Opinion statement
With the recent increase in complex coronary interventions including percutaneous coronary intervention (PCI) for chronic total occlusions and complex higher risk (and indicated) patients, the spectrum of potential periprocedural complications and their prompt management has become even more relevant. Vascular access-related problems remain the most prevalent of all PCI complications and with randomized controlled trial data from over 20,000 patients supporting the superiority of radial over femoral access in reducing bleeding and vascular complications, a default radial strategy should be promoted. The European Society of Cardiology guidelines have acknowledged this by giving a class 1 (level of evidence: A) recommendation for a radial approach for PCI. The US society guidelines, however, have thus far lagged behind. Each individual patient undergoing a PCI should be risk-stratified objectively using available risk prediction models based on patient comorbidities and anatomical and procedural complexities. Customized informed consent should therefore be provided to all patients and should include the potential risks from radiation injury. Here, we review the current data related to common periprocedural complications related to PCI.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation. 2007;115(20):2666–74. doi:10.1161/circulationaha.106.681973.
Petersen JCM, Insua JJV. Pseudoaneurysm after transradial coronary angiography. New England Journal of Medicine N Engl J Med. 2015;373(14):1361–1. doi:10.1056/nejmicm1406093.
Babunashvili AM, Pancholy SB, Kartashov DS. New technique for treatment of postcatheterization radial artery pseudoaneurysm. Catheter Cardiovasc Interv. 2016. doi:10.1002/ccd.26717.
Kent K, Mcardle CR, Kennedy B, Baim DS, Anninos E, Skillman JJ. A prospective study of the clinical outcome of femoral pseudoaneurysms and arteriovenous fistulas induced by arterial puncture. J Vasc Surg. 1993;17(1):125–33. doi:10.1016/0741-5214(93)90016-f.
Toursarkissian B, Allen BT, Petrinec D, et al. Spontaneous closure of selected iatrogenic pseudoaneurysms and arteriovenous fistulae. J Vasc Surg. 1997;25(5):803–9. doi:10.1016/s0741-5214(97)70209-x.
Dzijan-Horn M, Langwieser N, Groha P, et al. Safety and efficacy of a potential treatment algorithm by using manual compression repair and ultrasound-guided thrombin injection for the management of iatrogenic femoral artery pseudoaneurysm in a large patient cohort. Circ Cardiovasc Interv. 2014;7(2):207–15. doi:10.1161/circinterventions.113.000836.
Cauchi MP, Robb PM, Zemple RP, Ball TC. Radial artery pseudoaneurysm: a simplified treatment method. J Ultrasound Med. 2014;33(8):1505–9. doi:10.7863/ultra.33.8.1505.
Collins N, Wainstein R, Ward M, Bhagwandeen R, Dzavik V. Pseudoaneurysm after transradial cardiac catheterization: case series and review of the literature. Catheter Cardiovasc Interv. 2011;80(2):283–7. doi:10.1002/ccd.23216.
Mogi S, Maekawa Y, Fukuda K, Noma S. Retroperitoneal bleeding and arteriovenous fistula after percutaneous coronary intervention successfully treated with intravascular ultrasound-guided covered stent implantation. Intern Med. 2016;55(11):1467–9. doi:10.2169/internalmedicine.55.6134.
Trimarchi S, Smith DE, Share D, et al. Retroperitoneal hematoma after percutaneous coronary intervention: prevalence, risk factors, management, outcomes, and predictors of mortality. J Am Coll Cardiol Intv. 2010;3(8):845–50. doi:10.1016/j.jcin.2010.05.013.
Kelm M, Perings SM, Jax T, et al. Incidence and clinical outcome of iatrogenic femoral arteriovenous fistulas. J Am Coll Cardiol. 2002;40(2):291–7. doi:10.1016/s0735-1097(02)01966-6.
Na KJ, Kim MA, Moon HJ, Lee JS, Choi J-S. Radial arteriovenous fistula developed late after coronary angiography: a case report. Korean J Thorac Cardiovasc Surg. 2012;45(6):421–3. doi:10.5090/kjtcs.2012.45.6.421.
Seto AH, Abu-Fadel MS, Sparling JM, et al. Real-time ultrasound guidance facilitates femoral arterial access and reduces vascular complications. J Am Coll Cardiol Intv. 2010;3(7):751–8. doi:10.1016/j.jcin.2010.04.015.
Seto AH, Roberts JS, Abu-Fadel MS, et al. Real-time ultrasound guidance facilitates transradial access. J Am Coll Cardiol Intv. 2015;8(2):283–91. doi:10.1016/j.jcin.2014.05.036.
Dauerman HL, Rao SV, Resnic FS, Applegate RJ. Bleeding avoidance strategies. J Am Coll Cardiol. 2011;58(1):1–10. doi:10.1016/j.jacc.2011.02.039.
Applegate RJ, Sacrinty MT, Kutcher MA, et al. Trends in vascular complications after diagnostic cardiac catheterization and percutaneous coronary intervention via the femoral artery, 1998 to 2007. J Am Coll Cardiol Intv. 2008;1(3):317–26. doi:10.1016/j.jcin.2008.03.013.
Doyle BJ, Ting HH, Bell MR, et al. Major femoral bleeding complications after percutaneous coronary intervention. J Am Coll Cardiol Intv. 2008;1(2):202–9. doi:10.1016/j.jcin.2007.12.006.
Ratib K, Mamas MA, Anderson SG, et al. Access site practice and procedural outcomes in relation to clinical presentation in 439,947 patients undergoing percutaneous coronary intervention in the United Kingdom. J Am Coll Cardiol Intv. 2015;8(1):20–9. doi:10.1016/j.jcin.2014.06.026.
Ferrante G, Rao SV, Jüni P, et al. Radial versus femoral access for coronary interventions across the entire spectrum of patients with coronary artery disease. J Am Coll Cardiol Intv. 2016;9(14):1419–34. doi:10.1016/j.jcin.2016.04.014.
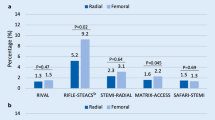
•• Bernat I, Horak D, Stasek J, et al. ST-segment elevation myocardial infarction treated by radial or femoral approach in a multicenter randomized clinical trial. J Am Coll Cardiol. 2014;63(10):964–72. doi:10.1016/j.jacc.2013.08.1651. The STEMI-RADIAL randomized multicenter trial compared both radial and femoral access outcomes in STEMI patients at high-volume centers. Radial use was associated with less major bleeding and access-related complications when compared to the femoral approach.
Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome. J Am Coll Cardiol. 2012;60(24):2481–9. doi:10.1016/j.jacc.2012.06.017.
Wagener JF, Rao SV. Radial artery occlusion after transradial approach to cardiac catheterization. Current Atherosclerosis Reports. 2015;17(3). doi:10.1007/s11883-015-0489-6.
Rashid M, Kwok CS, Pancholy S, et al. Radial artery occlusion after transradial interventions: a systematic review and meta‐analysis. J Am Heart Assoc Journal of the American Heart Association. 2016;5(1). doi:10.1161/jaha.115.002686.
Rao SV, Tremmel JA, Gilchrist IC, et al. Best practices for transradial angiography and intervention: a consensus statement from the society for cardiovascular angiography and intervention’s transradial working group. Catheter Cardiovasc Interv. 2013;83(2):228–36. doi:10.1002/ccd.25209.
Dharma S, Kedev S, Patel T, Kiemeneij F, Gilchrist IC. A novel approach to reduce radial artery occlusion after transradial catheterization: postprocedural/prehemostasis intra-arterial nitroglycerin. Catheter Cardiovasc Interv. 2014;85(5):818–25. doi:10.1002/ccd.25661.
Pancholy SB, Bernat I, Bertrand OF, Patel TM. Prevention of radial artery occlusion after transradial catheterization. J Am Coll Cardiol Intv. 2016;9(19):1992–9. doi:10.1016/j.jcin.2016.07.020.
Bernat I, Bertrand OF, Rokyta R, et al. Efficacy and safety of transient ulnar artery compression to recanalize acute radial artery occlusion after transradial catheterization. Am J Cardiol. 2011;107(11):1698–701. doi:10.1016/j.amjcard.2011.01.056.
Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115(17):2344–51. doi:10.1161/CIRCULATIONAHA.106.685313.
Kedhi E, Joesoef KS, Mcfadden E, et al. Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice (COMPARE): a randomised trial. Lancet. 2010;375(9710):201–9. doi:10.1016/s0140-6736(09)62127-9.
Serruys PW, Silber S, Garg S, et al. Comparison of zotarolimus-eluting and everolimus-eluting coronary stents. N Engl J Med. 2010;363(2):136–46. doi:10.1056/nejmoa1004130.
D’ascenzo F, Bollati M, Clementi F, et al. Incidence and predictors of coronary stent thrombosis: evidence from an international collaborative meta-analysis including 30 studies, 221,066 patients, and 4276 thromboses. Int J Cardiol. 2013;167(2):575–84. doi:10.1016/j.ijcard.2012.01.080.
Cutlip DE, Kereiakes DJ, Mauri L, Stoler R, Dauerman HL. Thrombotic complications associated with early and late nonadherence to dual antiplatelet therapy. J Am Coll Cardiol Intv. 2015;8(3):404–10. doi:10.1016/j.jcin.2014.10.017.
Stone GW, Witzenbichler B, Guagliumi G, et al. Bivalirudin during primary PCI in acute myocardial infarction. N Engl J Med. 2008;358(21):2218–30. doi:10.1056/nejmoa0708191.
Steg PG, Hof AV’t, Hamm CW, et al. Bivalirudin started during emergency transport for primary PCI. N Engl J Med. 2013;369(23):2207–17. doi:10.1056/nejmoa1311096.
Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. Circulation. 2015;133(11):1135–47. doi:10.1161/cir.0000000000000336.
Waldo SW, Armstrong EJ, Yeo K-K, et al. Procedural success and long-term outcomes of aspiration thrombectomy for the treatment of stent thrombosis. Catheter Cardiovasc Interv. 2013;82(7):1048–53. doi:10.1002/ccd.25007.
Lipinski MJ, Escarcega RO, Baker NC, et al. Scaffold thrombosis after percutaneous coronary intervention with absorb bioresorbable vascular scaffold. J Am Coll Cardiol Intv. 2016;9(1):12–24. doi:10.1016/j.jcin.2015.09.024.
Colombo A, Ruparelia N. Who is thrombogenic: the scaffold or the doctor? back to the future! J Am Coll Cardiol Intv. 2016;9(1):25–7. doi:10.1016/j.jcin.2015.09.021.
Felix CM, Fam JM, Diletti R, et al. Mid- to long-term clinical outcomes of patients treated with the everolimus-eluting bioresorbable vascular scaffold. J Am Coll Cardiol Intv. 2016;9(16):1652–63. doi:10.1016/j.jcin.2016.04.035.
Attizzani GF, Capodanno D, Ohno Y, Tamburino C. Mechanisms, pathophysiology, and clinical aspects of incomplete stent apposition. J Am Coll Cardiol. 2014;63(14):1355–67. doi:10.1016/j.jacc.2014.01.019.
Hassan AKM, Bergheanu SC, Stijnen T, et al. Late stent malapposition risk is higher after drug-eluting stent compared with bare-metal stent implantation and associates with late stent thrombosis. Eur Heart J. 2009;31(10):1172–80. doi:10.1093/eurheartj/ehn553.
Kan J, Ge Z, Zhang J-J, et al. Incidence and clinical outcomes of stent fractures on the basis of 6,555 patients and 16,482 drug-eluting stents from 4 centers. J Am Coll Cardiol Intv. 2016;9(11):1115–23. doi:10.1016/j.jcin.2016.02.025.
Lee SE, Jeong MH, Kim IS, et al. Clinical outcomes and optimal treatment for stent fracture after drug-eluting stent implantation. J Cardiol. 2009;53(3):422–8. doi:10.1016/j.jjcc.2009.02.010.
•• Claessen BE, Henriques JPS, Jaffer FA, et al. Stent thrombosis. J Am Coll Cardiol Intv. 2014;7(10):1081–92. doi:10.1016/j.jcin.2014.05.016. This thorough review of stent thrombosis describes the pathophysiology and possible predictors of this complication. Claessen et al. provide etiology-directed treatment strategies for several complications that result in stent thrombosis including stent fracture, malapposition, and underexpansion.
Devidutta S, Yeo KK. Acute stent thrombosis due to stent underexpansion managed with rotational atherectomy. Cardiovasc Revasc Med. 2016;17(1):66–70. doi:10.1016/j.carrev.2015.10.003.
Huber MS, Mooney JF, Madison J, Mooney MR. Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol. 1991;68(5):467–71. doi:10.1016/0002-9149(91)90780-o.
Holmes DR, Holubkov R, Vlietstra RE, et al. Comparison of complications during percutaneous transluminal coronary angioplasty from 1977 to 1981 and from 1985 to 1986: The National Heart, Lung, and Blood Institute Percutaneous Transluminal Coronary Angioplasty Registry. J Am Coll Cardiol. 1988;12(5):1149–55. doi:10.1016/0735-1097(88)92593-4.
Furukawa MK, Domingues CEM, Almeida MCVD, Jr VRF, Jr DS. Use of tandem stents for treatment of helicoidal dissection of the right coronary artery. Arq Bras Cardiol Arquivos Brasileiros de Cardiologia. 2000;74(6). doi:10.1590/s0066-782x2000000600004.
Chamié D, Bezerra HG, Attizzani GF, et al. Incidence, predictors, morphological characteristics, and clinical outcomes of stent edge dissections detected by optical coherence tomography. J Am Coll Cardiol Intv. 2013;6(8):800–13. doi:10.1016/j.jcin.2013.03.019.
Dunning DW, Kahn JK, Hawkins ET, O’neill WW. Iatrogenic coronary artery dissections extending into and involving the aortic root. Catheter Cardiovasc Interv. 2000;51(4):387–93. doi:10.1002/1522-726x(200012)51:4<387::aid-ccd3>3.3.co;2-2.
Ellis SG, Ajluni S, Arnold AZ, et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994;90(6):2725–30. doi:10.1161/01.cir.90.6.2725.
Fasseas P, Orford JL, Panetta CJ, et al. Incidence, correlates, management, and clinical outcome of coronary perforation: analysis of 16,298 procedures. Am Heart J. 2004;147(1):140–5. doi:10.1016/s0002-8703(03)00505-2.
Fejka M, Dixon SR, Safian RD, et al. Diagnosis, management, and clinical outcome of cardiac tamponade complicating percutaneous coronary intervention. Am J Cardiol. 2002;90(11):1183–6. doi:10.1016/s0002-9149(02)02831-x.
Eeckhout E, De Palma R. Coronary perforation. JACC: Cardiovascular Interventions. 2013;6(8):800–813. 2011;4(1):96–97. doi:10.1016/j.jcin.2010.09.021
Chowdhury MA, Sheikh MA. Coronary bypass graft perforation during percutaneous intervention. Cardiovasc Revasc Med. 2016;17(1):48–53. doi:10.1016/j.carrev.2015.11.004.
Antoniucci D. Put Off Till Tomorrow What You Can Do Today. J Am Coll Cardiol. 2014;63(20):2099–100. doi:10.1016/j.jacc.2014.01.056.
Jaffe R, Dick A, Strauss BH. Prevention and treatment of microvascular obstruction-related myocardial injury and coronary no-reflow following percutaneous coronary intervention. J Am Coll Cardiol Intv. 2010;3(7):695–704. doi:10.1016/j.jcin.2010.05.004.
Sardella G, Mancone M, Bucciarelli-Ducci C, et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size. J Am Coll Cardiol. 2009;53(4):309–15. doi:10.1016/j.jacc.2008.10.017.
Stone GW. Distal microcirculatory protection during percutaneous coronary intervention in acute ST- segment elevation myocardial infarction: a randomized controlled trial. JAMA. 2005;293(9):1063. doi:10.1001/jama.293.9.1063.
O’gara PT, Kushner FG, Ascheim DD, et al. ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;2012:127(4). doi:10.1161/cir.0b013e3182742cf6.
Bushberg JT. The essential physics of medical imaging. Philadelphia: Lippincott Williams & Wilkins; 2002.
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation. 2007;116(11):1290–305. doi:10.1161/CIRCULATIONAHA.107.688101.
Chambers CE, Fetterly KA, Holzer R, et al. Radiation safety program for the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 2011;77(4):546–56. doi:10.1002/ccd.22867.
Stewart F, Akleyev A, Hauer-Jensen M, et al. ICRP PUBLICATION 118: ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs—threshold doses for tissue reactions in a radiation protection context. Ann ICRP. 2012;41(1–2):1–322. doi:10.1016/j.icrp.2012.02.001.
Agarwal S, Parashar A, Ellis SG, et al. Measures to reduce radiation in a modern cardiac catheterization laboratory. Circ Cardiovasc Interv. 2014;7(4):447–55. doi:10.1161/CIRCINTERVENTIONS.114.001499. Agarwal and colleagues showed that by decreasing the default fluoroscopic frame rate to 7.5 frames per second from 10, total air kerma and air kerma rates can be reduced in the modern catheterization lab.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Coronary Artery Disease
Rights and permissions
About this article
Cite this article
Means, G., End, C. & Kaul, P. Management of Percutaneous Coronary Intervention Complications. Curr Treat Options Cardio Med 19, 25 (2017). https://doi.org/10.1007/s11936-017-0526-6
Published:
DOI: https://doi.org/10.1007/s11936-017-0526-6