Opinion statement
Traumatic brain injury (TBI) is a complex disease process that requires constant attention as one manages the associated body systems. Even though an “isolated” brain injury may be the cause for admission to the hospital, the injured brain cannot be thought of in isolation from the remainder of the body. All body systems, from cardiac to pulmonary, need to be addressed as one moves from the initial to the long-term management of the TBI. The multiple issues are best addressed with a dedicated neurocritical care team that is in continuous communication with the neurosurgical team throughout the course of treatment. To date, no pharmacologic treatment has led to improved outcomes after TBI, but it is becoming increasingly clear that advances in the critical care of TBI patients are contributing to better results.
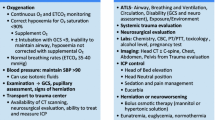
During resuscitation of the TBI patient, medical management in its simplest form strives to return measurable vital signs and laboratory values (eg, intracranial pressure, mean arterial pressure, blood glucose, PaO2, or PaCO2) to their normal range. The initial goal is to maintain or reestablish normal homeostasis.
The initial injury to the brain is irreversible by any medical modalities available today. After the initial resuscitation, medical maneuvers are directed at limiting secondary damage to the brain. Secondary brain injury occurs in response to inflammatory changes, expanding hematomas, cellular swelling, seizures, and systemic complications (ie, hemodynamic or pulmonary changes, fever, pain); vulnerable surrounding brain tissue can be damaged through alterations in cerebral perfusion and metabolism. Treatments to address these issues include, but are not limited to, analgesics, sedatives, anticonvulsants, hyperosmotic agents, and hypothermia.
The future of TBI care likely lies in the areas of better injury classification to guide therapeutic interventions, management of secondary injury, improved technology for intracranial monitoring, and regeneration/rehabilitation. Studies focusing on signaling pathways, neural stem cells, and reparative medications are all in the early stages of development; their use is currently experimental at best.
There are few areas in medicine where clinicians have the opportunity to impact a patient’s life to the degree seen in the management of TBI. Although parts of the proverbial puzzle certainly remain unsolved, it is the remarkable recoveries that patients make with the therapeutic modalities available today that keep management of TBI one of the most exciting areas in medicine.
Similar content being viewed by others
Introduction
Each year, about 1.5 million people in the United States incur a traumatic brain injury (TBI), a number that far outpaces new cases of cancer. TBI contributes to 50,000 deaths and at least 235,000 hospitalizations each year in the United States [1]. The effects on society are profound, especially when lost wages and productivity are considered. The annual cost of TBI in the United States is estimated to be $62 billion [1]. The demographics of TBI show that males are twice as likely as females to sustain a TBI, and the most frequent mechanism of TBI is motor vehicle crashes [2]. Age also makes a difference: children between the ages of ages 0–4 and 15–19 years are at the highest risk for an injury, whereas adults over the age of 75 are most likely to die from a TBI [2]. Morbidity and mortality related to TBI often are not directly related to the brain injury itself, but rather may be due to complications that result from the inability of a comatose patient to protect the airway or ambulate.
The appropriate management of TBI begins before patients arrive at the hospital and continues long after their discharge. Advances in neuromonitoring, neuroimaging and neurocritical care have drastically changed the medical management and outcomes of TBI [3]. Biomarkers of brain injury and genetic testing to guide the use of central nervous system (CNS)—specific therapies are likely to be critical in the future of TBI management.
Treatment
-
Over the past two decades, TBI has been identified as a major cause of death and disability, especially in young and previously healthy patients. Hospitalizations and morbidity related to TBI have decreased over this period as a result of improved awareness [4] and specialization of care delivery.
Diet and lifestyle
-
No single diet or lifestyle variable has been shown to be protective in TBI. Outcomes of TBI are worse in obese patients, but the higher rate of mortality and complications in obese patients appears to depend largely on age and other associated medical conditions [5].
-
The use of restraint devices in automobiles and helmets during motorcycle riding and sports activities has proven to be beneficial. Their use must be emphasized by the health care system [6,7].
-
The role of appropriate nutrition replacements is important in the course of recovery, especially with severe head injuries. Initiation of feeding within 48 h of TBI is associated with improved outcomes and should be stressed in the immediate postresuscitation period (Level II evidence, moderate clinical certainty) [8].
Pharmacologic treatment
-
Various types of pharmacologic agents are used to limit secondary damage to the injured brain during the healing process. Although the same medications used in intensive care units are commonly used in managing TBI patients, the use of some drugs (as discussed below) is unique to this patient population.
-
Corticosteroids were associated with increased mortality in a large, multicenter, randomized, placebo-controlled clinical trial. The use of corticosteroids is contraindicated in TBI patients (Level I evidence, a high degree of clinical certainty) [9••,10, Class I].
Sedatives
-
The use of sedatives for management of patients with TBI is a Level II recommendation (moderate clinical certainty) [9••].
Propofol
- Standard dosage :
-
Often given as a continuous infusion with a range of 50–100 μg/kg per minute.
- Contraindications :
-
Should be avoided in children and in patients with allergies to eggs, egg products, soybeans, or soy products.
- Main drug interactions :
-
No absolute drug interactions, although lower doses of propofol are often required in patients receiving opioids.
- Main side effects :
-
Cardiac and respiratory depression are common. Propofol is avoided in children, because of a higher risk of propofol infusion syndrome and liver dysfunction [11].
- Special points :
-
Propofol has become the sedative of choice in many neuro-intensive care units because of its rapid onset and short half-life. Care must be taken with long-term infusions, as they have been associated with complications.
- Cost/cost-effectiveness :
-
Expensive but cost-effective for desired outcome.
Midazolam
- Standard dosage :
-
Typically given intravenously (IV) either as single bolus doses of 1–2 mg or a continuous infusion in the range of 0.01–0.1 mg/kg per hour.
- Contraindications :
-
Known drug allergy, narrow-angle glaucoma.
- Main drug interactions :
-
Caution is advised when midazolam is administered with drugs that are known to inhibit the P450 3A4 enzyme system. Care must be taken when combined with other sedating drugs, as effects may be potentiated.
- Main side effects :
-
Retrograde amnesia, cardiac arrhythmias, hypotension.
- Special points :
-
Care and proper monitoring are required, as midazolam has been associated with cardiac and respiratory arrest.
- Cost/cost-effectiveness :
-
Expensive.
Lorazepam
- Standard dosage :
-
Can be used in oral or IV formulation; a typical dosage ranges from 1 to 10 mg/d.
- Contraindications :
-
Pregnancy, allergy to benzodiazepines, acute narrow-angle glaucoma.
- Main drug interactions :
-
Increased sedative effects when given with other CNS depressants (ie, alcohol, barbiturates, opioids). Probenecid and valproate increase the effective concentration of lorazepam through inhibition of glucuronidation. Theophylline or aminophylline may reduce the sedative effects of benzodiazepines, including lorazepam, by increasing clearance.
- Main side effects :
-
Sedation, weakness, dizziness, unsteadiness of gait.
- Special points :
-
Lorazepam is used in the TBI patient for both its sedative and antiepileptic effects. With prolonged use, lorazepam may accumulate in fat tissue, so sedative effects may persist after discontinuation.
- Cost/cost-effectiveness :
-
Moderate cost.
Quetiapine fumarate
- Standard dosage :
-
The typical starting dosage in patients with TBI is 25 mg twice daily. This dose is much lower than that typically used for psychiatric disorders.
- Contraindications :
-
None identified.
- Main drug interactions :
-
Poorly recognized at this time, but care must be taken when combining with any centrally acting drug.
- Main side effects :
-
Headache, agitation, somnolence.
- Special points :
-
Care must be taken with long-term administration of this drug in patients with depression or in elderly patients with psychotic dementia, owing to evidence of increased mortality rates. This agent may be particularly helpful in the combative, agitated TBI patient.
- Cost/cost-effectiveness :
-
Expensive; cost-effectiveness varies depending on the patient.
Dexmedetomidine hydrochloride
- Standard dosage :
-
A loading dose of 1 μg/kg over 10 min with a maintenance dose of 0.2–0.7 μg/kg per hour can be used. The maintenance infusion can be adjusted for patient comfort.
- Contraindications :
-
Prior allergic reaction.
- Main drug interactions :
-
Care must be taken when given with other sedatives or opioids.
- Main side effects :
-
Cardiovascular effects, sedation.
- Special points :
-
This is a newer agent that has potential for widespread use in the neuro-intensive care unit. The rapid on-off characteristics of dexmedetomidine make it an option for procedural uses. Because it causes little respiratory depression, dexmedetomidine may become the drug of choice for ventilator weaning and extubation.
- Cost/cost-effectiveness :
-
Very expensive; cost-effectiveness yet to be determined.
Trazodone
- Standard dosage :
-
Doses of 50–100 mg are typically given at night to address anxiety and restore sleep-wake cycles.
- Contraindications :
-
Prior allergic reaction.
- Main drug interactions :
-
Potentiated action when combined with other antidepressants.
- Main side effects :
-
Drowsiness and lightheadedness are the most common.
- Special points :
-
Long-term use has been associated with an increased risk of suicide, but the impact of this risk is unclear in the inpatient setting.
- Cost/cost-effectiveness :
-
Moderate price; cost-effectiveness depends on the patient.
Antiepileptic drugs
-
The use of antiepileptic drugs for management of patients with TBI is a Level II recommendation (moderate clinical certainty) [9••].
Phenytoin
- Standard dosage :
-
The goal range for clinical effectiveness is a serum level ranging from 10 to 20 μg/mL. Patients should receive an IV loading dose of 10–20 mg/kg, followed by a maintenance dose of 5 mg/kg per day in divided doses.
- Contraindications :
-
Prior allergic reaction to phenytoin or hydantoins.
- Main drug interactions :
-
Many drugs can alter the metabolism of phenytoin, and care must be taken to follow therapeutic ranges to guide daily dose adjustments.
- Main side effects :
-
The main side effects of IV formulations are hypotension and cardiac arrhythmias. Both IV and oral formulations can cause nystagmus, dizziness, ataxia, and altered level of consciousness. Systemic side effects can include nausea, hematopoietic suppression, and a skin reaction of the Stevens-Johnson type.
- Special points :
-
In TBI, phenytoin is indicated for the prevention and control of seizures resulting from brain trauma. Fosphenytoin is a phosphorylated version of phenytoin that can be infused more rapidly and has slightly fewer hemodynamic effects. Its dosing is similar to phenytoin.
- Cost/cost-effectiveness :
-
Moderate cost; IV formulations are more expensive.
Levetiracetam
- Standard dosage :
-
Initial daily doses range from 500 to 3000 mg divided between two daily doses, with a maximum daily dose of 6000 mg per day. IV and oral formulations are available, and doses are clinically equivalent. The serum level of levetiracetam provides little information regarding effective dosing; therefore, the drug is titrated to effect.
- Contraindications :
-
Prior allergic reaction to levetiracetam.
- Main drug interactions :
-
None yet shown to be prevalent.
- Main side effects :
-
Many CNS side effects have been observed, ranging from somnolence to agitation, but these are usually mild. General symptoms of nausea, rhinitis, and cough can also occur.
- Special points :
-
Levetiracetam is a newer antiepileptic drug that is being used more frequently in critically ill neurologic patients. A major advantage of this medication is that levels do not have to be followed or adjusted to a specific range, and the side effect profile appears better than the profile for phenytoin [12, Class II]. It can be used for both prevention and treatment of posttraumatic seizures.
- Cost/cost-effectiveness :
-
Expensive but effective; significant price differences between IV and oral formulations.
Sedative/antiepileptic drug
-
The use of high-dose barbiturates for management of refractory ICP elevations in patients with TBI is a Level II recommendation (moderate clinical certainty) [9••].
Pentobarbital
- Standard dosage :
-
This medication may be used to treat elevations in intracranial pressure (ICP) that are refractory to other medical interventions. In this situation, a continuous infusion of pentobarbital is used to achieve burst suppression on EEG monitoring. The loading dose is 10–20 mg/kg, followed by an infusion of 1–3 mg/kg per hour. The dose is titrated based on the EEG response. Pentobarbital may also be used for its potent antiepileptic effects in a patient with known refractory status epilepticus.
- Contraindications :
-
Prior hypersensitivity to barbiturates or history of porphyria.
- Main drug interactions :
-
Can affect anticoagulant levels, corticosteroids, antiepileptic drugs, and other CNS depressants.
- Main side effects :
-
Hemodynamic collapse can occur; patients receiving pentobarbital must be continuously monitored. A global hypometabolic state occurs with prolonged use, resulting in impaired gastrointestinal motility, cardiac function, and immunologic responses.
- Special points :
-
Pentobarbital is a powerful agent to reduce and control ICP in the patient with refractory intracranial hypertension. Care must be taken when deciding to use pentobarbital, as the neurologic examination is lost and side effects can be catastrophic.
- Cost/cost-effectiveness :
-
Moderate cost but effective.
Analgesics
-
The use of analgesics for management of patients with TBI is a Level II recommendation (moderate clinical certainty) [9••].
Fentanyl
- Standard dosage :
-
Can be used at intermittent IV doses of 25–100 μg for pain control. Continuous IV infusion of 25–100 μg/h is common and can be titrated to effectiveness.
- Contraindications :
-
Prior allergic reaction to fentanyl or other opioids.
- Main drug interactions :
-
Synergistic effects when given with other CNS depressants such as opioids, benzodiazepines, or muscle relaxants. Fentanyl is metabolized via the human cytochrome P450 3A4 enzyme system, so drugs that affect this system can raise or lower fentanyl concentrations.
- Main side effects :
-
Respiratory depression, hypotension, nausea, vomiting, and constipation are commonly observed.
- Special points :
-
Commonly used in the intensive care unit, as it provides rapid onset and is metabolized quickly, allowing frequent neurologic assessments. IV morphine is used for analgesia in many facilities, but fentanyl is generally preferred because of its rapid effect and clearance.
- Cost/cost-effectiveness :
-
Moderate cost but effective.
Osmotic agents
-
The use of osmotic agents (specifically mannitol) for management of patients with TBI and increased ICP is a Level II recommendation (moderate clinical certainty) [9••].
Mannitol
- Standard dosage :
-
Typically given as an IV bolus of 0.25–1 g/kg with suspected herniation or elevated ICP. Infusion should be completed over 30–60 min.
- Contraindications :
-
Should not be used in patients with anuric renal failure or hypovolemia. Renal failure can occur in severely dehydrated patients. Patients with heart failure and pulmonary edema must be followed carefully, as these conditions may worsen.
- Main drug interactions :
-
None are typical or common.
- Main side effects :
-
Hypotension, electrolyte imbalances, tachycardia, and marked diuresis are common.
- Special points :
-
This is an effective agent for rapid reduction of ICP. Care must be taken when repeated doses are used, because of the risk of diuresis and hypovolemia.
- Cost/cost-effectiveness :
-
Expensive but cost-effective for desired outcome.
Hypertonic saline
- Standard dosage :
-
May be used in bolus dosing or as a continuous infusion to achieve goal serum sodium of 145–160 mEq/L. Bolus dosing may use different concentrations of hypertonic saline ranging from 3% to 23.4%. Continuous infusions generally use 3% hypertonic saline. The decision regarding method of dosing is often institutionally determined. Dosing is determined by the concentration of hypertonic saline used.
- Contraindications :
-
Should not be used in TBI patients with symptoms of diabetes insipidus. Risk is extremely high in patients with renal failure, and caution should be used in patients with congestive heart failure or pulmonary edema.
- Main drug interactions :
-
None are known.
- Main side effects :
-
Vein site thrombosis and phlebitis require that this agent be given via a central venous line.
- Special points :
-
Provides rapid-onset reduction of ICP and may be the fluid of choice in hypovolemic TBI patients during their initial resuscitation, as intravascular volume can be increased while reducing ICP.
- Cost/cost-effectiveness :
-
Expensive but effective.
Interventional procedures/ assistive devices
-
Most interventional procedures in TBI patients (except for external ventricular drains) are for diagnostic purposes rather than for treatment. Individualized clinical judgment and patient-by-patient evaluation cannot be emphasized enough. It is generally accepted that patients who have a score 8 or less on the Glasgow Coma Scale with an abnormal head CT scan, or those with a normal CT scan but evidence of hypotension, motor posturing, or age over 40 years require invasive monitoring for ICP, brain-tissue oxygen measurement, and so forth. Patients with normal findings on head CT may require invasive monitoring if examinations cannot be performed for extended periods (eg, during long operations). Methods of monitoring used in the TBI patient include:
-
Fiberoptic monitoring to continuously measure ICP. Clinical evidence exists supporting the use of ICP monitoring for early detection of intracranial mass lesions [13]. Once elevated ICP has been identified, therapeutic interventions such as ventilator adjustments, osmotic therapy, and surgical decompression all may be treatment options. In addition, ICP measurements can help to assess prognosis. ICP monitoring is recommended by consensus guidelines for head injury management [9••,14].
-
External ventricular drains (EVDs) can be placed to monitor and treat elevated ICP [15]. EVDs can be placed at the bedside without transporting patients to the operating room. To function correctly, the drain must be placed into the ventricular system and have a continuous fluid column. An EVD is generally preferred to fiberoptic ICP monitoring alone, as it is more accurate and allows therapeutic drainage.
-
Brain tissue oxygen (PbtO 2 ) monitoring has been available for many years but only recently has been widely used to provide data complementary to ICP monitoring. PbtO2 is thought to represent the diffusion of dissolved plasma oxygen into the brain. Low PbtO2 values have been associated with increased mortality and worse neurologic outcomes, and thus may be a potential target for intervention [16, Class III]. Further studies are needed, as recent data have questioned the efficacy of PbtO2-guided management [17,18].
-
Continuous electroencephalography (cEEG) is being used more frequently since a study showed that 24% of comatose TBI patients were demonstrating seizure activity (half nonconvulsive) [19, Class II]. The need for early identification of seizure activity after TBI is important, as early posttraumatic seizure activity has been associated with poor outcome [20].
-
Microdialysis is a technique that places a small catheter into brain parenchyma to measure extracellular levels of glucose, lactate, pyruvate, glutamate, and glycerol, which can provide information regarding cellular distress. Additional metabolites being explored are nitric oxide and markers of inflammation, which may help with prognostication [21]. In addition, microdialysis measurement of brain glucose has provided data showing that tight systemic glucose control was associated with reduced cerebral glucose levels, elevated lactate/pyruvate ratios, and increased mortality, which may be due to energy failure [22•, Class II]. Microdialysis is not a new technique, but it remains experimental because the value of real-time use of the information it provides remains unclear, as do the ideal metabolites for monitoring.
-
Diagnostic angiography was used in the pre-CT era to evaluate for midline shift and the presence of intracranial mass lesions. Currently, diagnostic angiography is used to evaluate suspected traumatic dissection after blunt-force trauma, which has a reported incidence of up to 20% [23]. Unexplained strokes in the TBI patient require further investigation of intracranial and extracranial vasculature. CT angiography has recently gained acceptance as a viable noninvasive alternative [24].
-
MRI is an expanding modality in the area of TBI. MR spectroscopy (MRS) is a noninvasive imaging technique that uses spectroscopic methods to evaluate specific areas of the brain. This technique has been shown to reveal injury that is not obvious on other modalities, and it provides prognostic information [25, Class II]. Diffusion tensor imaging (DTI) and tractography can identify traumatic axonal injury, which has been associated with worse outcome [26].
-
Surgery
-
In its simplest form, the goal of surgery in TBI is to evacuate a mass lesion and/or provide room for the injured brain to swell in order to preserve the vital deep structures of the brain.
-
Immediately after injury, surgical decompression is often used for evacuation of intracranial mass lesions (subdural, epidural, or intraparenchymal). Criteria regarding age, type of lesion, and associated comorbidities are available to aid in determining surgical candidates and appropriate therapy [27–30].
-
Delayed surgical decompression (mainly by means of decompressive craniectomy) can also be performed when medical management for elevated ICP has failed. It has been shown to improve outcome when carried out in an appropriate patient population [9••,31,32].
Physical/speech therapy and exercise
-
Physical therapy and speech/cognitive therapy play important roles in recovery. Early rehabilitative interventions are associated with significant recovery even in patients with severe TBI [33•].
-
The impact of brain injury is far-reaching, and significant cognitive impairment may be seen for years after the injury, even in patients with good outcomes [34]. This fact often makes it difficult for the TBI patient to return to his or her prior occupation, resulting in significant economic costs to society, which have been estimated to be 62 billion dollars annually in the United States [1].
Other treatments / emerging therapies
-
As discussed earlier, TBI is divided into primary and secondary injury phases. The primary injury is irreversible. Current care of the TBI patient focuses on managing the secondary physiologic responses to the initial injury. Research efforts have been directed at isolating and minimizing factors that contribute to secondary injury.
-
Both hypotension (systolic blood pressure < 90 mm Hg [Level II, moderate clinical certainty]) and hypoxemia (PaO2 < 60 mm Hg or SaO2 < 90% [Level III, unclear clinical certainty]) have been associated with increased mortality and morbidity after TBI. Every effort should be made to maintain adequate blood pressure and oxygenation [9••].
-
The general hypometabolic state induced by hypothermia was thought to provide protection from secondary injury [35, Class II]. Unfortunately, TBI usually does not occur in isolation. The systemic effects of hypothermia can have deleterious consequences on other aspects of critical care after trauma, and these may cancel any potential neurologic benefits (Level III, unclear clinical certainty) [36]. Induced normothermia recently has been associated with improved outcomes and may be the appropriate course of action (Level II, moderate clinical certainty) [37].
-
TBI is an active area of clinical research, with both medical and surgical interventions currently under investigation. Medical trials currently active or under development include the use of progesterone [38, 39], endothelin receptor antagonists [40], and cyclosporine [41]. Randomized surgical trials currently under way are examining the surgical timing of decompressive hemicraniectomy [42], the utility of decompressive craniectomy for refractory elevated ICP [43], and the evacuation of traumatic intracranial hemorrhage [44].
-
Genetic testing and biochemical markers may come to play important roles in prognosis and treatment. At some time in the future, patients with TBI who arrive in the ICU may be subject to a battery of tests that directs an individualized course of care.
Pediatric considerations
-
Pediatric TBI has unique issues that make management and outcome differ from management and outcome in adults [45, 46]. The mechanism of injury in the pediatric population generally falls into one of two groups: accidental or nonaccidental trauma. Neurologic recovery in nonaccidental trauma is uniformly poorer than for matched accidental trauma, even in the cases of clinically minor injuries [47]. The social implications of nonaccidental trauma are far-reaching and the best interest of the child must be considered during the course of his or her care.
-
Unique factors that must be addressed are potential underlying congenital anomalies, differing physiological factors such as blood flow and general hemodynamics, and the differing support systems needed for long-term care and rehabilitation required in the pediatric patient. The large volume ratio of brain to body, the presence of open fontanelles, and the low circulating blood volume are also physiological differences that must be kept in mind when caring for pediatric TBI patients.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance, •• Of major importance
Centers for Disease Control and Prevention: Traumatic brain injury. Available at http://www.cdc.gov/ncipc/tbi/TBI.htm. Accessed December 29, 2009.
Langlois JA, Rutland-Brown W, Thomas KE: Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2006. Available at http://www.cdc.gov/ncipc/pub-res/TBI_in_US_04/TBI%20in%20the%20US_Jan_2006.pdf. Accessed December 29, 2009.
Lu J, Marmarou A, Choi S, et al.: Mortality from traumatic brain injury. Acta Neurochir Suppl 2005, 95:281–285.
Adekoya N, Thurman DJ, White DD, Webb KW: Surveillance for traumatic brain injury deaths—United States, 1989–1998. MMWR Surveill Summ 2002, 51(10):1–14.
Brown CV, Rhee P, Neville AL, et al.: Obesity and traumatic brain injury. J Trauma 2006, 61(3):572–576.
McDermott F, Lane J, Brazenor G, Debney E: The effectiveness of bicycle helmets: a study of 1710 casualties. J Trauma 1993, 34:834–845.
Coimbra R, Conroy C, Hoyt DB, et al.: The influence of damage distribution on serious brain injury in occupants in frontal motor vehicle crashes. Accid Anal Prev 2008, 40(4):1569–1575.
Härtl R, Gerber LM, Ni Q, Ghajar J: Effect of early nutrition on deaths due to severe traumatic brain injury. J Neurosurg 2008, 109(1):50–56.
Brain Trauma Foundation: Guidelines for Management of Severe Traumatic Brain Injury, edn 3. New York: Brain Trauma Foundation; 2007. Available at http://www.braintrauma.org/site/DocServer/Guidelines_Management_2007w_bookmarks.pdf?docID=621. Accessed December 29, 2009. The Brain Trauma Foundation guidelines are a comprehensive guide for management of traumatic brain injury. Solutions to questions about patient care and level of evidence of current therapies are available from this source and can be used for patient care.
Roberts I, Yates D, Sandercock P, et al.: Effect of intravenous corticosteroids on death within 14 days in 10,008 adults with clinically significant head injury (MRC CRASH trial): randomized placebo-controlled trial. Lancet 2004, 364:1321–1328.
Vasile B, Rasulo F, Candiani A, Latronico N: The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med 29(9):1417–1425.
Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA: Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam vs. phenytoin for seizure prophylaxis. Neurocrit Care, published online Nov 9, 2009.
Smith M: Monitoring intracranial pressure in traumatic brain injury. Anesth Analg 2008, 106:240–248.
Brain Trauma Foundation: Guidelines for Prehospital Management of Traumatic Brain Injury. New York: Brain Trauma Foundation, 2000.
Timofeev I, Dahyot-Fizelier C, Keong N, et al.: Ventriculostomy for control of raised ICP in acute traumatic brain injury. Acta Neurochir Suppl 2008, 102:99–104.
Van den Brink WA, van Santbrink H, Steyerberg EW, et al.: Brain oxygen tension in severe head injury. Neurosurgery 2000, 46:868–878.
Martini RM, Deem S, Yanez ND, et al.: Management guided by brain tissue oxygen monitoring and outcome following severe traumatic brain injury. J Neurosurg 2009, 111:644–649.
Meixensberger J, Jaeger M, Väth A, et al.: Brain tissue oxygen guided treatment supplementing ICP/CPP therapy after traumatic brain injury. J Neurol Neurosurg Psychiatry 2003, 74(6):760–764.
Vespa PM, Nuwer MR, Nenov V, et al.: Increased incidence and impact of nonconvulsive and convulsive seizures after traumatic brain injury as detected by continuous electroencephalographic monitoring. J Neurosurg 1999, 91(5):750–760.
Wang HC, Chang WN, Chang HW, et al.: Factors predictive of outcome in posttraumatic seizures. J Trauma 2008, 64:883–888.
Goodman JC, Robertson CS: Microdialysis: is it ready for prime time? Curr Opin Crit Care 2009, 15(2):110–117.
Oddo M, Schmidt JM, Carrera E, et al.: Impact of tight glycemic control on cerebral glucose metabolism after severe brain injury: a microdialysis study. Crit Care Med 2008, 36(12):3233–3238.
Mulloy JP, Flick PA, Gold RE: Blunt carotid injury: a review. Radiology 1998, 207:571–585.
Berne JD, Norwood SH: Blunt vertebral artery injuries in the era of computed tomographic angiographic screening: incidence and outcomes from 8292 patients. J Trauma 2009, 67(6):1333–1338.
Shutter L, Tong KA, Lee A, Holshouser BA: Prognostic role of proton magnetic resonance spectroscopy in acute traumatic brain injury. J Head Trauma Rehabil 2006, 21(4):334–349.
Lipton ML, Gellella E, Lo C, et al.: Multifocal white matter ultrastructural abnormalities in mild traumatic brain injury with cognitive disability: a voxel-wise analysis of diffusion tensor imaging. J Neurotrauma 2008, 25(11):1335–1342.
Bullock MR, Chesnut R, Ghajar J, et al.; Surgical Management of Traumatic Brain Injury Author Group: Surgical management of acute epidural hematomas. Neurosurgery 2006, 58(3 Suppl):S7–S15, discussion Si–Siv.
Bullock MR, Chesnut R, Ghajar J, et al.; Surgical Management of Traumatic Brain Injury Author Group: Surgical management of acute subdural hematomas. Neurosurgery 2006, 58(3 Suppl):S16–S24, discussion Si–Siv.
Bullock MR, Chesnut R, Ghajar J, et al.; Surgical Management of Traumatic Brain Injury Author Group: Surgical management of traumatic parenchymal lesions. Neurosurgery 2006, 58(3 Suppl):S25–S46, discussion Si–Siv.
Maas AI, Marmarou A, Murray GD, et al.: Prognosis and clinical trial design in traumatic brain injury: the IMPACT study. J Neurotrauma 2007, 24:232–238.
Chibbaro S, Tacconi L: Role of decompressive craniectomy in the management of severe head injury with refractory cerebral edema and intractable intracranial pressure. Our experience with 48 cases. Surg Neurol 2007, 68(6):632–638.
Aarabi B, Hesdorffer DC, Ahn ES, et al.: Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg 2006, 104(4):469–479.
Choi JH, Jakob M, Stapf C, et al.: Multimodal early rehabilitation and predictors of outcome in survivors of severe traumatic brain injury. J Trauma 2008, 65(5):1028–1035.
Draper K, Ponsford J: Cognitive functioning ten years following traumatic brain injury and rehabilitation. Neuropsychology 2008, 22(5):618–625.
Marion DW, Penrod LE, Kelsey SF, et al.: Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med 1997, 336(8):540–546.
Peterson K, Carson S, Carney N: Hypothermia treatment for traumatic brain injury: a systematic review and meta-analysis. J Neurotrauma 2008, 25(1):62–71.
Puccio AM, Fischer MR, Jankowitz BT, et al.: Induced normothermia attenuates intracranial hypertension and reduces fever burden after severe traumatic brain injury. Neurocrit Care 2009, 11(1):82–87.
SyNAPSe (Study of the Neuroprotective Activity of Progesterone in Severe Traumatic Brain Injuries). http://www.synapse-trial.com/. Accessed December 29, 2009.
Wright DW, Kellermann AL, Hertzberg VS, et al.: ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med 2007, 49(4):391–402.
A phase 2a dose escalation study with SLV334 in patients traumatic brain injury. http://clinicaltrials.gov/ct2/show/NCT00735085. Accessed December 29, 2009.
Empey PE, McNamara PJ, Young B, et al.: Cyclosporin A disposition following acute traumatic brain injury. J Neurotrauma 2006, 23(1):109–116.
The DECRA Trial: early decompressive craniectomy in patients with severe traumatic brain injury. http://clinicaltrials.gov/ct2/show/NCT00155987. Accessed December 29, 2009.
Randomised Evaluation of Surgery with Craniectomy for Uncontrollable Elevation of Intra-Cranial Pressure. http://www.rescueicp.com/. Accessed December 29, 2009.
Surgical trial in traumatic intracerebral haemorrhage. STITCH (Trauma). Available at http://research.ncl.ac.uk/trauma.STITCH/documents/Summary.pdf. Accessed December 29, 2009.
James HE: Pediatric head injury: What is unique and different? Acta Neurochir Suppl 1999, 73:85–88.
Roaten JB, Partrick DA, Nydam TL, et al.: Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level 1 pediatric trauma center. J Pediatr Surg 2006, 41(12):2013–2015.
Vinchon M, Defoort-Dhellemmes S, Desurmont M, Dhellemmes P: Accidental and nonaccidental head injuries in infants: a prospective study. J Neurosurg 2005, 102(4 Suppl):380–384.
Disclosure
Dr. Shutter has received research support from UCB Pharma, the US Department of Defense, and the National Institutes of Health. No other potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Losiniecki, A., Shutter, L. Management of Traumatic Brain Injury. Curr Treat Options Neurol 12, 142–154 (2010). https://doi.org/10.1007/s11940-010-0063-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-010-0063-z