Opinion statement
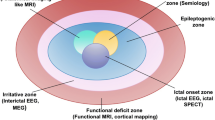
Partial seizures of extratemporal origin may present unique challenges in the patient with medically refractory seizures. The efficacy of an extratemporal focal cortical resection may be less effective than an anterior temporal lobectomy for intractable epilepsy. The potential operative complications may be increased in individuals with extratemporal epilepsy because of functional cerebral cortex involvement and the need for a large cortical resection to significantly reduce seizure tendency. Partial seizures of extratemporal origin are predominantly associated with frontal lobe epilepsy. The most effective treatment for intractable partial epilepsy is a focal cortical resection with excision of the epileptogenic zone, that is, an area of ictal onset and initial seizure propagation. The preoperative evaluation and operative strategy in patients with partial epilepsy of extratemporal origin associated with pharmacoresistant seizures is determined by the anatomic localization of the epileptogenic zone and the presence of a substrate-directed disorder. The goals of surgical treatment in extratemporal epilepsy include rendering the patient seizure-free, avoiding operative morbidity, and allowing the individual to become a participating and productive member of society. Before surgical treatment, the individual with extratemporal epilepsy will require a comprehensive preoperative evaluation, including routine electroencephalogram (EEG), long-term EEG monitoring, neuropsychologic studies, and magnetic resonance imaging (MRI). Patients with a normal MRI study, conflicting preoperative evaluation, or involvement of suspected functional cerebral cortex would require chronic intracranial EEG monitoring. The rationale for intracranial EEG includes localization of the ictal onset zone or intraoperative functional mapping, or both. Two-fluorodeoxyglucose positron emission tomography studies are usually unremarkable in patients with extratemporal epilepsy and normal MRI scans. Subtraction ictal single photon emission computed tomography coregistered to MRI (SISCOM) study may be useful to demonstrate a localized cerebral perfusion alteration in patients with intractable partial epilepsy. The diagnostic yield of SISCOM has been confirmed in patients with extratemporal epilepsy undergoing surgical treatment. The results of the SISCOM study may tailor the placement of intracranial EEG electrodes and affect the operative strategy. Patients with extratemporal epilepsy overall are less favorable operative candidates than individuals with medial temporal lobe epilepsy. However, individuals with MRI-identified lesional pathology of SISCOM-identified perfusion alterations concordant with the epileptogenic zone may be considered for surgical treatment. Chronic intracranial EEG monitoring may be necessary to confirm the localization of the ictal onset zone before epilepsy surgery. Patients with normal neuroimaging studies and extratemporal epilepsy are unlikely to be rendered seizurefree with focal cortical resection and should be considered candidates for other alternative forms of treatment for intractable partial epilepsy. Patients with non-substrate-directed extratemporal epilepsy should undergo a preoperative evaluation and surgical treatment at a comprehensive epilepsy center with extensive experience in chronic intracranial EEG monitoring and contemporary neuroimaging procedures because of the inherently high acuity associated with the operative management clinical disorder.
Similar content being viewed by others
References and Recommended Reading
Hauser W: The natural history of drug resistant epilepsy: epidemiologic considerations. Epilepsy Res 1992, 5(suppl):25–28.
Hauser A, Hesdorffer D: Prognosis. In Epilepsy: Frequency, Causes and Consequences. Edited by Hauser WA, Hesdorffer DC. New York: Demos; 1990:197–243.
Kwan P, Brodie MJ: Early identification of refractory epilepsy. N Engl J Med 2000, 342:314–319. This review provides an update on medical response in patients with epilepsy, and emphasizes the predictive value of the initial antiepileptic drug therapy.
Wiebe S, Blume WT, Girvin JP, Eliasziw M: A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 2001, 5:311–318. This is a prospective randomized controlled trial that established the efficacy and safety of epilepsy surgery for temporal lobe epilepsy.
Radhakrishnan K, So EL, Silbert PL, et al.: Predictors of outcome of anterior temporal lobectomy for intractable epilepsy: a multivariate study. Neurology 1998, 51:465–471.
Cascino GD, Trenerry MR, So E, et al.: Routine EEG and temporal lobe epilepsy: relation to long-term EEG monitoring, quantitative MRI, and operative outcome. Epilepsia 1996, 37:651–656.
Cambier DM, Cascino GD, So EL, Marsh WR: Video-EEG monitoring in patients with hippocampal atrophy. Acta Neurol Scan 2001, 103:1–7.
Mosewich RK, So EL, O’Brien TJ, et al.: Factors predictive of the outcome of frontal lobe epilepsy surgery. Epilepsia 2000, 41:843–849. This is a fine study on outcome after surgical treatment for extratemporal epilepsy.
Cascino GD: Advances in neuroimaging: surgical localization. Epilepsia 2001, 42:3–12.
Cascino GD, Jack CR, Jr., Parisi JE, et al.: MRI in the presurgical evaluation of patients with frontal lobe epilepsy and children with temporal lobe epilepsy: pathological correlation and prognostic importance. Epilepsy Res 1992, 11:51–59.
O’Brien TJ, So EL, Mullan BP, et al.: Subtraction ictal SPECT co-registered to MRI improves clinical usefulness of SPECT in localizing the surgical seizure focus. Neurology 1998, 50:445–454. Discusses the introduction of SISCOM as a preoperative neuroimaging procedure for peri-ictal imaging.
O’Brien TJ, O’Connor MK, Mullan BP, et al.: Subtraction ictal SPECT co-registered to MRI in partial epilepsy: description and technical validation of the method with phantom and patients studies. Nucl Med Commun 1998, 19:31–45.
So EL: Integration of EEG, MRI and SPECT in localizing the seizure focus for epilepsy surgery. Epilepsia 2000, 41(suppl):S48-S54.
Brinkmann BH, O’Brien TJ, Webster DB, et al.: Voxel significance mapping using local image variances in subtraction ictal SPET. Nucl Med Commun 2000, 21:545–551.
O’Brien TJ, Brinkmann BH, Mullan BP, et al.: Comparative study of 99mTc-ECD and 99mTc-HMPAO for SPECT: qualitative and quantitative analysis. J Neurol Neurosurg Psychiatry 1999, 66:331–339.
So EL, O’Brien TJ, Brinkmann BH, et al.: The EEG evaluation of single photon emission computed tomography abnormalities in epilepsy. J Clin Neurophysiol 2000, 17:10–28.
O’Brien TJ, So EL, Mullan BP, et al.: Subtraction periictal SPECT is predictive of extratemporal epilepsy surgery outcome. Neurology 2000, 55:1668–1677. A study of SISCOM in patients undergoing surgery for extratemporal epilepsy.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cascino, G.D. Surgical treatment for extratemporal epilepsy. Curr Treat Options Neurol 6, 257–262 (2004). https://doi.org/10.1007/s11940-004-0017-4
Issue Date:
DOI: https://doi.org/10.1007/s11940-004-0017-4