Opinion statement
Left ventricular thrombus (LVT) is a frequent complication in patients with acute anterior myocardial infarction (MI) and in those with dilated cardiomyopathy (DCM). The clinical importance of LVT lies in its potential to embolize. The current treatment of patients with acute MI centers on reperfusion, and although controversial, the incidence of LVT complicating acute anterior MI is probably reduced when compared with historical controls. Nevertheless, stroke continues to be a clinically important complication of acute MI and is most common in patients with anterior MI, in part secondary to embolization of LVT. Therapeutic anticoagulation during acute MI reduces the incidence of LVT, and long-term anticoagulation has been associated with a reduction in recurrent infarction and ischemic stroke, but carries hemorrhagic risk. Primary treatment strategies for patients with acute MI center on reperfusion therapy followed by antiplatelet agents and pharmacologic blockade of abnormal neurohumoral mechanisms. Strategies to prevent stroke following infarction include risk stratification for development of LVT and embolism. For patients with anterior MI, particularly those with apical akinesis or dyskinesis, therapeutic anticoagulation reduces the number of LVT and cardioembolic strokes. However, the absolute number of ischemic strokes prevented with this strategy may only be marginal, given the anticoagulation risk, particularly if antiplatelet agents are used concurrently. An attractive alternative strategy is echocardiographic evaluation following anterior infarction with therapeutic anticoagulation reserved for those with demonstrable thrombus. The efficacy of this strategy, however, never has been proven in a clinical study. Primary prevention of cardioembolic stroke through therapeutic anticoagulation is controversial in patients with DCM; the greatest benefit would be expected for those with severe left ventricular dysfunction. If LVT is detected during the course of MI or DCM, therapeutic anticoagulation is usually indicated with the expectation that the majority of thrombi will resolve without clinical evidence of systemic embolism. Additional therapeutic intervention is rarely needed.
Similar content being viewed by others
References and Recommended Reading
van Dantzig JM, Delemarre BJ, Bot H, et al.: Left ventricular thrombus in acute myocardial infarction. Eur Heart J 1996, 17:1640–1645.
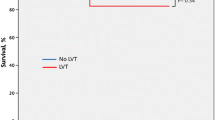
Keren A, Goldberg S, Gottlieb S, et al.: Natural history of left ventricular thrombi: their appearance and resolution in the posthospitalization period of acute myocardial infarction. J Am Coll Cardiol 1990, 15:790–800. The authors describe the natural history of LVT following acute MI in 198 consecutive patients, 34 of whom received thrombolytic therapy. This large series of patients was prospectively followed with echocardiography for an average of 2 years following infarction. Anterior infarction, ejection fraction less than or equal to 35%, and apical dyskinesis were predictive of LVT development. Nearly half of the patients with thrombus had resolution of thrombus 6 months after infarction. Resolution of thrombus was associated with akinesia rather than dyskinesia at hospital discharge and warfarin treatment. LVT developed after discharge in about 10% of patients and was related to deterioration in left ventricular function, ejection fraction less than or equal to 35% before discharge, and ventricular aneurysm or dyskinesia. These observations have established the natural history of LVT and provide the rational for anticoagulation therapy recommendations.
Vaitkus PT, Barnathan ES: Embolic potential, prevention and management of mural-thrombus complicating anterior myocardial infarction: a metaanalysis. J Am Coll Cardiol 1993, 22:1004–1009.
Roberts WC, Siegal RJ, McManus BM: Idiopathic dilated cardiomyopathy: analysis of 152 necropsy patients. Am J Cardiol. 1987, 60:1340–55.
Tanne D, Gottlieb S, Hod H, et al.: Incidence and mortality from early stroke associated with acute myocardial infarction in the prethrombolytic and thrombolytic eras. J Am Coll Cardiol 1997, 30:1484–1490.
Chiarella FC, Santoro E, Domenicucci S, et al.: Predischarge two-dimensional echocardiographic evaluation of left ventricular thrombosis after acute myocardial infarction in the GISSI-3 Study. Am J Cardiol 1998, 81:822–827.
Pizzetti G, Belotti G, Margonato A, et al.: Thrombolytic therapy reduces the incidence of left ventricular thrombus after anterior myocardial infarction relationship to vessel patency and infarct size. Eur Heart J 1996, 17:421–428.
Ryan TJ, Antman EM, Brooks NH, et al.: 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol 1999, 34:890–911. This committee recommends a conservative anticoagulation approach to the prevention of stroke, presumably due to embolism of LVT, following acute MI. The authors reserve long-term anticoagulation to patients with documented LVT complicating acute MI.
Cairns JA, Theroux P, Lewis HD Jr, et al.: Antithrombotic agents in coronary artery disease. Chest 1998, 114:611S-633S. This Consensus Panel on Antithrombotic Therapy of the ACCP recommends a more aggressive approach to anticoagulation following acute MI that than of the ACC/AHA guidelines. Anticoagulation is recommended for those with large anterior infarction, apical akinesis or dyskinesis, and moderate or worse left ventricular dysfunction.
Smith P: Long-term anticoagulant treatment after acute myocardial infarction: the warfarin re-infarction study. Ann Epidemiol 1992, 2:549–552.
Anticoagulants in the secondary prevention of events in coronary thrombosis (ASPECT) research group: Effect of long-term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction. Lancet 1994, 343:499–503.
Fihn SD, Callahan CM, Martin DC, et al.: The risk for and severity of bleeding complications in elderly patients treated with warfarin. Ann Intern Med. 1996, 124:970–979.
Koniaris LS, Goldhaber SZ: Anticoagulation in dilated cardiomyopathy. J Am Coll Cardiol 1998, 31:745–748.
Turpie AG, Robinson JG, Doyle DJ, et al.: Comparison of high-dose with low-dose subcutaneous heparin to prevent left ventricular mural thrombosis in patients with acute transmural anterior myocardial infarction. N Engl J Med 1989, 320:352–357.
Randomized controlled trial of subcutaneous calcium-heparin in acute myocardial infarction. The SCATI (Studio Sulla Calciparina Nell’Angina E Nella Trombosi Ventricolare Nell’Infarto) Group. Lancet 1989:182-186.
Kontny F, Dale J, Abildgaard U, et al.: Randomized trial of low molecular weight heparin (dalteparin) in prevention of left ventricular thrombus formation and arterial embolism after acute anterior myocardial infarction: the Fragmin in Acute Myocardial Infarction (FRAMI) study. J Am Coll Cardiol 1997, 30:962–969.
Delemarre BJ, Visser CA, Bot H, et al.: Prediction of apical thrombus formation in acute myocardial infarction based on left ventricular spatial flow patter. J Am Coll Cardiol 1990, 15:355–360.
Yamamoto K, Ikeda U, Furuhashi K, et al.: The coagulation system is activated in idiopathic cardiomyopathy. J Am Coll Cardiol 1995, 25:1634–1640.
Manning WJ, Leeman DE, Gotch PJ, et al.: Pulsed Doppler evaluation of atrial mechanical function after electrical cardioversion of atrial fibrillation. J Am Coll Cardiol 1989, 13:617–623.
Fatkin D, Kelly RP, Feneley MP: Relations between left atrial appendage blood flow velocity, spontaneous echocardiographic contrast and thromboembolic risk in vivo. J Am Coll Cardiol 1994, 23:961–969.
Asinger RW, Mikell FL, Elsperger KJ, et al.: Serial changes in left ventricular wall motion by two-dimensional echocardiography following anterior infarction. Am Heart J 1988, 116:50–58.
Falk RH, Foster E, Coats MH: Ventricular thrombi and thromboembolism in dilated cardiomyopathy: a prospective follow-up study. Am Heart J 1992, 123:136–142.
Haugland JM, Asinger RW, Mikell Fl, et al.: Embolic potential of left ventricular thrombi detected by two-dimensional echocardiography. Circulation 1984: 70:588–598.
Stratton JR, Lighty GW Jr, Pearlman AS, et al.: Detection of left ventricular thrombus by two-dimensional echocardiography: sensitivity, specificity and causes of uncertainty. Circulation 1982, 66:156–166.
Asinger RW, Mikell FL, Sharma B, et al.: Observations on detecting left ventricular thrombus with two dimensional echocardiography: emphasis on avoidance of false positive diagnoses. Am J Cardiol 1981, 47:145–156.
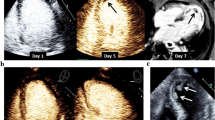
Mikell FL, Asinger RW, Elsperger KJ, et al.: Regional stasis of blood in the dysfunctional left ventricle: echocardiographic detection and differentiation from early thrombosis. Circulation 1982, 66:755–763.
Chen C, Koschyk D, Hamm C, et al.: Usefulness of transesophageal echocardiography in identifying small left ventricular apical thrombus. J Am Coll Cardiol 1993, 21:208–215.
Ezekowitz MD, Wilson DA, Smith EO, et al.: Comparison of indium-111 platelet scintigraphy and twodimensional echocardiography in the diagnosis of left ventricular thrombi. N Engl J Med 1982, 306:1509–1513.
Sechtem U, Theissen P, Heindel W, et al.: Diagnosis of left ventricular thrombi by magnetic resonance imaging and comparison with angiocardiography, computed tomography and echocardiography. Am J Cardiol 1989, 64:1195–1200.
Reeder GS, Lengyel M, Tajik AJ, et al.: Mural thrombus in left ventricular aneurysm: incidence, role of angiography and relation between anticoagulation and embolization. Mayo Clin Proc 1981, 56:77–81.
Kontny F, Dale J, Abildgaard U, et al.: Adverse effect of warfarin in acute myocardial infarction: increased left ventricular thrombus formation in patients not treated with high-dose heparin. Eur Heart J 1993, 14:1040–1043.
Schomig A, Neumann FJ, Kastrati A, et al.: A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary artery stents. N Engl J Med 1996, 334:1084–1089.
Coumadin Aspirin Reinfarction Study (CARS) Investigators. Randomized double-blind trial of fixed low-dose warfarin with aspirin after myocardial infarction. Lancet 1997, 350:389–396.
Kremer P, Fiebig R, Tilsner V, et al.: Lysis of left ventricular thrombi with urokinase. Circulation 1985, 72:112–118.
Kouvaras G, Chronopoulos G, Soufras G, et al.: The effects of long-term antithrombotic treatment on left ventricular thrombi in patients after an acute myocardial infarction. Am Heart J 1990, 119:73–78.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Stokman, P.J., Nandra, C.S. & Asinger, R.W. Left ventricular thrombus. Curr Treat Options Cardio Med 3, 515–521 (2001). https://doi.org/10.1007/s11936-001-0025-6
Issue Date:
DOI: https://doi.org/10.1007/s11936-001-0025-6