Abstract
Background
Multiple mechanical factors affecting the hip have been associated with the development of slipped capital femoral epiphysis (SCFE). Whether acetabular depth plays a role in the development of a SCFE has not been elucidated.
Questions/purposes
(1) What is the prevalence of a deep acetabulum in SCFE? (2) Is the presence of a deep acetabulum associated with physeal instability? (3) Is the presence of a deep acetabulum associated with the occurrence of a contralateral SCFE?
Methods
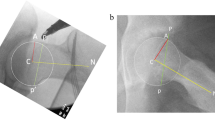
We retrospectively reviewed 232 patients (156 males) who presented with a unilateral SCFE. Fifty (22%) subsequently developed a contralateral SCFE. The involved and uninvolved sides were evaluated for the presence of a deep acetabulum (DA). Preoperative radiographic parameters, slip stability, development of a contralateral SCFE, and demographic factors were then compared between patients with and without DA.
Results
DA was present in 120 hips (52%) with a SCFE. DA was more common in females (55 of 76 [72%]) than males (65 of 156 [42%]). Patients with DA presented with a higher lateral center-edge angle (33° versus 31°), slip angle (52° versus 43°), and with a lower body mass index (28.1 versus 30.0 kg/m2). Increased acetabular depth was more common in patients with an unstable SCFE (29 of 41 [71%]) than those with a stable SCFE (91 of 191 [48%]). The presence of DA either on the affected side or the contralateral side did not predict a contralateral SCFE.
Conclusions
Despite not predicting a contralateral SCFE, DA may influence physeal stability if a SCFE does develop. Therefore, the contralateral hip with DA should be closely monitored.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.

Similar content being viewed by others
References
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018.
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73.
Bhatia NN, Pirpiris M, Otsuka NY. Body mass index in patients with slipped capital femoral epiphysis. J Pediatr Orthop. 2006;26:197–199.
Chung SM, Batterman SC, Brighton CT. Shear strength of the human femoral capital epiphyseal plate. J Bone Joint Surg Am. 1976;58:94–103.
Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66.
Crowninshield RD, Brand RA, Pedersen DR. A stress analysis of acetabular reconstruction in protrusio acetabuli. J Bone Joint Surg Am. 1983;65:495–499.
Gelberman RH, Cohen MS, Shaw BA, Kasser JR, Griffin PP, Wilkinson RH. The association of femoral retroversion with slipped capital femoral epiphysis. J Bone Joint Surg Am. 1986;68:1000–1007.
Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162–1169.
Gusis SE, Babini JC, Garay SM, Garcia Morteo O, Maldonado Cocco JA. Evaluation of the measurement methods for protrusio acetabuli in normal children. Skeletal Radiol. 1990;19:279–282.
Hagglund G, Hansson LI, Ordeberg G, Sandstrom S. Bilaterality in slipped upper femoral epiphysis. J Bone Joint Surg Br. 1988;70:179–181.
Hastings DE, Parker SM. Protrusio acetabuli in rheumatoid arthritis. Clin Orthop Relat Res. 1975;108:76–83.
Kallio PE, Mah ET, Foster BK, Paterson DC, LeQuesne GW. Slipped capital femoral epiphysis. Incidence and clinical assessment of physeal instability. J Bone Joint Surg Br. 1995;77:752–755.
Kennedy JG, Hresko MT, Kasser JR, Shrock KB, Zurakowski D, Waters PM, Millis MB. Osteonecrosis of the femoral head associated with slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21:189–193.
Kitadai HK, Milani C, Nery CA, Filho JL. Wiberg’s center-edge angle in patients with slipped capital femoral epiphysis. J Pediatr Orthop. 1999;19:97–105.
Kordelle J, Richolt JA, Millis M, Jolesz FA, Kikinis R. Development of the acetabulum in patients with slipped capital femoral epiphysis: a three-dimensional analysis based on computed tomography. J Pediatr Orthop. 2001;21:174–178.
Leunig M, Nho SJ, Turchetto L, Ganz R. Protrusio acetabuli: new insights and experience with joint preservation. Clin Orthop Relat Res. 2009;467:2241–2250.
Loder RT, Aronson DD, Greenfield ML. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am. 1993;75:1141–1147.
Loder RT, Hensinger RN. Slipped capital femoral epiphysis associated with renal failure osteodystrophy. J Pediatr Orthop. 1997;17:205–211.
Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75:1134–1140.
Loder RT, Wittenberg B, DeSilva G. Slipped capital femoral epiphysis associated with endocrine disorders. J Pediatr Orthop. 1995;15:349–356.
Manoff EM, Banffy MB, Winell JJ. Relationship between body mass index and slipped capital femoral epiphysis. J Pediatr Orthop. 2005;25:744–746.
Maquet P. Biomechanics of the Hip. Berlin, Germany: Springer; 1985.
Mirkopulos N, Weiner DS, Askew M. The evolving slope of the proximal femoral growth plate relationship to slipped capital femoral epiphysis. J Pediatr Orthop. 1988;8:268–273.
Park S, Hsu JE, Rendon N, Wolfgruber H, Wells L. Predicting a contralateral slip after unilateral slipped capital femoral epiphysis: is the posterior sloping angle useful? UPOJ. 2010;20:106–112.
Poussa M, Schlenzka D, Yrjonen T. Body mass index and slipped capital femoral epiphysis. J Pediatr Orthop B. 2003;12:369–371.
Rattey T, Piehl F, Wright JG. Acute slipped capital femoral epiphysis. Review of outcomes and rates of avascular necrosis. J Bone Joint Surg Am. 1996;78:398–402.
Sankar WN, Brighton BK, Kim Y-J, Millis MB. Acetabular morphology in slipped capital femoral epiphysis. J Pediatr Orthop. 2011;31:254–258.
Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49:807–835.
Stanitski CL, Woo R, Stanitski DF. Femoral version in acute slipped capital femoral epiphysis. J Pediatr Orthop B. 1996;5:74–76.
Steel HH. Protrusio acetabuli: its occurrence in the completely expressed Marfan syndrome and its musculoskeletal component and a procedure to arrest the course of protrusion in the growing pelvis. J Pediatr Orthop. 1996;16:704–718.
Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466:273–280.
Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552.
Wenger DR, Ditkoff TJ, Herring JA, Mauldin DM. Protrusio acetabuli in Marfan’s syndrome. Clin Orthop Relat Res. 1980;147:134–138.
Wiberg G. Studies in dysplastic acetabulum and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83:S58.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Texas Scottish Rite Hospital for Children, Dallas, TX, USA.
About this article
Cite this article
Podeszwa, D.A., Gurd, D., Riccio, A. et al. Increased Acetabular Depth May Influence Physeal Stability in Slipped Capital Femoral Epiphysis. Clin Orthop Relat Res 471, 2151–2155 (2013). https://doi.org/10.1007/s11999-013-2807-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-2807-z