Abstract
Background
As the number of primary total knee arthroplasties (TKAs) performed in the United States increases, policymakers have questioned whether the indications and timing of TKA have evolved so that surgery is offered earlier.
Questions/purposes
We analyzed data from a US national TKA cohort to evaluate variation in surgeon selection criteria for elective unilateral TKA based on preoperative patient-reported pain and function scores.
Methods
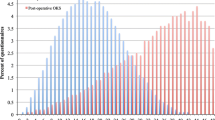
Preoperative SF-36 (Physical Component Summary [PCS]/physical function) scores and Knee Injury and Osteoarthritis Outcome Score (KOOS) (pain, activities of daily living/function) of 4900 patients undergoing elective unilateral TKA enrolled in this national database of prospectively followed patients from 22 states were evaluated. The 25th, 50th, and 75th percentile pain and function scores for patients cared for in 24 orthopaedic offices with 20 or more patients in the database were compared to assess whether consistent preoperative criteria are used in selecting patients undergoing TKA across settings.
Results
The preoperative global function (PCS median, 32.6; national norm, 50; SD, 10) and knee-specific function (KOOS median, 51.5; maximum score, 100; SD, 17) percentile scores represented substantial patient disability, because both values approached 2 SDs below ideal. Consistency in patients across 24 surgeon offices, and more than 100 surgeons, was noted because site-specific medians varied from the national median by less than the minimum clinically important change.
Conclusions
These data suggest that despite the rapidly growing use of TKA, surgeons in the participating sites use consistent patient criteria in scheduling TKA. Today’s patients report significant pain and disability, supporting the need for TKA.




Similar content being viewed by others
References
Ackerman IN, Dieppe PA, March LM, Roos EM, Nilsdotter A, Brown GC, Sloan KE, Osborne RH. Variation in age and physical status prior to total knee and hip replacement surgery: a comparison of centers in Australia and Europe. Arthritis Rheum. 2009;61:166–173.
Ayers DC, Zheng H, Franklin PD. Integrating patient-reported outcomes (PROs) into orthopaedic clinical practice: proof of concept from FORCE-TJR. Clin Orthop Relat Res. 2013;471:3419–3425.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;12:1833–1840.
Chernew M, Goldman D, Axeen S. How much savings can we wring from Medicare? N Engl J Med. 2011;365:e29.
Cobos R, Latorre A, Aizpuru F, Guenaga JI, Sarasqueta C, Escobar A, Garcia L, Herrera-Espineira C. Variability of indication criteria in knee and hip replacement: an observational study. BMC Musculoskelet Disord. 2010;11:249..
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236.
Cross WW 3rd, Saleh KJ, Wilt TJ, Kane RL. Agreement about indications for total knee arthroplasty. Clin Orthop Relat Res. 2006;446:34–39.
Dieppe P, Lim K, Lohmander S. Who should have knee joint replacement surgery for osteoarthritis? Int J Rheum Dis. 2011;14:175–180.
Felson DT, Chaisson CE. Understanding the relationship between body weight and osteoarthritis. Baillieres Clin Rheumatol. 1997;11:671–681.
Fortin PR, Penrod JR, Clarke AE, St-Pierre Y, Joseph L, Belisle P, Liang MH, Ferland,D, Phillips CB, Mahomed N, Tanzer M, Sledge C, Fossel AH, Katz JN. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46:3327–3330.
Franklin PD, Allison JJ, Ayers DC. Beyond joint implant registries: a patient-centered research consortium for comparative effectiveness in total joint replacement. JAMA. 2012;308:1217–1218.
Franklin PD, Harrold LR, Ayers DC. Incorporating patient reported outcomes in total joint arthroplasty registries: challenges and opportunities. Clin Orthop Relat Res. 2013;471:3482–3488.
Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: Functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466:2597–604.
Freund D, Lave J, Clancy C, Hawker G, Hasselblad V, Keller R, Schneiter E, Wright J. Patient outcomes research teams: contribution to outcomes and effectiveness research. Annu Rev Public Health. 1999:337–359.
Gossec L, Paternotte S, Bingham CO 3rd, Clegg DO, Coste P, Conaghan PG, Davis AM, Giacovelli G, Gunther KP, Hawker G, Hochberg MC, Jordan JM, Katz JN, Kloppenburg M, Lanzarotti A, Lim K, Lohmander LS, Mahomed NN, Maillefert JF, Manno RL, March LM, Mazzuca SA, Pavelka K, Punzi L, Roos EM, Rovati LC, Shi H, Singh JA, Suarez-Almazor ME, Tajana-Messi E, Dougados M. OARSI/OMERACT initiative to define states of severity and indication for joint replacement in hip and knee osteoarthritis. An OMERACT 10 special interest group. J Rheumatol. 2011;38:1765–1769.
HCUPnet. Healthcare Cost and Utilization Project (HCUP). Nationwide Inpatient Sample (NIS). Rockville, MD, USA: Agency for Healthcare Research and Quality; 2011. Available at: http://hcupnet.ahrq.gov/. Accessed October 11, 2013.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the united states from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Rankin EA, Alarcon GS, Chang RW, Cooney LM Jr, Costley LS, Delitto A, Dey RA, Donaldson SK, Hochberg MC, MacLean CH, Yelin EH, Marciel K. NIH consensus statement on total knee replacement, December 8–10, 2003. J Bone Joint Surg Am. 2004;86:1328–1335.
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96.
Ware JE, Kosinski M, Bjomer JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s Manual for the SF-36v2 Health Survey. 2nd ed. Lincoln, RI, USA: QualityMetric Incorporated; 2007.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483.
Woolf AD, Breedveld F, Kvien TK. Controlling the obesity epidemic is important for maintaining musculoskeletal health. Ann Rheum Dis. 2006;65:1401–1402.
Wright JG, Hawker GA, Bombardier C, Croxford R, Dittus RS, Freund DA, Coyte PC. Physician enthusiasm as an explanation for area variation in the utilization of knee replacement surgery. Med Care. 1999;37:946–956.
Acknowledgments
We gratefully acknowledge the more than 120 surgeons who participate in the FORCE-TJR national consortium, especially the core site Principal Investigators, Courtland Lewis MD, Philip Noble PhD, Regis O’Keefe MD, PhD, and Vincent Pellegrini MD. We also appreciate the editorial assistance of Sylvie Puig PhD.
Author information
Authors and Affiliations
Corresponding author
Additional information
During the study period, the authors’ institution has received funding from the Agency for Healthcare Research and Quality (Grant P50HS018910).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Ayers, D.C., Li, W., Harrold, L. et al. Preoperative Pain and Function Profiles Reflect Consistent TKA Patient Selection Among US Surgeons. Clin Orthop Relat Res 473, 76–81 (2015). https://doi.org/10.1007/s11999-014-3716-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3716-5