Abstract
Purpose of Review
To summarize recent investigation into associations between the genitourinary microbiota and prostatic disease.
Recent Findings
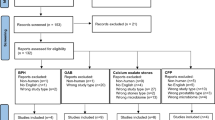
The genitourinary tract is not sterile. There are microbial communities (microbiota) in each niche of the genitourinary tract including the bladder, prostate, and urethra, which have been the subject of increasing scientific interest. Investigators have utilized several unique methods to study them, resulting in a highly heterogeneous body of literature. To characterize these genitourinary microbiota, diverse clinical specimens have been analyzed, including urine obtained by various techniques, seminal fluid, expressed prostatic secretions, and prostatic tissue. Recent studies have attempted to associate the microbiota detected from these samples with urologic disease and have implicated the genitourinary microbiota in many common conditions, including benign prostatic hyperplasia (BPH), prostate cancer, and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
Summary
In this review, we summarize the recent literature pertaining to the genitourinary microbiota and its relationship to the pathophysiology and management of three common prostatic conditions: BPH, prostate cancer, and CP/CPPS.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hollingsworth JM, Wei JT. Economic impact of surgical intervention in the treatment of benign prostatic hyperplasia. Rev Urol. 2006;8(Suppl 3):S9–S15.
Auffenberg GB, Helfand BT, McVary KT. Established medical therapy for benign prostatic hyperplasia. Urol Clin North Am. 2009;36:443–59.
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (1999–2015). 2018. Available at: www.cdc.gov/cancer/dataviz. Accessed 16 Mar 2019.
Bowen DK, Dielubanza E, Schaeffer AJ. Chronic bacterial prostatitis and chronic pelvic pain syndrome. BMJ Clin Evid. 2015;2015:1802.
Ficarra V, Rossanese M, Zazzara M, Giannarini G, Abbinante M, Bartoletti R, et al. The role of inflammation in lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH) and its potential impact on medical therapy. Curr Urol Rep. 2014;15:463.
Gandaglia G, Zaffuto E, Fossati N, Cucchiara V, Mirone V, Montorsi F, et al. The role of prostatic inflammation in the development and progression of benign and malignant diseases. Curr Opin Urol. 2017;27:99–106.
•• Shrestha E, White JR, Yu SH, Kulac I, Ertunc O, de Marzo AM, et al. Profiling the urinary microbiome in men with positive versus negative biopsies for prostate cancer. J Urol. 2018;199:161–71 A recent study demonstrating increase in uropathogenic bacteria in cancerous prostate tissue. This study leads to additional hypotheses regarding the nature of bacterial inflammation as a determinant of prostate cancer.
Sfanos KS, Isaacs WB, De Marzo AM. Infections and inflammation in prostate cancer. Am J Clin Exp Urol. 2013;1:3–11.
De Marzo AM, et al. Inflammation in prostate carcinogenesis. Nat Rev Cancer. 2007;7:256–69.
Sfanos KS, De Marzo AM. Prostate cancer and inflammation: the evidence. Histopathology. 2012;60:199–215.
Sfanos KS, Yegnasubramanian S, Nelson WG, De Marzo AM. The inflammatory microenvironment and microbiome in prostate cancer development. Nat Rev Urol. 2018;15:11–24.
Mani RS, Amin MA, Li X, Kalyana-Sundaram S, Veeneman BA, Wang L, et al. Inflammation-induced oxidative stress mediates gene fusion formation in prostate cancer. Cell Rep. 2016;17:2620–31.
Sfanos KS, Joshu CE. IBD as a risk factor for prostate cancer: what is the link? Nat Rev Urol. 2019. https://doi.org/10.1038/s41585-019-0157-7.
Massari F, Mollica V, di Nunno V, Gatto L, Santoni M, Scarpelli M, et al. The human microbiota and prostate cancer: friend or foe? Cancers (Basel). 2019;11(4):E459. https://doi.org/10.3390/cancers11040459
Nickel JC, et al. Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls. J Urol. 2003;170:818–22.
Breser ML, Salazar FC, Rivero VE, Motrich RD. Immunological mechanisms underlying chronic pelvic pain and prostate inflammation in chronic pelvic pain syndrome. Front Immunol. 2017;8:898.
Porter CM, Shrestha E, Peiffer LB, Sfanos KS. The microbiome in prostate inflammation and prostate cancer. Prostate Cancer Prostatic Dis. 2018;21:345–54.
Flint HJ, Scott KP, Louis P, Duncan SH. The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol. 2012;9:577–89.
Frank DN, Zhu W, Sartor RB, Li E. Investigating the biological and clinical significance of human dysbioses. Trends Microbiol. 2011;19:427–34.
Gajer P, et al. Temporal dynamics of the human vaginal microbiota. Sci Transl Med. 2012;4:132ra52.
Hilt EE, McKinley K, Pearce MM, Rosenfeld AB, Zilliox MJ, Mueller ER, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol. 2014;52:871–6.
Brubaker L, Nager CW, Richter HE, Visco A, Nygaard I, Barber MD, et al. Urinary bacteria in adult women with urgency urinary incontinence. Int Urogynecol J. 2014;25:1179–84.
Pearce MM, Hilt EE, Rosenfeld AB, Zilliox MJ, Thomas-White K, Fok C, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. MBio. 2014;5:e01283–14.
Wolfe AJ, Toh E, Shibata N, Rong R, Kenton K, FitzGerald M, et al. Evidence of uncultivated bacteria in the adult female bladder. J Clin Microbiol. 2012;50:1376–83.
Nienhouse V, Gao X, Dong Q, Nelson DE, Toh E, McKinley K, et al. Interplay between bladder microbiota and urinary antimicrobial peptides: mechanisms for human urinary tract infection risk and symptom severity. PLoS One. 2014;9:e114185.
•• Bajic P, van Kuiken ME, Burge BK, Kirshenbaum EJ, Joyce CJ, Wolfe AJ, et al. Male bladder microbiome relates to lower urinary tract symptoms. Eur Urol Focus. 2018. https://doi.org/10.1016/j.euf.2018.08.001 This study is the first study to demonstrate an association between the urinary microbiome in men and lower urinary tract symptoms. Also important in establishing the difference between voided and catheterized urine collection in men. It lays groundwork for additional investigation in the the male urinary microbiome.
Khasriya R, Sathiananthamoorthy S, Ismail S, Kelsey M, Wilson M, Rohn JL, et al. Spectrum of bacterial colonization associated with urothelial cells from patients with chronic lower urinary tract symptoms. J Clin Microbiol. 2013;51:2054–62.
Fouts DE, Pieper R, Szpakowski S, Pohl H, Knoblach S, Suh MJ, et al. Integrated next-generation sequencing of 16S rDNA and metaproteomics differentiate the healthy urine microbiome from asymptomatic bacteriuria in neuropathic bladder associated with spinal cord injury. J Transl Med. 2012;10:174.
Karstens L, et al. Does the urinary microbiome play a role in urgency urinary incontinence and its severity? Front Cell Infect Microbiol. 2016;6:78.
Brubaker L, Wolfe A. The urinary microbiota: a paradigm shift for bladder disorders? Curr Opin Obstet Gynecol. 2016;28:407–12.
Brubaker L, Wolfe AJ. The female urinary microbiota, urinary health and common urinary disorders. Ann Transl Med. 2017;5:34.
Pearce MM, et al. The female urinary microbiome in urgency urinary incontinence. Am J Obstet Gynecol. 2015;213(347):e1–11.
• Price TK, Dune T, Hilt EE, Thomas-White KJ, Kliethermes S, Brincat C, et al. The clinical urine culture: enhanced techniques improve detection of clinically relevant microorganisms. J Clin Microbiol. 2016;54:1216–22 This study further expands our knowledge of urine culture protocols and the expanded quantitative urine culture (EQUC) to identify and isolate live bacteria that would not otherwise be detected by standard clinical cultures.
Thomas-White KJ, Hilt EE, Fok C, Pearce MM, Mueller ER, Kliethermes S, et al. Incontinence medication response relates to the female urinary microbiota. Int Urogynecol J. 2016;27:723–33.
Nelson DE, Dong Q, van der Pol B, Toh E, Fan B, Katz BP, et al. Bacterial communities of the coronal sulcus and distal urethra of adolescent males. PLoS One. 2012;7:e36298.
Dong Q, Nelson DE, Toh E, Diao L, Gao X, Fortenberry JD, et al. The microbial communities in male first catch urine are highly similar to those in paired urethral swab specimens. PLoS One. 2011;6:e19709.
Nelson DE, van der Pol B, Dong Q, Revanna KV, Fan B, Easwaran S, et al. Characteristic male urine microbiomes associate with asymptomatic sexually transmitted infection. PLoS One. 2010;5:e14116.
Nickel JC, Stephens A, Landis JR, Chen J, Mullins C, van Bokhoven A, et al. Search for microorganisms in men with urologic chronic pelvic pain syndrome: a culture-independent analysis in the MAPP research network. J Urol. 2015;194:127–35.
Lewis DA, Brown R, Williams J, White P, Jacobson SK, Marchesi JR, et al. The human urinary microbiome; bacterial DNA in voided urine of asymptomatic adults. Front Cell Infect Microbiol. 2013;3:41.
• Thomas-White KJ, Gao X, Lin H, Fok CS, Ghanayem K, Mueller ER, et al. Urinary microbes and postoperative urinary tract infection risk in urogynecologic surgical patients. Int Urogynecol J. 2018;29:1797–805 In this study, the authors showed that certain preoperative urinary microbiome profiles in women lead to increased risk of postoperative, symptomatic UTI. Moreover, abundance of Lactobacillus iners was associated with protection against UTI development. This may have an important corollary in men in that dysbiosis of the urinary microbiome may lead to increased risk of disease.
Fok CS, et al. Urinary symptoms are associated with certain urinary microbes in urogynecologic surgical patients. Int Urogynecol J. 2018;29:1765–71.
Kass EH. Pyelonephritis and bacteriuria. Ann Intern Med. 1962;56:46.
Coorevits L, Heytens S, Boelens J, Claeys G. The resident microflora of voided midstream urine of healthy controls: standard versus expanded urine culture protocols. Eur J Clin Microbiol Infect Dis. 2017;36:635–9.
Gottschick C, Deng ZL, Vital M, Masur C, Abels C, Pieper DH, et al. The urinary microbiota of men and women and its changes in women during bacterial vaginosis and antibiotic treatment. Microbiome. 2017;5:99.
• Yu H, et al. Urinary microbiota in patients with prostate cancer and benign prostatic hyperplasia. Arch Med Sci. 2015;11:385–94 In this study, investigators showed a difference in bacterial flora in men with and without prostate cancer. This study utilized expressed prostatic secretions as a sample type, introducing a less invasive way to detect prostatic microbiota outside of invasive tissue sampling.
Alanee S, el-Zawahry A, Dynda D, Dabaja A, McVary K, Karr M, et al. A prospective study to examine the association of the urinary and fecal microbiota with prostate cancer diagnosis after transrectal biopsy of the prostate using 16sRNA gene analysis. Prostate. 2019;79:81–7.
• Cavarretta I, et al. The microbiome of the prostate tumor microenvironment. Eur Urol. 2017;72:625–31 This study examines the difference in microbial communities of various prostatic pathologies in patients with prostate cancer. In doing so, it suggests the microbiota to be a possible source of carcinogenesis and a potential therapeutic target.
Miyake M, Ohnishi K, Hori S, Nakano A, Nakano R, Yano H, et al. Mycoplasma genitalium infection and chronic inflammation in human prostate cancer: detection using prostatectomy and needle biopsy specimens. Cells. 2019;8:212.
• Feng Y, et al. Metagenomic and metatranscriptomic analysis of human prostate microbiota from patients with prostate cancer. BMC Genomics. 2019;20:146 The importance of this study relates to the use of advanced miciobial detection methods with metagenomic and metascriptomic profiling for detecting the non-“sterile” environment in the prostate and prostate tumor tissue.
•• Mändar R, Punab M, Korrovits P, Türk S, Ausmees K, Lapp E, et al. Seminal microbiome in men with and without prostatitis. Int J Urol. 2017;24:211–6 In this study, the authors demonstrate a different microbial profile in patients with CP/CPPS compared to controls. Importantly, there was a relative depletion of the genus Lactobacillus. These findings are similar to previous studies in women suggesting the importance of Lactobacillus in the genitourinary microbiome.
• Shoskes DA, Altemus J, Polackwich AS, Tucky B, Wang H, Eng C. The urinary microbiome differs significantly between patients with chronic prostatitis/chronic pelvic pain syndrome and controls as well as between patients with different clinical phenotypes. Urology. 2016;92:26–32 Additional evidence suggesting a difference in microbiota composition in patients with and without CP/CPPS. This study used voided urine.
Russo GI, Urzì D, Cimino S. Epidemiology of LUTS and BPH. Lower Urinary Tract Symptoms and Benign Prostatic Hyperplasia; 2018. p. 1–14. https://doi.org/10.1016/b978-0-12-811397-4.00001-9.
McConnell JD, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–98.
Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57:123–31.
McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–803.
Djavan B. The correlation between inflammation, BPH and prostate cancer. Eur Urol Suppl. 2009;8:863–4.
Pisano F. The contribution of prostate infection and inflammation to BPH and cancer. Prostatitis and Its Management; 2016. p. 87–94. https://doi.org/10.1007/978-3-319-25175-2_10.
Kashyap M, Pore S, Wang Z, Gingrich J, Yoshimura N, Tyagi P. Inflammasomes are important mediators of prostatic inflammation associated with BPH. J Inflamm. 2015;12:37.
Jiang Y-H, Lin VC-H, Liao C-H, Kuo H-C. International prostatic symptom score — voiding/storage subscore ratio in association with total prostatic volume and maximum flow rate is diagnostic of bladder outlet-related lower urinary tract dysfunction in men with lower urinary tract symptoms. PLoS One. 2013;8:e59176.
Liao C-H, Kuo H-C. Use of the international prostate symptom score voiding-to-storage subscore ratio in assessing lower urinary tract symptoms. Tzu Chi Med J. 2014;26:61–3.
Chuang F-C, Hsiao S-M, Kuo H-C. The overactive bladder symptom score, international prostate symptom score–storage subscore, and urgency severity score in patients with overactive bladder and hypersensitive bladder: which scoring system is best? Int Neurourol J. 2018;22:99–106.
Roberts RO, Bergstralh EJ, Bass SE, Lieber MM, Jacobsen SJ. Prostatitis as a risk factor for prostate cancer. Epidemiology. 2004;15:93–9.
Dennis LK, Lynch CF, Torner JC. Epidemiologic association between prostatitis and prostate cancer. Urology. 2002;60:78–83.
Masood U, Sharma A, Lowe D, Khan R, Manocha D. Colorectal cancer associated with Streptococcus anginosus bacteremia and liver abscesses. Case Rep Gastroenterol. 2016;10:769–74.
Sasaki M, Yamaura C, Ohara-Nemoto Y, Tajika S, Kodama Y, Ohya T, et al. Streptococcus anginosus infection in oral cancer and its infection route. Oral Dis. 2005;11:151–6.
Shiga K, et al. Presence of Streptococcus infection in extra-oropharyngeal head and neck squamous cell carcinoma and its implication in carcinogenesis. Oncol Rep. 2001;8:245–8.
Domann E, Hong G, Imirzalioglu C, Turschner S, Kuhle J, Watzel C, et al. Culture-independent identification of pathogenic bacteria and polymicrobial infections in the genitourinary tract of renal transplant recipients. J Clin Microbiol. 2003;41:5500–10.
Williams GD. Two cases of urinary tract infection caused by Propionimicrobium lymphophilum. J Clin Microbiol. 2015;53:3077–80.
Glassing A, Dowd SE, Galandiuk S, Davis B, Chiodini RJ. Inherent bacterial DNA contamination of extraction and sequencing reagents may affect interpretation of microbiota in low bacterial biomass samples. Gut Pathog. 2016;8:24.
Mollerup S, Friis-Nielsen J, Vinner L, Hansen TA, Richter SR, Fridholm H, et al. Propionibacterium acnes: disease-causing agent or common contaminant? Detection in diverse patient samples by next-generation sequencing. J Clin Microbiol. 2016;54:980–7.
Yow MA, et al. Characterisation of microbial communities within aggressive prostate cancer tissues. Infect Agent Cancer. 2017;12:4.
Keay S, Zhang CO, Baldwin BR, Alexander RB. Polymerase chain reaction amplification of bacterial 16s rRNA genes in prostate biopsies from men without chronic prostatitis. Urology. 1999;53:487–91.
Krieger JN, et al. Bacterial dna sequences in prostate tissue from patients with prostate cancer and chronic prostatitis. J Urol. 2000;164:1221–8.
Sfanos KS, Sauvageot J, Fedor HL, Dick JD, de Marzo AM, Isaacs WB. A molecular analysis of prokaryotic and viral DNA sequences in prostate tissue from patients with prostate cancer indicates the presence of multiple and diverse microorganisms. Prostate. 2008;68:306–20.
Xiang J, Yan H, Li J, Wang X, Chen H, Zheng X. Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer: a systematic review and meta-analysis. World J Surg Oncol. 2019;17:31.
Schaeffer AJ. Epidemiology and evaluation of chronic pelvic pain syndrome in men. Int J Antimicrob Agents. 2008;31(Suppl 1):S108–11.
Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Investig Urol. 1968;5:492–518.
Schwager S, Agnoli K, Köthe M, Feldmann F, Givskov M, Carlier A, et al. Identification of Burkholderia cenocepacia strain H111 virulence factors using nonmammalian infection hosts. Infect Immun. 2013;81:143–53.
Arzola JM, Hawley JS, Oakman C, Mora RV. A case of prostatitis due to Burkholderia pseudomallei. Nat Clin Pract Urol. 2007;4:111–4.
Organ M, Grantmyre J, Hutchinson J. Burkholderia cepacia infection of the prostate caused by inoculation of contaminated ultrasound gel during transrectal biopsy of the prostate. Can Urol Assoc J. 2010;4:E58–60.
Hütt P, et al. Characterisation of probiotic properties in human vaginal lactobacilli strains. Microb Ecol Health Dis. 2016;27:30484.
Miller EA, Beasley DE, Dunn RR, Archie EA. Lactobacilli dominance and vaginal pH: why is the human vaginal microbiome unique? Front Microbiol. 2016;7:1936.
Shoskes DA, Wang H, Polackwich AS, Tucky B, Altemus J, Eng C. Analysis of gut microbiome reveals significant differences between men with chronic prostatitis/chronic pelvic pain syndrome and controls. J Urol. 2016;196:435–41.
Murphy SF, Schaeffer AJ, Done JD, Quick ML, Acar U, Thumbikat P. Commensal bacterial modulation of the host immune response to ameliorate pain in a murine model of chronic prostatitis. Pain. 2017;158:1517–27.
Hetrick DC, et al. Musculoskeletal dysfunction in men with chronic pelvic pain syndrome type III: a case-control study. J Urol. 2003;170:828–31.
Berger RE, Ciol MA, Rothman I, Turner JA. Pelvic tenderness is not limited to the prostate in chronic prostatitis/chronic pelvic pain syndrome (CPPS) type IIIA and IIIB: comparison of men with and without CP/CPPS. BMC Urol. 2007;7:17.
Anderson RU, Wise D, Nathanson BH. Chronic prostatitis and/or chronic pelvic pain as a psychoneuromuscular disorder—a meta-analysis. Urology. 2018;120:23–9.
Shoskes DA, Nickel JC. Classification and treatment of men with chronic prostatitis/chronic pelvic pain syndrome using the UPOINT system. World J Urol. 2013;31:755–60.
Ackerman AL, Underhill DM. The mycobiome of the human urinary tract: potential roles for fungi in urology. Ann Transl Med. 2017;5:31.
Garretto A, Thomas-White K, Wolfe AJ, Putonti C. Detecting viral genomes in the female urinary microbiome. J Gen Virol. 2018;99:1141–6.
Miller-Ensminger T, Garretto A, Brenner J, Thomas-White K, Zambom A, Wolfe AJ, et al. Bacteriophages of the urinary microbiome. J Bacteriol. 2018;200(7):e00738–17. https://doi.org/10.1128/JB.00738-17
Bang C, Schmitz RA. Archaea: forgotten players in the microbiome. Emerg Top Life Sci. 2018;2:459–68.
Acknowledgments
We would like to thank the members of the Loyola Urinary Education and Research Collaborative (LUEREC) for their contributions to the work described.
Funding
AJW has been supported by National Institutes of Health grants R01 DK104718, 2 U10 HD41250, U01 DK58229, R21 DK097435, R56 DK104718, and P20 DK108268, a translational grant from the Falk Foundation, and by RFC LU206998 from Loyola University Chicago. AJW also has received funding for an Investigator Initiated Study VESI-12D01 from Astellas Scientific and Medical Affairs, Inc. AVF and LB have been supported by Loyola University Chicago RFC LU207906. LB has also been supported by the Interstitial Cystitis Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Petar Bajic and Chirag P. Doshi each declare no potential conflicts of interest.
Ryan A. Dornbier, Ahmer V. Farooq, and Larissa Bresler report intramural funding from Loyola University Medical Center Research Committee.
Alan J. Wolfe reports grants from Astellas Scientific and Medical Affairs and Kimberly Clark Corporation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The funding sources have had no role in design or conduct of the studies; collection, management, analysis, and interpretation of the data; or in preparation, review, or approval of this or any other manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Benign Prostatic Hyperplasia
Rights and permissions
About this article
Cite this article
Bajic, P., Dornbier, R.A., Doshi, C.P. et al. Implications of the Genitourinary Microbiota in Prostatic Disease. Curr Urol Rep 20, 34 (2019). https://doi.org/10.1007/s11934-019-0904-6
Published:
DOI: https://doi.org/10.1007/s11934-019-0904-6