Abstract
Background
Studies have demonstrated sex differences in femoral shape and quadriceps angle raising a question of whether implant design should be sex-specific. Much of this research has addressed shape differences within the Caucasian population and little is known about differences among ethnic groups.
Questions/purposes
We therefore asked: Do shape differences in the distal femur and proximal tibia exist among different ethnic groups and between the sexes in each ethnic population? And if ethnic differences exist, do they have a clinical impact on current TKA design?
Subjects and Methods
We analyzed 1000 normal adult knees (80 African American, 80 East Asian, and 860 Caucasian). Three-dimensional surface models were created for each bone and added to three-dimensional statistical bone atlases. Statistical shape analysis was conducted with a process combining principal components and multiple discriminate analyses. Eleven femoral and nine tibial measurements were calculated.
Results
We found differences in mean measurements between the sexes and ethnicities. Males had larger knees, with a mean 5-mm-larger anteroposterior dimension than females in all ethnicities. African American females had a 7.4-mm-deeper patellar groove, 2.3-mm-smaller tibial mediolateral dimension, and 2.5-mm-larger tibial anteroposterior dimension than Caucasian females. African American males had a 4.3-mm-larger femoral anteroposterior dimension, 10.1-mm-larger tibial mediolateral dimension, and 6-mm-larger tibial anteroposterior dimension than Asian males.
Conclusions
We identified differences in three-dimensional knee morphology among Caucasian, African American, and East Asian populations. Clinical studies will be required to determine whether these differences are important for implant design.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, many studies have identified shape differences in the knee within the Caucasian population [2, 6, 10]. Shape analyses have identified sex differences in the femoral midshaft, distal femur, and patella [7, 15, 24]. Using automated three-dimensional (3D) morphologic analysis, differences in knee morphology between the sexes has been identified [17, 18]. Differences among European Caucasian males and females have been reported, with females having a smaller mediolateral to anteroposterior ratio and more narrow distal femurs; however, the study suggested morphotype in addition to sex contributed to the distal femur and proximal tibia geometry [2].
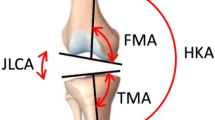
Ethnic differences have not received much focus given that most existing TKA implant designs are based on the Caucasian population. Many studies have reported the anatomy and comparison of East Asian populations (Japanese, Chinese, Indian) to existing implant systems [3, 4, 10, 11, 21–23, 26]. Anatomic differences have been identified between both sex and ethnicity, with Caucasian subjects having a higher tibial torsion angle and lower varus alignment than Japanese [12]. Also, females had smaller medial and lateral tibial widths and higher valgus alignment. General size differences have been reported between Chinese and Caucasian knees, with Chinese knees having smaller mediolateral and anteroposterior femoral measurements, tibial measurements, and femoral and tibial aspect ratios, suggesting existing femoral implant designs may not properly accommodate the East Asian population [27]. However, most of these studies focusing on Asians lacked true 3D measurements [20]. Images captured by two-dimensional (2D) methods, such as radiography, provide only a projection of bone shape and do not provide a complete picture of the patient’s anatomy. Anatomic landmarks can often be hidden from view and manual measurements calculated using such images can contain interobserver error. Measurements from radiographs are also prone to errors generated from the misalignment of the knee relative to the imaging plane. A 3D analysis can eliminate this error by automatically calculating these measurements in 3D space, more accurately reflecting a person’s true anatomy.
We therefore asked: (1) Do shape differences in the distal femur and proximal tibia exist among different ethnic groups? (2) Do shape differences in the distal femur and proximal tibia exist between the sexes in each ethnic population? And (3) if ethnical differences in the shape and size of the distal femur and proximal tibia exist, do they have a clinical impact on current TKA design?
Subjects and Methods
We analyzed 1000 adult knees (840 Caucasians [500 male (CM), 340 female (CF)], 80 African Americans [40 male (AAM), 40 female (AAF)], 80 East Asians [40 male (AM), 40 female (AF)]). All Caucasians were of European descent. CT datasets were obtained through either the William M. Bass Donated Skeletal Collection in the Department of Anthropology or cadaver scans in the Center for Musculoskeletal Research, both at the University of Tennessee, and MRI datasets were obtained through The Osteoarthritis Initiative. We included only normal, nonpathologic bones in this analysis and specifically excluded those with any abnormalities. MRI scans for the 34 AAFs and the 80 East Asians were obtained with 0.36- × 0.36- × 0.69-mm cubic voxels. In addition, 886 CT datasets (840 Caucasians, 40 AAMs, six AAFs) were acquired with 0.625- × 0.625- × 0.625-mm cubic voxels. DICOM images for both CT and MRI were manually segmented and surface models were generated. This segmentation process has been proven reliable with an interobserver error of 0.163 mm, intraobserver error of 0.105 mm, and pairwise interobserver variability of 0.269 mm [18].
Segmented models for each femur and tibia were added to the bone atlas [18] (Fig. 1). Briefly, a bone atlas is an average model that captures the primary shape variation of a bone and allows for the comparison of global shape differences between groups or populations, guaranteeing standardization, normalization, and landmark correspondence across a population. Twelve separate statistical atlases of femora and tibiae were generated for Caucasians, African Americans, and East Asians divided into male and female.
To fully identify shape differences among ethnicities, a two-step feature extraction methodology was implemented (Fig. 2). The first step identified global shape differences between the sexes in each ethnicity and between the sexes across all ethnicities. This method utilized principle component analysis [13], a mathematical tool that reduces the dimensionality of variables while maintaining most of the variance of the original data, both as a means of variable reduction and as a global shape descriptor. This method finds points of high discrimination between different sex and ethnic groups when normalized against the first principal component, which is considered primarily scale, highlighting areas that would be highly discriminating without the use of any other information. This algorithm was used to examine shape differences independent of size differences between the sexes and among the three ethnicity populations. The second step utilized anatomic and surgical landmarks to automatically calculate linear measurements, angular measurements, and curvature once each bone was added to the atlas.
Three-dimensional landmarks were automatically calculated on each bone [18]. Landmarks sometimes falling between CT slices can be miscalculated in 2D analyses. Utilizing a 3D approach ensures all landmarks are anatomically accurate in three dimensions (Fig. 3). Using these landmarks, a set of linear and angular measurements was calculated on the distal femur (Fig. 4) and proximal tibia (Fig. 5). In total, 11 femoral (Table 1) and nine tibial (Table 2) measurements were recorded.
An example shows the advantage of our 3D method when calculating the transepicondylar axis. (A) A volume rendering of the knee shows the transepicondylar axis passing through a series of points collected on the epicondyles. (B) An image shows the automatically calculated transepicondylar axis and a sample image slice to demonstrate the axis does not lie in one CT slice; thus, localizing directly on the CT image will produce rotational error.
A diagram illustrates measurements on the distal femur. TEA = transepicondylar axis length; APH = anteroposterior height; MAP = medial anteroposterior height; LAP = lateral anteroposterior height; AP_AD = anteroposterior angle difference; AML = anterior mediolateral length; PML = posterior mediolateral length; DML = distal mediolateral length.
A diagram illustrates measurements on the proximal tibia. ML = mediolateral width; AP = anteroposterior height; EM_W = eminence width; TEVA = tuberosity eminence vector angle; LPW = lateral plateau mediolateral width; LPH = lateral plateau anteroposterior height; MPW = medial plateau mediolateral width; MPH = medial plateau anteroposterior height.
Using the above measurements, three normalized ratios that best describe femoral shape were calculated: mediolateral width/anteroposterior height (ML/AP), anterior mediolateral length/posterior mediolateral length (AML/PML), and medial anteroposterior height/lateral anteroposterior height (MAP/LAP). These ratios were used to classify and describe the shapes of femora: Type I and II with regard to ML/AP, Type III and IV based on AML/PML, and Type V and VI based on LAP/MAP (Fig. 6). Type I femurs are more square in shape with a ML/AP closer to 1 whereas Type II femurs have a higher ratio and are more rectangular in shape. Type III femurs are more triangular with a smaller AML/PML ratio whereas Type IV femurs are more rectangular. A smaller MAP/LAP ratio implies a lesser angle between the anterior and posterior condylar axes, indicating a Type V femur, whereas the anterior and posterior condylar axes are more parallel to one another in Type VI femurs. Three ratios were also calculated on the tibia: ML/AP, lateral plateau width/lateral plateau height (LPW/LPH), and medial plateau width/medial plateau height (MPW/MPH).
A diagram illustrates the six classifications used to describe femoral shape based on three normalized ratios. Type I and Type II classify femoral shape relative to mediolateral width/anteroposterior height (ML/AP), Type III and Type IV classify femoral shape relative to anterior mediolateral length/posterior mediolateral length (AML/PML), and Type V and Type VI classify femoral shape relative to medial anteroposterior height/lateral anteroposterior height (MAP/LAP).
Curvature of the femoral condyle and tibial plateau are integral in dictating normal knee motion as curvature of the lateral and medial condyles is one of the main factors affecting knee kinematics. In general, a more curved knee has a higher ROM. To accurately map, and therefore analyze, the femoral condyle curvature, three profiles were used to approximate the most prominent contact points on both the medial and lateral sides and the patellar groove. The medial profile was calculated by defining a plane that passes through the most anterior, distal, and posterior points on the medial condyle. This plane was then intersected with the distal femur and the resulting contour was resampled into 50 equidistance points. This profile contour represented the most protruding points on the medial condyle surface. Similarly, the same method was used to calculate the lateral profile. To accurately calculate the curvature of the sulcus, a set of contours were extracted by intersecting the distal femur with a series of planes rotating around the transepicondylar axis in 10° increments. The lowest points on these contours were then used to define the sulcus points (Fig. 7). To quantify curvature of the medial and lateral condyles and sulcus profiles, an iterative least-square algorithm was developed to break down each curve into a number of radii of curvature that best approximated that curve.
Differences in the sex and ethnic group means of femoral measurements, femoral curvature, and tibia measurements were tested by one-way ANOVA and t test. Due to the imbalanced sample size, two versions of the t test for both equal and unequal variance were utilized. Hypothesis of equal variance was tested using f test. The power test was used to calculate the minimum sample size required to test the null hypothesis of two populations from different means. Discriminate analysis, a means of determining discrimination between two or more groups, was used along with principal component analysis to rank bone surfaces using statistics captured from populations using IDAS software [16]. ANOVA, t test, f test, and power test calculations were completed using MATLAB® (The MathWorks, Inc, Natick, MA, USA).
Results
Shape differences among the ethnic groups were identified in the distal femur (Table 3) and proximal tibia (Table 4). On examining femoral differences among ethnicities, medial and lateral curves for African Americans and Caucasians were best approximated using four radii of curvature, C1 to C4, whereas East Asians were best approximated using three, C1 to C3 (Fig. 8). AAMs and AAFs had larger (p < 0.01) AP dimensions than their Asian and Caucasian counterparts and AMs and AFs had smaller (p < 0.01) AP dimensions than CMs and CFs. When compared to CFs with similar AP dimensions, AMs had larger (p < 0.01) ML dimensions. In analyzing ethnic differences in tibial anatomy, AAMs had larger (p < 0.01) LAPs and smaller MPHs than CMs, while also having larger (p < 0.01) ML and AP dimensions than AMs. AMs and AFs had smaller (p < 0.01) ML and AP dimensions than CMs and CFs. Figure 9 outlines areas of high (red) and low (blue) morphologic differences in both the femur and tibia captured by the second to ninth principal components among sex and ethnicity. These femoral linear (Table 5), femoral curvature (Table 6), and tibial (Table 7) differences were highlighted in the t tests and power tests based on the automated measurements. Several of these measurements directly correlated to some of the shape differences found in the femur and tibia (Fig. 10).
Images illustrate the comparison of high (red) and low (blue) global shape differences among sex and ethnicity groups captured by the second to ninth principal components. AM = East Asian male; AF = East Asian female; CM = Caucasian male; CF = Caucasian female; AAM = African American male; AAF = African American female.
Images illustrate the correlation between global shape analysis using principal component analysis and geodesic measurements. TEA = transepicondylar axis length; APH = anteroposterior height; MAP = medial anteroposterior height; LAP = lateral anteroposterior height; AP_AD = anteroposterior angle difference; AML = anterior mediolateral length; PML = posterior mediolateral length; DML = distal mediolateral length.
Shape differences in the distal femur and proximal tibia were identified between sexes in each ethnic population. Males across all ethnicities had average 9-mm larger (p < 0.01) ML and 5-mm larger (p < 0.01) AP dimensions than their female counterparts. AAMs and CFs had shallower (p < 0.01) patellar grooves than AAFs and CMs. Females had more curved (p < 0.01) femurs in all ethnicities. Males had larger (p < 0.01) tibial AP dimensions than females. AAMs and CMs had larger (p < 0.01) ML dimensions than AAFs and CFs, respectively. Differences in femoral (Table 8) and tibial (Table 9) shapes were identified in comparing shapes across populations based on differences in ML/AP, AML/PML, and MAP/LAP ratios.
The morphologic differences identified among the ethnicities in this study indicated notable clinical implications on existing TKA design. For example, the AP of AMs (54.9 ± 4.4 mm) was similar to that of CFs (55.9 ± 3.3 mm), which could lead to the wrongful assumption of using sex-specific implants for AMs. However, a closer look reveals substantial ML and ML/AP ratio differences between these two groups, which could lead to underhang when using such implants for AMs. When comparing datasets with the same AP (57.4 mm), we found AMs (ML = 85.6 mm) had a 6-mm-larger ML than CFs (ML = 80 mm). Likewise, another comparison of datasets (AP = 49.7 mm) showed AMs (77 mm) had a 6-mm-larger ML than comparable CFs (ML = 71 mm).
Discussion
Ethnic differences have not received much focus given that most research has been aimed at the investigation of shape differences within the Caucasian population [2–4, 6, 10, 11, 17, 21–23]; however, previous studies have reported the anatomy and comparison of East Asian populations (Japanese, Chinese, Indian) to existing implant systems [3, 4, 10, 11, 21–23, 26]. We therefore asked: (1) Do shape differences in the distal femur and proximal tibia exist among different ethnic groups? (2) Do shape differences in the distal femur and proximal tibia exist between the sexes in each ethnic population? And (3) if ethnic differences in the shape and size of the distal femur and proximal tibia exist, do they have a clinical impact on current TKA design?
There are a number of limitations to our study. First, while we found statistically significant differences in the size and morphology of the distal femur and proximal tibia in sex and ethnicity, further investigation is required to closer examine any clinical impact of each of these differences. While a direct comparison of the absolute and average values revealed a difference of a few millimeters, it is the analysis of different aspect ratios that has clinical relevance with a combined impact on both shape and size. Second, our Caucasian population was much larger than the African American and East Asian (consisting mainly of Chinese, Korean, and a few Japanese subjects) populations and thus we utilized two versions of the t test for both equal and unequal variance. Third, we did not investigate the tibial slope as this measurement is calculated relative to the tibial mechanical axis. Some of our datasets included only the proximal tibia preventing proper calculation of the mechanical axis. Lastly, the measurements recorded from the bone models analyzed in this study did not contain hyaline cartilage. Two studies suggest the thickness of the articular cartilage in the knee follows the surface topography of the subchondral bone [5, 9]; therefore, measurements of the sagittal radii can be extrapolated from the bone measurements. The actual thickness of the articular cartilage is variable, with the thickest cartilage being central on the femoral condyle in the weightbearing region and the thinnest along the periphery in regions of less weightbearing. Hence, it is safe to assume the shape and dimension of the distal femur and proximal tibia measured along the periphery are impacted little by the thickness of the articular cartilage.
We identified ethnic differences among the three populations examined. We found AMs had a smaller ML/AP ratio than CMs (1.33 ± 0.12 versus 1.4 ± 0.06), contrary to Yue et al. [27] who reported a larger tibial aspect ratio in Chinese men compared to Caucasian men (1.82 ± 0.07 versus 1.75 ± 0.11). Our mean and SD values of the ML for CMs (79 ± 4.6 mm) and CFs (68.6 ± 4.8 mm) were comparable to those published by Yue et al. [27] who recorded 69 ± 4.2 mm for CFs and 78.7 ± 5 mm for CMs; however, the authors contradicted their finding in the conclusion by reporting Chinese men have wider proximal tibiae than CMs. In addition, our normalized ratios and nonlinear shape analysis supported differences between East Asians and Caucasians independent of any scale factor. We found differences in the ratio between AAF/CF and AAM/CM, with the mean ratio being larger in CMs compared to AAMs and CFs compared to AAFs. This finding conflicts with Gillespie et al. [8] who reported a larger ML/AP ratio in African Americans than in Caucasians; however, their African American population was from the early 20th century, which could account for differing anatomic features from the current population. The radii of curvature analysis on both the medial and lateral condyles revealed AMs and AFs tend to have more curved condyles (ie, less radius of curvature) than Caucasians, implying a larger ROM. This finding agrees with Leszko et al. [14] who found an increased ROM of 153° for AF and 151° for AM compared to 146° for CM.
We observed sex differences in each of the populations analyzed. Women from all ethnic groups had smaller, narrower knees with a smaller ML/AP ratio. These results are comparable to those reported in other studies [2, 8]. Although a number of studies have published results of sex differences, we find it difficult to compare measurements as each method utilized is different. Three-dimensional modeling of the distal femur and proximal tibia from CT and MRI has the advantage of obtaining the full shape of both bones, as well as obtaining the anatomic coordinate axes and rotational landmarks. Direct measurements during surgery and bone wafer measurements do not reveal the true shape, provide rotational references, or maintain coordinate axes [10, 25]. In addition, radiographic analysis creates a pattern of variability due to variations in the angle of the xray beam and magnification, not to mention the bone margins may not be representative of the true shape of the distal femur and proximal tibia [19]. However, we did find our MLs for CMs (85.9 ± 4.7 mm) and CFs (75.8 ± 3.3 mm) were comparable to the anthropologic measurement of bicondylar width taken by Alunni-Perret et al. [1] who recorded 84.3 ± 3.6 mm for CMs and 74.8 ± 2.5 mm for CFs. In addition, we found females tended to have more curved knees and thus higher ROM. This finding agrees with Leszko et al. [14] who measured an average maximum flexion of 152° for CFs and 153° for AFs compared to 146° and 151° for CMs and AMs.
In sizing the femoral component, the AP is important in maintaining the flexion-extension gap, optimizing patellofemoral tracking and tension in the quadriceps mechanism; all of which impact knee motion and stability. In contrast, the ML determines bone coverage and soft tissue tension. Current implant designs and surgical techniques account for morphologic differences by compromises during surgery to fit the average implant on the measured anatomy, avoiding overhang and soft tissue impingement with a larger prosthesis or instability with a smaller prosthesis.
New anatomic and morphologic insights for both the femur (Fig. 11) and tibia (Fig. 12) brought forth in this paper may help foster implant design changes in all component parts in TKA; however, further evaluation is needed to determine whether these design changes would improve clinical outcome. Ethnic differences in the anatomy of the knee have also been identified by this study. Some Asian surgeons claim current knee implants do not fulfill the requirements of their patient population [21]. Further investigation is needed to evaluate any clinical impact of implant designs based on these ethnic differences.
References
Alunni-Perret V, Staccini P, Quatrehomme G. Sex determination from the distal part of the femur in a French contemporary population. Forensic Sci Int. 2008;175:113–117.
Bellemans J, Carpentier K, Vandenneucker H, Vanlauwe J, Victor J. The John Insall Award. Both morphotype and gender influence the shape of the knee in patients undergoing TKA. Clin Orthop Relat Res. 2010;468:29–36.
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee. 2009;16:341–347.
Chiu KY, Ng TP, Tang WM, Cheng HC, Hung TS, Tse PY, Ko PS. The shape and size of femoral components in revision total hip arthroplasty among Chinese patients. J Orthop Surg (Hong Kong). 2003;11:53–58.
Cohen ZA, McCarthy DM, Kwak SD, Legrand P, Fogarasi F, Ciaccio EJ, Ateshian GA. Knee cartilage topography, thickness, and contact areas from MRI: in-vitro calibration and in-vivo measurements. Osteoarthritis Cartilage. 1999;7:95–109.
Conley S, Rosenberg A, Crowninshield R. The female knee: anatomic variations. J Am Acad Orthop Surg. 2007;15(Suppl 1):S31–S36.
DiBennardo R, Taylor JV. Sex assessment of the femur: a test of a new method. Am J Phys Anthropol. 1979;50:635–637.
Gillespie RJ, Levine A, Fitzgerald SJ, Kolaczko J, DeMaio M, Marcus RE, Cooperman DR. Gender differences in the anatomy of the distal femur. J Bone Joint Surg Br. 2011;93:357–363.
Hall FM, Wyshak G. Thickness of articular cartilage in the normal knee. J Bone Joint Surg Am. 1980;62:408–413.
Hitt K, Shurman JR 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85(Suppl 4):115–122.
Ho WP, Cheng CK, Liau JJ. Morphometrical measurements of resected surface of femurs in Chinese knees: correlation to the sizing of current femoral implants. Knee. 2006;13:12–14.
Hovinga KR, Lerner AL. Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J Orthop Res. 2009;27:1191–1196.
Jolliffe I. Principal Component Analysis. New York, NY: John Wiley & Sons, Ltd; 2005.
Leszko F, Hovinga KR, Lerner AL, Komistek RD, Mahfouz MR. In vivo normal knee kinematics: is ethnicity or gender an influencing factor? Clin Orthop Relat Res. 2011;469:95–106.
Mahfouz M, Badawi A, Merkl B, Abdel Fatah E, Pritchard E, Kesler K, Moore M, Jantz R, Jantz L. Patella sex determination by 3D statistical shape models and nonlinear classifiers. Forensic Sci Int. 2007;173:161–170.
Mahfouz MR. Implant Design Analysis Suite. USA; 2009. Patent Application Number WO/2009/025783, Section PCT/US2008/00983.
Mahfouz MR, Abdel Fatah EE, Merkl BC, Mitchell JW. Automatic and manual methodology for three-dimensional measurements of distal femoral gender differences and femoral component placement. J Knee Surg. 2009;22:294–304.
Mahfouz MR, Merkl BC, Fatah EE, Booth R Jr, Argenson JN. Automatic methods for characterization of sexual dimorphism of adult femora: distal femur. Comput Methods Biomech Biomed Engin. 2007;10:447–456.
Mensch JS, Amstutz HC. Knee morphology as a guide to knee replacement. Clin Orthop Relat Res. 1975;112:231–241.
Tamari K, Tinley P, Briffa K, Aoyagi K. Ethnic-, gender-, and age-related differences in femorotibial angle, femoral antetorsion, and tibiofibular torsion: cross-sectional study among healthy Japanese and Australian Caucasians. Clin Anat. 2006;19:59–67.
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y. Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. J Arthroplasty. 2002;17:1028–1032.
Urabe K, Mahoney OM, Mabuchi K, Itoman M. Morphologic differences of the distal femur between Caucasian and Japanese women. J Orthop Surg (Hong Kong). 2008;16:312–315.
Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty. 2000;15:79–85.
Van Gerven DP. The contribution of size and shape variation to patterns of sexual dimorphism of the human femur. Am J Phys Anthropol. 1972;37:49–60.
Westrich GH, Haas SB, Insall JN, Frachie A. Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasty. 1995;10:47–51.
Yip DK, Zhu YH, Chiu KY, Ng TP. Distal rotational alignment of the Chinese femur and its relevance in total knee arthroplasty. J Arthroplasty. 2004;19:613–619.
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G. Differences of knee anthropometry between Chinese and white men and women. J Arthroplasty. 2011;26:124–130.
Acknowledgments
The authors thank Gary To, Brian Petree, Andrew Milstead, and Griffin Smith for their efforts in data preparation.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Tennessee.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mahfouz, M., Abdel Fatah, E.E., Bowers, L.S. et al. Three-dimensional Morphology of the Knee Reveals Ethnic Differences. Clin Orthop Relat Res 470, 172–185 (2012). https://doi.org/10.1007/s11999-011-2089-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-2089-2