Abstract
Background
There is a trend toward decreasing length of hospital stay (LOS) after TKA although it is unclear whether this trend is detrimental to the overall postoperative course. Such information is important for future decisions related to cost containment.
Questions/purposes
We determined whether decreases in LOS after TKA are associated with increases in readmission rates.
Patients and Methods
We retrospectively reviewed the rates and reasons for readmission and LOS for 4057 Medicare TKA patients from 2002 to 2007. We abstracted data from the Medicare Patient Safety Monitoring System. Hierarchical generalized linear modeling was used to assess the odds of changing readmission rates and LOS over time, controlling for changes in patient demographic and clinical variables.
Results
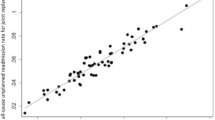
The overall readmission rate in the 30 days after discharge was 228/4057 (5.6%). The 10 most common reasons for readmission were congestive heart failure (20.4%), chronic ischemic heart disease (13.9%), cardiac dysrhythmias (12.5%), pneumonia (10.8%), osteoarthrosis (9.4%), general symptoms (7.4%), acute myocardial infarction (7.0%), care involving other specified rehabilitation procedure (6.3%), diabetes mellitus (6.3%), and disorders of fluid, electrolyte, and acid-base balance (5.9%); the top 10 causes did not include venous thromboembolism syndromes. We found no difference in the readmission rate between the periods 2002–2004 (5.5%) and 2005–2007 (5.8%) but a reduction in LOS between the periods 2002–2004 (4.1 ± 2.0 days) and 2005–2007 (3.8 ± 1.7 days).
Conclusions
The most common causes for readmission were cardiac-related. A reduction in LOS was not associated with an increase in the readmission rate in this sample. Optimization of cardiac status before discharge and routine primary care physician followup may lead to lower readmission rates.

Similar content being viewed by others
References
Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010;25:114–117.
Dall GF, Ohly NE, Ballantyne JA, Brenkel IJ. The influence of pre-operative factors on the length of in-patient stay following primary total hip replacement for osteoarthritis: a multivariate analysis of 2302 patients. J Bone Joint Surg Br. 2009;91:434–440.
Epps CD. Length stay, discharge disposition, and hospital charge predictors. AORN J. 2004;79:975–997.
Fontaine KR, Haaz S, Heo M. Projected prevalence of US adults with self-reported doctor-diagnosed arthritis, 2005 to 2050. Clin. Rheumatol. 2007;26:772–774.
Foote J, Panchoo K, Blair P, Bannister G. Length of stay following primary total hip replacement. Ann R Coll Surg Engl. 2009;91:500–504.
Forrest GP, Roque JM, Dawodu ST. Decreasing length of stay after total joint arthroplasty: effect on referrals to rehabilitation units. Arch Phys Med Rehabil. 1999;80:192–194.
Hayes JH, Cleary R, Gillespie WJ, Pinder IM, Sher JL. Are clinical and patient assessed outcomes affected by reducing length of hospital stay for total hip arthroplasty? J Arthroplasty. 2000;15:448–452.
Hunt DR, Verzier N, Abend SL, Lyder C, Jaser LJ, Safer N, Davern P. Fundamentals of Medicare patient safety surveillance: intent, relevance, and transparency. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation. Vol 2. Concepts and Methodology. Rockville, MD: Agency for Healthcare Research and Quality Publication Number 05-0021-2; 2005.
Husni ME, Losina E, Fossel AH, Solomon DH, Mahomed NN, Katz JN. Decreasing medical complications for total knee arthroplasty: effect of critical pathways on outcomes. BMC Musculoskelet Disord. 2010;11:160.
Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL, Kehlet H. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg. 2010;130:263–268.
Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79:168–173.
Husted H, Otte KS, Kristensen BB, Orsnes T, Kehlet H. Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg. 2010;130:1185–1191.
Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann. Surg. 2008;248:189–198.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–1121.
Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87:1222–1228.
Polk HC, Birkmeyer J, Hunt DR, Jones RS, Whittemore AD, Barraclough B. Quality and safety in surgical care. Ann. Surg. 2006;243:439–448.
Räsänen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynänen OP, Roine RP. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78:108–115.
Shetty VD, Nazare SP, Shitole BR, Jain SK, Kumar AV. Silent cardiac comorbidity in arthroplasty patients: an unusual suspect? J Arthroplasty. 2011;26:375–378.
Urban MK, Jules-Elysee K, Loughlin C, Kelsey W, Flynn E. The one year incidence of postoperative myocardial infarction in an orthopedic population. HSS J. 2008;4:76–80.
van Klei WA, Bryson GL, Yang H, Forster AJ. Effect of beta-blocker prescription on the incidence of postoperative myocardial infarction after hip and knee arthroplasty. Anesthesiology. 2009;111:717–724.
Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C, Hobson P, Greengold N. Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study. Am J Med. 1998;105:33–40.
Author information
Authors and Affiliations
Corresponding author
Additional information
WJM receives royalties from Zimmer Inc (Warsaw, IN) and Wright Medical Technology, Inc (Arlington, TN). JIH receives research support from Biomet Inc (Warsaw, IN) and is a consultant to Zimmer Inc (Warsaw, IN), Biomet, Smith and Nephew Inc (Memphis, TN), and PorOsteon Inc (Menlo Park, CA). All other authors certify that they have no commercial associations that might pose a conflict of interest in connection with the submitted article.
These data were generated by the US Department of Health and Human Services and thus review by our local institutional review board is not required.
Work performed at Qualidigm and Stanford University.
About this article
Cite this article
Vorhies, J.S., Wang, Y., Herndon, J.H. et al. Decreased Length of Stay After TKA Is Not Associated With Increased Readmission Rates in a National Medicare Sample. Clin Orthop Relat Res 470, 166–171 (2012). https://doi.org/10.1007/s11999-011-1957-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-1957-0