult, cost prohibitive, and subject to inherent bias. The novel 3-D MRI technique we used has been shown to be accurate and reproducible as seen by the comparison of scans performed on the same patients at two different times. In each instance, measurements of posterior condylar offset, total condylar height, and articular cartilage thickness were identical.
Our results show that males have larger medial and lateral posterior condylar offset and total condylar height measurements compared with females. In short, knees in males are larger compared with knees in females, which is consistent with previous studies [9, 11]. Li et al. [11] found that the male femoral condyle was, on average, 12% to 13% larger than the female femoral condyle. Fehring et al. [9] also found that the total medial condylar height was larger in men compared with women. The differences were minimal (average, 1.1 mm), and there was variability in the sexes [9]. Thus, while male femoral condyles usually are larger compared with female femoral condyles, there can be a wide range of femoral sizes in a given sex. However, the question remains: Are there any proportional differences in the posterior femoral articulation between knees in males and females?
We found that while there are sex differences in posterior condylar offset and total condylar height at both femoral condyles, the ratio of medial posterior condylar offset to medial condylar height and the ratio of lateral posterior condylar offset to lateral condylar height were not different between sexes. Therefore, sex differences in posterior condylar offset size appear to be related to sex differences in femoral size, which means that the relationship of the posterior condylar articular surface to the posterior cortex of the femoral shaft was not different between males and females. These results are supported by other anatomic studies of human knees [6, 11, 21]. Li et al. [11] showed that while there were absolute size differences between knees in males and females, there was no sex difference in aspect ratios. Additionally, variations may exist in the human spectrum, regardless of sex or ethnicity. van den Heever et al. [21] attempted to classify distal femoral morphometric features using a neural network and reported that when corrected for size, sex and ethnic differences were diminished [21]. Finally, Chin et al. [6] observed in a group of Asian patients, that knees undergoing TKA showed sex variations in mediolateral dimensions, however, the AP dimensions of the condyles were similar between the sexes. The implication of these findings is that a sex-specific knee implant is not necessary to reproduce posterior condylar offset in women.
Finally, there were no sex differences in posterior condylar articular cartilage thickness. Therefore, the differences in posterior condylar offset size between the sexes cannot be accounted for by differences in cartilage thickness and simply are reflective of differences in femoral bone size. As a cohort, the mean thickness of the posterior condylar articular cartilage was 2.6 mm (± 0.7 mm) at the medial condyle and 2.5 mm (± 0.7 mm) at the lateral condyle. These findings are consistent with those of Thaunat and Beaufils [20], who mapped articular cartilage thickness of the posterior condyles in 15 cadaveric knees and reported that the mean cartilage thickness was 2.35 mm in the posteromedial condyle and 1.96 mm in the posterolateral femoral condyle. Given the consistency of the MRI measurements in our study with cadaveric measurements in their study, validation for the use of MRI as a measurement tool for articular cartilage thickness is provided. Tashiro et al. [19] showed that the articular cartilage thickness of the posterior condyles can affect rotational alignment in TKA. In their study, failure to account for articular cartilage of the posterior condyles led to excessive external rotation of the femoral components [19]. Consequently, instrumentation and prosthetic knee designs should be based on MRI rather than CT to provide the most accurate anatomic relationships.
Our study showed that there are no sex differences in the relative size of the posterior condylar offset at either the medial or the lateral femoral condyle. These results suggest that a unisex knee prosthesis design is sufficient to recreate the normal posterior condylar offset for men and women.
References
Arabori M, Matsui N, Kuroda R, Mizuno K, Doita M, Kurosaka M, Yoshiya S. Posterior condylar offset and flexion in posterior cruciate-retaining and posterior stabilized TKA. J Orthop Sci. 2008;13:46–50.
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty: influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63.
Braun HJ, Gold GE. Advanced MRI of articular cartilage. Imaging Med. 2011;3:541–555.
Chin KR, Dalury DF, Zurakowski D, Scott RD. Intraoperative measurements of male and female distal femurs during primary total knee arthroplasty. J Knee Surg. 2002;15:213–217.
Chin PL, Tey TT, Ibrahim MY, Chia SL, Yeo SJ, Lo NN. Intraoperative morphometric study of gender differences in Asian femurs. J Arthroplasty. 2011;26:984–988.
Deirmengian CA, Lonner JH. What’s new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2008;90:2556–2565.
Dennis DA, Komistek RD, Mahfouz MR. In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res. 2003;410;114–130.
Fehring TK, Odum SM, Hughes J, Springer BD, Beaver WB Jr. Differences between the sexes in the anatomy of the anterior condyle of the knee. J Bone Joint Surg Am. 2009;91:2335–2341.
Hitt K, Shurman JR 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85(suppl 4):115–122.
Li K, Langdale E, Tashman S, Harner C, Zhang X. Gender and condylar differences in distal femur morphometry clarified by automated computer analyses. J Orthop Res. 2012;30:686–692.
Lonner JH, Jasko JG, Thomas BS. Anthropomorphic differences between the distal femora of men and women. Clin Orthop Relat Res. 2008;466:2724–2729.
Malviya A, Lingard EA, Weir DJ, Deehan DJ. Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc. 2009;17:491–498.
Massin P, Gournay A. Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty. 2006;21:889–896.
Onodera T, Majima T, Nishiike O, Kasahara Y, Takahashi D. Posterior femoral condylar offset after total knee replacement in the risk of knee flexion contracture. J Arthroplasty. 2013;28:1112–1116.
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:35–46.
Seo SS, Ha DJ, Kim CW, Choi JS. Effect of posterior condylar offset on cruciate-retaining mobile TKA. Orthopedics. 2009;32(10 suppl):44–48.
Soda Y, Oishi J, Nakasa T, Nishikawa K, Ochi M. New parameter of flexion after posterior stabilized total knee arthroplasty: posterior condylar offset ratio on X-ray photographs. Arch Orthop Trauma Surg. 2007;127:167–170.
Tashiro Y, Uemura M, Matsuda S, Okazaki K, Kawahara S, Hashizume M, Iwamoto Y. Articular cartilage of the posterior condyle can affect rotational alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:1463–1469.
Thaunat M, Beaufils P. The posterior femoral condyles: a potential donor site for mosaic-like osteochondral autograft? Arthroscopy. 2010;26:1503–1509.
van den Heever DJ, Scheffer C, Erasmus P, Dillon E. Classification of gender and race in the distal femur using self organising maps. Knee. 2012;19:488–492.
Voleti PB, Stephenson JW, Lotke PA, Lee GC. Plain radiographs underestimate the asymmetry of the posterior condylar offset of the knee compared with MRI. Clin Orthop Relat Res. 2014;472:155–161.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery, University of Pennsylvania, Philadelphia, PA, USA.
About this article
Cite this article
Voleti, P.B., Stephenson, J.W., Lotke, P.A. et al. No Sex Differences Exist in Posterior Condylar Offsets of the Knee. Clin Orthop Relat Res 473, 1425–1431 (2015). https://doi.org/10.1007/s11999-014-4066-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-4066-z