Abstract
Background
Key factors limiting patients with lower extremity amputations to achieve maximal functional capabilities are falls and fear of falling. A task-specific fall prevention training program has successfully reduced prospectively recorded trip-related falls that occur in the community by the elderly. However, this program has not been tested in amputees.
Questions/purposes
In a cohort of unilateral transtibial amputees, we aimed to assess effectiveness of a falls prevention training program by (1) quantifying improvements in trunk control; (2) measuring responses to a standardized perturbation; and (3) demonstrating retention at 3 and 6 months after training. Second, we collected patient-reported outcomes for balance confidence and falls control.
Methods
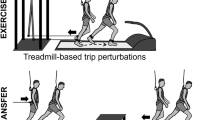
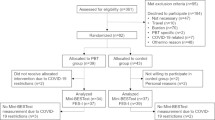
Fourteen male military service members (26 ± 3 years) with unilateral transtibial amputations and who had been walking without an assistive device for a median of 10 months (range, 2–106 months) were recruited to participate in this prospective cohort study. The training program used a microprocessor-controlled treadmill designed to deliver task-specific postural perturbations that simulated a trip. The training consisted of six 30-minute sessions delivered over a 2-week period, during which task difficulty, including perturbation magnitude, increased as the patient’s ability progressed. Training effectiveness was assessed using a perturbation test in an immersive virtual environment. The key outcome variables were peak trunk flexion and velocity, because trunk kinematics at the recovery step have been shown to be a determinant of fall likelihood. The patient-reported outcomes were also collected using questionnaires. The effectiveness of the rehabilitation program was also assessed by collecting data before perturbation training and comparing the key outcome parameters with those measured immediately after perturbation training (0 months) as well as both 3 and 6 months posttraining.
Results
Mean trunk flexion angle and velocity significantly improved after participating in the training program. The prosthetic limb trunk flexion angle improved from pretraining (42°; 95% confidence interval [CI], 38°–47°) to after training (31°; 95% CI, 25°–37°; p < 0.001). Likewise, the trunk flexion velocity improved from pretraining (187°/sec; 95% CI, 166°–209°) to after training (143°/sec; 95% CI, 119°–167°; p < 0.004). The results display a significant side-to-side difference for peak trunk flexion angle (p = 0.01) with perturbations of the prosthetic limb resulting in higher peak angles. Prosthetic limb trips also exhibited significantly greater peak trunk flexion velocity compared with trips of the prosthetic limb (p = 0.005). These changes were maintained up to 6 months after the training. The peak trunk flexion angle of the subjects when the prosthetic limb was perturbed had a mean of 31° (95% CI, 25°–37°) at 0 month, 32° (95% CI, 28°–37°) at 3 months, and 30° (95% CI, 25°–34°) at 6 months. Likewise, the peak trunk flexion velocity for the prosthetic limb was a mean of 143°/sec (95% CI, 118°–167°) at 0 months, 143°/sec (95% CI, 126°–159°) at 3 months, and 132° (95% CI, 115°–149°) at 6 months. The peak trunk flexion angle when the nonprosthetic limb was perturbed had a mean of 22° (95% CI, 18°–24°) at 0 months, a mean of 26° (95% CI, 20°–32°) at 3 months, and a mean of 23° (95% CI, 19°–28°) at 6 months. The peak trunk flexion velocity for the nonprosthetic limb had a mean of 85°/sec (95% CI, 71°–98°) at 0 months, a mean of 96° (95% CI, 68°–124°) at 3 months, and 87°/sec (95% CI, 68°–105°) at 6 months. There were no significant changes in the peak trunk flexion angle (p = 0.16) or peak trunk flexion velocity (p = 0.35) over time after the training ended. The skill retention was present when either the prosthetic or nonprosthetic limb was perturbed. There were side-to-side differences in the trunk flexion angle (p = 0.038) and trunk flexion velocity (p = 0.004). Perturbations of the prosthetic side resulted in larger trunk flexion and higher trunk flexion velocities. Subjects prospectively reported decreased stumbles, semicontrolled falls, and uncontrolled falls.
Conclusions
These results indicate that task-specific fall prevention training is an effective rehabilitation method to reduce falls in persons with lower extremity transtibial amputations.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.




Similar content being viewed by others
References
Alexander RM. Optimization and gaits in the locomotion of vertebrates. Physiol Rev. 1989;69:1199–1227.
Andersen R, Davis S, Scoville C. Rehabilitation of military amputees: from injury to independence. Orthopedics. 2008;31:100–1002.
Berg WP, Alessio HM, MIlls EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26:261–268.
Bieryla KA, Madigan ML, Nussbaum MA. Practicing recovery from a simulated trip improves recovery kinematics after an actual trip. Gait Posture. 2007;26:208–213.
Crenshaw JR, Kaufman KR, Grabiner MD. Trip recoveries of people with unilateral transfemoral and knee disarticulation amputations. Gait Posture. 2013;38:500–506.
Crenshaw JR, Rosenblatt NJ, Hurt CP, Grabiner MD. The discriminant capabilities of stability measures, trunk kinematics, and step kinematics in classifying successful and failed compensatory stepping responses by young adults. J Biomech. 2012;45:129–133.
Dite W, Connor HJ, Curtis HC. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch Phys Med Rehabil. 2007;88:109–114.
Franchignoni F, Orlandini D, Ferriero G, Moscato TA. Reliability, validity, and responsiveness of the locomotor capabilities index in adults with lower-limb amputation undergoing prosthetic training. Arch Phys Med Rehabil. 2004;85:743–748.
Geurts ACH, Mulder TW, Nienhuis B, Rijken RA. Postural reorganization following lower limb amputation. Possible motor and sensory determinants of recovery. Scand J Rehabil Med. 1992;24:83–90.
Gooday HM, Hunter J. Preventing falls and stump injuries in lower limb amputees during inpatient rehabilitation: completion of the audit cycle. Clin Rehabil. 2004;18:379–390.
Grabiner MD, Bareither ML, Gatts S, Marone J, Troy KL. Task-specific training reduces trip-related fall risk in women. Med Sci Sports Exerc. 2012;44:2410–2414.
Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil. 2007;88:207–217.
Hall CD, Jensen JL. Age-related differences in lower extremity power after support surface perturbations. J Am Geriatr Soc. 2002;50:1782–1788.
Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056.
Henry FM. Specificity versus Generality in Learing Motor Skills. Englewood Cliffs, NJ, USA: Prentice Hall; 1968.
Hermodsson Y, Ekdahl C, Persson BM, Roxendal G. Standing balance in trans-tibial amputees following vascular disease or trauma: a comparative study with healthy subjects. Prosthet Orthot Int. 1994;18:150–158.
Holliday PJ, Fernie G, Gryfe CI, Griggs GT. Video recording of spontaneous falls of the elderly. In: ASTM STP 1103. Slips, Stumbles, and Falls: Pedestrian Foorwear and Surfaces. Philadelphia, PA, USA: American Society for Testing and Materials; 1990:7–16.
Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, Jette A. Covariates of fear of falling and associated activity curtailment. Gerontologist. 1998;38:549–555.
Kadaba M, Ramakrishnan H, Wootten M. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392.
Kavounoudias A, Tremblay C, Gravel D, Iancu A, Forget R. Bilateral changes in somatosensory sensibility after unilateral below-knee amputation. Arch Phys Med Rehabil. 2005;86:633–640.
Knapp B. Skill in Sport–the Attainment of Proficiency. London, UK: Routledge & Kegan Paul PLC; 1963.
Liao KI, Skinner HB. Knee joint proprioception in below-knee amputees. Am J Knee Surg. 1995;8:105–109.
Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991;46:M123–131.
Mansfield A, Maki BE. Are age-related impairments in change-in-support balance reactions dependent on the method of balance perturbation? J Biomech. 2009;42:1023–1031.
Memmert D. Long-term effects of type of practice on the learning and transfer of a complex motor skill. Percept Mot Skills. 2006;103:912–916.
Mille ML, Rogers MW, Martinez K, Hedman LD, Johnson ME, Lord SR, Fitzpatrick RC. Thresholds for inducing protective stepping responses to external perturbations of human standing. J Neurophysiol. 2003;90:666–674.
Miller WC, Deathe AB, Speechley M. Psychometric properties of the Activities-Specific Balance Confidence Scale among individuals with a lower limb amputation. Arch Phys Med Rehabil. 2003;84:656–661.
Miller WC, Deathe AB, Speechley M, Koval J. The influence of falling, fear of falling, and balance confidence on prosthetic mobility and social activity among individuals with a lower extremity amputation. Arch Phys Med Rehabil. 2001;82:1238–1244.
Miller WC, Speechley M, Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch Phys Med Rehabil. 2001;82:1031–1037.
Miller WC, Speechley M, Deathe AB. Balance confidence among people with lower-limb amputations. Phys Ther. 2002;82:856–865.
Ovens A, Smith W. Skill: making sense of a complex concept. Journal of Physical Education New Zealand. 2006;39:72–82.
Owings TM, Pavol MJ, Grabiner MD. Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin Biomech. 2001;16:813–819.
Pai YC, Rogers MW, Patton J, Cain TD, Hanke TA. Static versus dynamic predictions of protective stepping following waist-pull perturbations in young and older adults. J Biomech. 1998;31:1111–1118.
Pauley T, Devlin M, Heslin K. Falls sustained during inpatient rehabilitation after lower limb amputation: prevalence and predictors. Am J Phys Med Rehabil. 2006;85:521–532; quiz 533–535.
Pavol MJ, Owings TM, Foley KT, Grabiner MD. Mechanisms leading to a fall from an induced trip in healthy older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M428–437.
Potter BK, Scoville CR. Amputation is not isolated: an overview of the US Army Amputee Patient Care Program and associated amputee injuries. J Am Acad Orthop Surg. 2006;14:S188–S190.
Powell LE, Myers AM. The Activities-Specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–34.
Quai TM, Brauer SG, Nitz JC. Somatosensation, circulation and stance balance in elderly dysvascular transtibial amputees. Clin Rehabil. 2005;19:668–676.
Rogers MW, Hedman LD, Johnson ME, Cain TD, Hanke TA. Lateral stability during forward-induced stepping for dynamic balance recovery in young and older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M589–594.
Rosenblatt N, Marone J, Grabiner MD. Task-specific trainning decreases falls by older women in the community: 6 month prospective data. Gerontologist. 2010;50:412.
Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: a prospective study. J Am Geriatr Soc. 2013;61:1629–1631.
Savion-Lemieux T, Penhune VB. The effects of practice and delay on motor skill learning and retention. Exp Brain Res. 2005;161:423–431.
Schulz BW, Ashton-Miller JA, Alexander NB. Compensatory stepping in response to waist pulls in balance-impaired and unimpaired women. Gait Posture. 2005;22:198–209.
Sessoms PH, Wyatt M, Grabiner MD, Collins JD, Kingsbury T, Thesing N, Kaufman K. Method for evoking a trip-like response using a treadmill-based perturbation during locomotion. J Biomech. 2014;47:277–280.
Shadmehr R, Brashers-Krug T. Functional stages in the formation of human long-term motor memory. J Neurosci. 1997;17:409–419.
Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehabil. 2004;83:493–499.
Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 1998;53:M112–119.
Troy KL, Donovan SJ, Marone JR, Bareither ML, Grabiner MD. Modifiable performance domain risk-factors associated with slip-related falls. Gait Posture. 2008;28:461–465.
Van Velzen JM, Van Bennekom CAM, Polomski W, Slootman JR, Van Der Woude VHL, Houdijk H. Physical capacity of walking ability after lower limb amputation: a systematic review. Clin Rehabil. 2006;20:999–1016.
Vellas BJ, Rubenstein LZ, Ousset PJ, Faisant C, Kostek V, Nourhashemi F, Allard M, Albarede JL. One-leg standing balance and functional status in a population of 512 community-living elderly persons. Aging (Milano). 1997;9:95–98.
Acknowledgments
We thank Jordan Sturdy, Trevor Kingsbury, Nancy Thesing, Katie Sharp, John-David Collins, Mandy Wong, Grant Myers, and Birgit Unfried for contributing to this research project.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by the Department of Defense Grant Number W81X-WH-11-2-0058 (Log No. DM090896) and the Navy Bureau of Medicine and Surgery, Wounded, Ill, and Injured Program. Approved for public release; distribution is unlimited. This research was conducted in compliance with all applicable federal regulations governing the protection of human subjects (protocol NMCSD.2001.003 and Protocol NHRC.2001.0031). The institution of one or more of the authors (MDG) has a patent on technology (ActiveStep™; Symbex, Lebanon, NH, USA) noted in this manuscript. One of the authors (MDG) is an inventor of the ActiveStep™ system but has no conflicts of interest to declare with regard to the present study.
The views expressed are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Patients were recruited from the Comprehensive Combat & Complex Casualty Care (C5) program at the Naval Medical Center San Diego, San Diego, CA, USA.
About this article
Cite this article
Kaufman, K.R., Wyatt, M.P., Sessoms, P.H. et al. Task-specific Fall Prevention Training Is Effective for Warfighters With Transtibial Amputations. Clin Orthop Relat Res 472, 3076–3084 (2014). https://doi.org/10.1007/s11999-014-3664-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3664-0