Abstract
Purpose of Review
Based on the discussions of a symposium co-organized by the Université Libre de Bruxelles (ULB) and the University of Lausanne (UNIL) in Brussels in 2019, this paper critically reflects upon the zero-tolerance strategy on “Female Genital Mutilation” (FGM) and its socio-political, legal and moral repercussions. We ask whether the strategy is effective given the empirical challenges highlighted during the symposium, and also whether it is credible.
Recent Findings
The anti-FGM zero-tolerance policy, first launched in 2003, aims to eliminate all types of “female genital mutilation” worldwide. The FGM definition of the World Health Organization condemns all forms of genital cutting (FGC) on the basis that they are harmful and degrading to women and infringe upon their rights to physical integrity. Yet, the zero-tolerance policy only applies to traditional and customary forms of genital cutting and not to cosmetic alterations of the female genitalia. Recent publications have shown that various popular forms of cosmetic genital surgery remove the same tissue as some forms of “FGM”. In response to the zero-tolerance policy, national laws banning traditional forms of FGC are enforced and increasingly scrutinize the performance of FGC as well as non-invasive rituals that are culturally meaningful to migrants. At the same time, cosmetic procedures such as labiaplasty have become more popular than ever before and are increasingly performed on adolescents.
Summary
This review shows that the socio-legal and ethical inconsistencies between “FGM” and cosmetic genital modification pose concrete dilemmas for professionals in the field that need to be addressed and researched.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In May 2019, social scientists, healthcare providers, activists and other professionals working for governmental and non-governmental organizations, from Europe, North America, Australia, Asia and Africa met in Brussels, Belgium, for a symposium co-organized by the Université Libre de Bruxelles (ULB) and the University of Lausanne (UNIL), Switzerland, to discuss perspectives and daily challenges regarding the international zero-tolerance policy on female genital mutilation (FGM).Footnote 1 Four speakers—Janice Boddy, Brian Earp, Omar Abdulcadir and Stephanie Florquin, whose papers are released in this special issue—presented their take on the debate, which was followed by a 2-hour discussion with the audience. The symposium was opened by the ULB anthropologist Asuncion Frezsnoza-Flot with personal memories of what was called female circumcisionFootnote 2 among fellow students in the Philippines. The custom, locally called tuli or pag Islam, was not publicly called into question at the time nor perceived to be controversial in the Philippines in the 1980s and 1990s. In contrast to this, male circumcision and the stigma that uncircumcised men are subject to was hotly debated in the media. In the meantime, international discourses on the practice have changed. All traditional forms of genital modifications of the female body are now commonly referred to as “female genital mutilations”.
Female genital mutilation (FGM)—also known as “female circumcision”, or female genital cutting (FGC), the term preferred in this paper except when quoting other viewpointsFootnote 3—is the generic term used by United Nations (UN) agencies, political actors, activists and the media more generally to refer to a customary form of genital modification commonly performed in 28 African countries and a few South-Asian countries in order to meet social norms linked to sexuality, gender, aesthetics, purity and virtue. The zero-tolerance policy, first launched on the 6 February 2003, is annually celebrated as the International Day of Zero-Tolerance for FGM and aims to eliminate all types of FGC worldwide. According to the definition of the World Health Organization (WHO), FGM constitutes “all procedures involving partial or total removal of the female external genitalia or other injury to the female genital organs for non-medical reasons” [1]. The FGM definition applies regardless of whether it involves a pricking or a nicking without removal of genital tissues and a visible physical scar in the long term. It also includes tissue stretching/elongation as well as more invasive practices including cutting or narrowing the female external genitals (e.g. infibulation, that is, the narrowing of the vaginal introitus by apposition of the labia, with or without excision of the glans more or less part of the body of the clitoris). This definition is also used if the procedure is performed by a traditional practitioner or a healthcare professional, with consent or without, regardless of whether it is practiced on a child or an adult woman—the tolerance is “zero”.
According to the latest figures, more than 200 million women and girls worldwide have undergone some kind of FGC according to the definition above, of which 1 million women, mostly migrants from Sub-Saharan countries, live in high-income countries [2]. Studies show that the performance of the practice and its meaning changes in the diaspora and many come to completely reject and abandon it [3,4,5,6,7,8,9]. For some, however, the practice is highly cherished or symbolically meaningful, for various reasons including religious belief or perception of women’s increased value in marriage [10,11,12,13,14]. In an attempt to deter parents from performing invasive types of FGC, clinicians across different countries, and in 2010 the American Academy of Paediatricians, had suggested that alternative rituals such as pricking, nicking or other symbolic forms of FGCFootnote 4 might be considered [15,16,17]. However, such propositions caused outrage particularly among women’s rights activists, arguing that alternative forms of FGC could slow down the overall progress of abandonment efforts. After withdrawing this controversial recommendation, the American Academy of Paediatricians issued a new statement to this effect, recommending sensitisation against any form of FGC, including non-invasive ritual forms [18].
The UN condemns all forms of FGC based on the argument that they violate a number of recognized human rights protected by international and regional human rights instruments, including the right to be free from gender-discrimination, the right to the highest attainable standard of health; the right to life (when the procedure may lead to unintended death); the right to freedom from torture or cruel, inhuman or degrading treatment or punishment; and the rights of the child. These human rights are enshrined in various treaties that are legally binding upon the states that have ratified them [19]. Today the term “zero-tolerance” has been adopted by international institutions, governmental and non-governmental organizations, and is commonly used in the policy language of the European Institute for Gender EqualityFootnote 5 and the European Parliament [20, 21].
Following health recommendations, human rights decrees and international agreements, governments all over the world are gradually adopting the zero-tolerance approach of the United Nations. The issue is no longer merely a question of ethnic identity, cultural aesthetics or personal preference; rather, it has become a moral imperative to protect the female body from culturally endorsed forms of violence and genital mutilations. This position is now consolidated by law and international policies. Furthermore, this is not merely a moral and legal issue but also an economic one because awareness-raising activities, which are mainly run by non-governmental organizations, are funded only by international institutions if they apply the zero-tolerance approach.
Questioning the zero-tolerance approach has come to be perceived as controversial by many. The final speaker of the symposium Stéphanie Florquin, vice director of the Belgian NGO “GAMS”, who was invited to speak about the challenges the zero-tolerance policy can elicit from a professional activist perspective, confessed that she received negative feedback when she shared the invitation of this symposium with her professional networks because the title of the program read “rethinking zero-tolerance”. With surprise, some activists and partners asked if GAMS was now against zero-tolerance. It shows, she argued, how sensitive this issue is, and how difficult it can be to adopt a critical stance on the approach.
This introductory chapter to the special issue sets out to give an overview of the debates following the timeline of developments, as well as highlighting some of the ramifications of the zero-tolerance policy as described in recent news reports and witness accounts made by participants during the symposium. This will be followed by the contributions of the four speakers of the symposium who each stress various layers of challenges linked to the zero-tolerance approach: socio-cultural, ethical, medical and socio-legal. Aware of the fact that the zero-tolerance policy was formulated with the best intentions, we wish to critically reflect upon this strategy given its socio-political, legal and moral repercussions. We ask whether the zero-tolerance strategy is effective given the empirical challenges highlighted during the symposium and also whether it is credible.
Cutting What? Controversies Around Female Genital Cutting and Socio-Legal Inconsistencies
The zero-tolerance strategy intends to promote respect for the physical integrity and rights of all women and girls. However, it has Western-centric implications that unequally distribute the right to dispose of one’s body according to race and ethnicity. Indeed, the prohibition only concerns the customary genital cutting practices in African and South-Asian countries but does not apply to female genital cosmetic surgeries, which are increasingly desired and practiced on white adult women and under-age girls worldwide. Commonly performed cosmetic surgeries include labiaplasty which involves the partial or complete removal of the labia minora for aesthetic reasons, as well as “cosmetic” clitoridectomy, hoodectomy and vaginal tightening. Although these cosmetic procedures involve the cutting of the same parts of the genitalia as FGM type I or II, for instance, as Earp shows (see Earp in this special issue), it is commonly argued that “FGM” and genital cosmetic surgery cannot be compared. For instance, as Bader [22] highlights, experts frequently point out that FGC is performed on underage girls without their consent, whereas genital cosmetic surgery is an informed choice made by adult women aware of the consequences.
However, various elements of this argument are flawed. First of all, the prohibition of FGM in many Western countries is also extended to adult women, while cosmetic surgeries are sometimes performed on underage girls’ genitalia. Secondly, the call for the respect of children’s rights is only applied to girls, whereas other medically unnecessary genital modification practices such as on intersex infants and boys as performed in Western clinics or even in FGC-practicing countries are overlooked by the zero-tolerance policy (Chase 2002; Ehrenreich and Barr 2015; Kraus 2013). The recent declaration of the unconstitutionality of the US anti-FGM ban by a federal judge in 2018 relied precisely on the argument that protection from genital cutting should be equally guaranteed to all children, regardless of their gender [23].
Medical recommendations on genital cosmetic surgery indicate that such procedures should not be performed on minors [24,25,26]. The American College of Obstetricians and Gynaecologists [2, 24] writes, “Although there may be a perception that labiaplasty is a minor procedure, serious complications can occur (e.g., pain, painful scarring, dyspareunia, hematoma, oedema, and infection)”. Despite these recommendations, the number of cosmetic surgeries is increasing worldwide, including among minors. The Independent newspaper in the UK states that “more than 200 girls under 18 had labiaplasty on the NHS in 2015-16 — more than 150 of whom were under 15”, a procedure that surgeons consider as the “world’s fastest-growing cosmetic procedure” [27]. The International Society of Aesthetic Plastic Surgery statistics indeed show that in 2016, 45% more labiaplasty procedures were carried out than in 2015, which in 2017 amounted to a reported total of 138,765 labiaplasties performed worldwide [28, 29].
Until recently, Western public discourse considered scholarship on the comparison between FGC and other genital modifications on adult women and minors such as intersex surgeries, male circumcision, and genital cosmetic surgeries as mere intellectual concerns. However, the heated discussion during the symposium demonstrates that what has long been considered an academic preoccupation is posing real-life challenges with moral dilemmas. Professionals working with women and girls who have undergone FGC in compromising positions in socio-legal and healthcare settings as well as during prevention campaigns, both in societies where the practice is normative and among diaspora communities in high income countries. Yet, to date little has been published on the challenging situations that arise as consequences of the contradictory aspects of zero-tolerance policies for professionals and the campaigns that are shaped by and respond to international agreements, human rights laws and health recommendations.
Zero-Tolerance and the Emergence of FGC as a Global Concern
The zero-tolerance policy has its origins in the international movements against FGC. The terms female “genital mutilation” and “sexual mutilation” first appeared in the 1970s when internationally organized campaigns against the practice became successful. Although campaigns against the practice have been around since the beginning of the twentieth century [30, 31], the League of Nations, and after 1946 the Economic and Social Council (ECOSOC) of the UN, refused to take it up as an agenda or recommend legislation against it due to the conflicts that campaigns against the practice caused in the colonies of Sudan and Kenya [30,31,32].
Abu-Sahlieh [32] notes that female circumcision, as it was still called at the time, came up for the first time in a conference held by the Société pour la sauvegarde de l’enfance in Geneva in 1931, when some European delegates pleaded for an end to these “barbaric customs”. However, the majority did not share their views, and the subject was dropped until the 1950s [32]. In 1952, the ECOSOC recommended its member states to act towards abolishing all forms of violence against women that violate the physical integrity and dignity of women according to the universal declaration of rights including “female circumcision”. Yet, 7 years later, it was decided at an international assembly of the WHO that no further action should be taken because “these ritual operations […] are a result of social and cultural conceptions” [32].
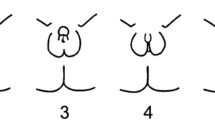
In 1976, the ECOSOC pushed the WHO to publish the Robert Cook report, which defined the four types of FGM that are still used today: clitoridectomy (I), excision (II), infibulation (III) and all other harmful procedures to the female genitalia for non-medical purposes, e.g. pricking, piercing, incising, scraping and cauterizing the genital area (IV). Three years later, at a seminar on “traditional practices affecting the health of women and children” in Khartoum, Sudan, the WHO officially became committed to “fighting against” FGM [32, 33]. Feminist activism and policy-related research undertaken for instance by Fran Hosken—now well-known for the Hosken Report: Genital and Sexual Mutilations of Females [34]—provided evidence and raised awareness of the issue at an international level.
In 1991, the WHO recommended that the UN adopt the term “female genital mutilation” and since then this label has been commonly used in UN documents [35]. In 1997 a joint statement by the WHO, UNICEF, and the UNFPA was published stating their shared commitment to bring the practice to an end [36].
Anti-FGM Bans
The enactment of a global ban formed a crucial part of the global anti-FGM strategy. Feminist activism advocating the eradication of FGC in the 1970s fell on fertile ground in Europe and North America. As African migrants started arriving in the global North, laws were soon put into place to criminalize the practice. France was the first European country to outlaw FGM in 1979. In their Penal Code, FGM is classified as a form of assault punishable as an “act of violence causing mutilation or permanent disability” (Article 222–9). Three years later, Sweden enacted a specific law prohibiting FGM. The Swedish initiative was followed by many other countries worldwide, including receiving countries in the global North as well as countries where the practice is socially normative in the global South.Footnote 6 The idea was that legislative reform should be supported by social change programmes aiming to strengthen the environment for the abandonment of FGC and the internalization of new socio-legal norms [37]. While some countries outlaw FGC only on minors, others extend the prohibition to adult women. These laws are enforced according to the definitions of the zero-tolerance policy—namely, in a stricto sensu interpretation. The following Australian and Swiss criminal court cases are illuminating examples of how the law is interpreted strictu sensu when FGM is carried out on minors, regardless of whether physical damage is observed and whether the procedure was performed prior to or after migration. This strict prohibition is also applied to adult African women who wish to undergo FGC (see the Kenyan case below), yet is not applied when protagonists involved (i.e., doctors and patients) are white (see the British case).
In Australia, a criminal investigation in November 2015 led to the conviction of the mother of two girls of Indian origin for having her daughters “mutilated” despite the fact that there was no physical scar according to expert examinations. The girls had gone through a Dawoodi Bohra ceremony during which their clitoral hood was “nicked” with a sharp tool [38]. The mother, the nurse performing the ritual and the community leader were charged with 15 months imprisonment.Footnote 7 Three years later, however, they were all acquitted after the judge ruled that physical “damage” must have occurred to call this intervention a “mutilation” [39]. New medical evidence that was presented showed that the clitoral glans of both girls was untouched. It was claimed that this evidence had been “absent” at the time of the trial because of the girls’ pre-puberty status.Footnote 8 In October 2019, the prosecutors sought an appeal to the Australian high court which stated that, even though no physical damage had been made, FGM was “illegal in all its forms”.Footnote 9 However, experts warned that re-opening this trial would cause more trauma to the girls.
In Switzerland, a Somali mother was convicted in August 2018 for having had her two daughters cut in Somalia before immigrating to Switzerland. The judge of the Swiss canton of Neuchâtel applied the second paragraph of the Swiss anti-FGM Act stating the universality of the offence, which allows the prosecution of anybody who is—at the time of the prosecution—in Switzerland, regardless of where and when FGM took place. Despite the fact that this case constitutes a first in European legal history of FGC [40], this conviction raised concerns among professionals working with the African diaspora. First of all, it was not clear whether professionals from now on had the duty to report every parent who had performed FGC on their daughters before immigrating to Switzerland. Secondly, there were doubts about whether long-established foreign residents would be threatened with deportation [41], as FGC is listed as among the crimes leading to mandatory deportation [40]. Finally, it was uncertain whether ongoing and future asylum requests made by families with daughters affected by FGC would be rejected because they had already breached the Swiss criminal law [42].
Critiquing Inconsistencies—the Debate on the Asymmetry in the Regulation of Genital Cosmetic Surgery and FGM
The strict reading of national anti-FGM legislations with regard to traditional forms of FGC stands in stark contrast to the lack of regulation of other genital modification practices on minors, such as male circumcision and female genital cosmetic surgery. For instance, Essén and Johnsdotter [43] pointed out that in three Scandinavian countries (Sweden, Norway and Denmark), operations on the external female genitalia that are designed to “mutilate them” or to produce permanent changes are prohibited and “must not take place, regardless of whether consent has or has not been given” (Swedish law). In the Danish law, the line between genital cosmetic surgery and FGM is even more blurred: “Any person who, by committing an act of violence, with or without consent, excises or in other way removes, in part or completely, female external sex organs shall be liable to imprisonment for any teiui not exceeding six years.” (§ 245 a) There is little ambiguity about the formulation of this law. Stricto sensu labiaplasty and hoodectomy are punishable with a prison sentence, regardless of whether consent has been obtained and even when the procedure is performed in medical settings by a surgeon. Essén and Johnsdotter [43] argue that age, ethnic background and consent should be irrelevant to the laws and hence any kind of non-medically motivated change to the genitalia ought to be punishable. Yet, according to our investigations, labiaplasty is performed in Denmark in public hospitals if “medically indicated” and privately for those willing to pay.
Writing almost three decades ago, legal ethicists, for instance, Bibbings and Aldridge [44] Sheldon and Wilkinson [45], raised concerns about the asymmetrical treatment of FGM and genital cosmetic surgery before the law. They warned of the lack of consistency of laws that distinguish between practices whereby the same parts of the genitalia are cut. Bibbings [46] advises that any legal regulation of body-altering practices should be consistent. She argues that if restrictions are to be imposed, they should be constructed according to valid health concerns and should treat the practices according to the risk involved, rather than merely enforcing dominant notions of the acceptable body.
Johnsdotter and Essén [47] argue that non-discriminatory policies should be adopted, which implies identifying a consistent and coherent stance in which key social values—including protection of children, bodily integrity, bodily autonomy, and equality before the law—are upheld. Different suggestions have been made as to how consistency could be achieved. Berer [48] calls for the prohibition of genital cosmetic surgery under the anti-FGM law. By contrast, Dustin [49] proposes to judge all forms of genital modification as cultural practices, possible on consenting adults but not on minors. She argues that this results in the prohibition of male circumcision and intersex surgery on minors, as well as the legality of re-infibulation and genital cosmetic surgery for adult women. Shahvisi [50], on the other hand suggests that all children should be equally protected from non-therapeutic genital surgeries while leaving adult women their agency and right to self-determination.
The Empirical Challenges
The corpus of scientific research and its conclusions regarding inconsistency nonetheless seem to pass unheard by lawmakers, and national and international organizations including the WHO, who continue to stand firm on the issue and hold that the “conceptual similarities” [51] between FGM and genital cosmetic surgery are irrelevant. Yet, this double standard produces empirical challenges and moral dilemmas for professionals.
Interpreting FGM in Court
A first challenge is the question of how the term FGM is interpreted in court when it comes to consenting adults undergoing either genital cosmetic surgery or FGC. The following two court cases illustrate the asymmetry in the clinical and legal handling of cases of FGC and genital cosmetic surgery and the unequal allocation of rights depending on ethnicity:
In the first case the white British surgeon, David Veale, who performed “cosmetic clitoridectomy” on a non-migrant woman was acquitted from prosecution under the anti-FGM law in February 2017. In a case report published in 2011 in the Archives of Sexual Behaviour, Veale and his colleague Joe Daniels explain that the 33-year-old patient had already undergone labiaplasty and hoodectomy but was still unhappy with the appearance of her clitoral glans and the increased unhooded sensitivity. Once clitoridectomy was performed, the patient was said to be “very satisfied with the outcome”. She stated that the simple “nothing there” look is just what she wanted 20 years ago [52]. During the criminal investigation, Veale, a Senior doctor based at Maudsley Hospital in London, defended his approval of the procedure saying “the bottom line for me is freedom of choice. You have a freedom of choice if you have capacity for consent to do what you wish with your own body”.Footnote 10 This case makes plain that the consent of a British adult woman of non-migrant background bears more weight in the legal defence in court than the actual formulation of the legislation.
In contrast to this, we have the case of a female Kenyan doctor, Tatu Kamau, who launched a petition to legalize FGC on adult women in her country and to allow its medicalisation, by mobilizing an argument that echoes the rationale of genital cosmetic surgery: “women should be allowed to do what they want with their bodies.”Footnote 11 Kamau was representing herself in the case before the Nairobi High Court where she argued that the practice was an age-old Kenyan tradition and that an outright ban infringed on a woman’s right to exercise her cultural beliefs. She further stated that the term mutilation was “offensive” and denigrated the cultural significance of the practice.Footnote 12 In fact, as Kenyan scholar Samuel Kimani highlighted at the symposium, Kenya extended its FGM ban in 2011 to adult women after realizing that 18-year-old women were asking for FGC for themselves. Kamau’s call for the decriminalization of FGC is, however, not an isolated one. Women in Liberia, Sierra Leone and Gambia are now campaigning for the right of adult women to undergo some forms of FGC once they have reached the age of majority, as reported in the CoP online discussion group of experts on FGC.Footnote 13
The porous borderline between FGM and genital cosmetic surgery raises questions about whether women who have undergone genital cosmetic surgery and feel “mutilated” afterwards may sue their surgeon based on the FGM Act. On a French online discussion forum about labiaplasty, one can read testimonies such as: “Hi, it may be late, but you should know that every woman is different. I made the mistake of having the operation, the surgeon botched it, I’m mutilated and traumatized. I don’t feel the same way at all. If others have had a botched labiaplasty, thank you for telling me about it and how you coped with it.” [see 53; translation ours] Echoing scholars’ concerns, the American College of Obstetricians and Gynaecologists [24] also warned that performing labiaplasty may be criminalized under the FGM ban. As Bader and Mottier [40] demonstrate for Switzerland, the technical similarities between FGC and genital cosmetic surgeries were well acknowledged by lawmakers when drafting the anti-FGM Act. Yet, members of parliament provided provisions to prevent misreading by stressing verbally, but not in writing, that judges should not criminalize genital cosmetic surgeries under the FGM law.
Sustaining Credibility
A second challenge concerns the credibility of anti-FGM campaigns following the zero-tolerance policy due to contradictory messages surrounding medically unnecessary genital alterations. Such campaigns tell practicing communities that pricking (symbolic form of FGC, type 4) is prohibited and should not be considered an alternative to more invasive forms of FGC. Yet these campaigns do not address genital cosmetic surgery, genital piercings and male circumcision. The Eritrean-Swiss psychiatrist Fana Asefaw [54] observes, “Immigrant women react with incomprehension to the fact that genital piercing, also on the erogenous zones (labia and clitoris), is trendy in the industrial nations and at the same time there are campaigns against the proposal of ‘symbolic circumcision’, which is basically the same as piercing”.
The first presenter at our symposium, anthropologist Janice Boddy, reported that when she presented her paper about genital cosmetic surgery at Ahfad University for Women in Khartoum, Sudan (a university that is actively working to end FGC), the audience “was stunned that we in the West are moving in the direction that they have been fighting against all their lives” (see Boddy in this special issue). She further reported that these women were concerned that genital cosmetic surgery could provide an alternative for families who wish to continue FGC—a fear shared by Samuel Kimani who suggested that the availability of genital cosmetic surgery might be an encouragement for people to continue with FGC. Stéphanie Florquin, the last speaker, stressed that some male proponents of (some types of) FGC are using the argument of the legality of male circumcision to call into question the abandonment of FGC. This observation had also been made by Otibho Obianwu, from the Population Council, who reported that in Nigeria, where male circumcision is commonly performed on boys (80% of Nigerian males), healthcare professionals ask for advice about the disparity between FGC and male circumcision.
Furthermore, globalization has added new challenges to the zero-tolerance policy. Accelerated modes of communication, images, access to information and news via the Internet from mobile phones connect the different parts of the world faster than ever before. Regardless of whether it is depictions of women’s bodies, pornography or advertisements for genital cosmetic surgery, images of the body and of female genitalia are no longer bound to socio-cultural spaces but are accessible to anyone anywhere in the world. Otibho Obianwu highlighted that reality TV brings explicit images of extreme cosmetic makeovers of Western women into the living rooms of Nigerian households. Boddy’s ethnographic examples from the Sudan echo this finding and the potential repercussions. She reported that young Sudanese men—who at first seem perfectly willing to marry uncut brides—sometimes sent their wives home after “discovering” that their vulva does not look like what they believe to be “normal” female genitalia—namely, as in the pornographic images of white women’s photoshopped or surgically modified genitals that they were used to seeing on the Internet [55].
Genital Cosmetic Surgeries on Women with FGC
An additional challenge emerges in debates around how genital cosmetic surgery performed on women from FGC-practicing communities is understood. According to anthropologist Adriana Kaplan, some surgeons in Spain show reluctance to perform genital cosmetic surgery on adult women on the basis of their ethnic origin. Stéphanie Florquin recalled that their NGO, which is alerted by the authorities in cases of suspected risk of FGC on underage girls living in Belgium, had been informed about a Somali teen who has undergone labiaplasty. The mother of the girl explained that her daughter was going to be fine in the cultural context of this ritual practice because she had got “the cut” in a medical setting. It was, indeed, a “medically indicated” labiaplasty following the girl’s complaints about discomfort when cycling. Florquin suggested that if the girl had not been of Somali origin, their NGO would never have heard of the case, which confirms that there are racial disparities in the ways that such cases are judged, reported and handled (see Florquin and Richard in this special issue).
The Kenyan sociologist Eva Komba pointed out that FGM and genital cosmetic surgery are debated as if they were two separate practices. However, what happens when these practices converge, for example, when both clitoral reconstruction (because of FGC) and labiaplasty are performed on the same women? For instance, it sometimes happens that during FGC the labia are cut asymmetrically. The third speaker of the symposium, Dr. Omar Abdulcadir, highlighted that a surgery of symmetrisation of the labia after FGC might be seen by some as a cosmetic labiaplasty and by others as a therapeutic corrective surgery (see Abdulcadir et al. in this special issue). Yet others may argue that it is a form of “re-excision” as the remaining genital tissue is removed just like during the first FGC. In other words, there is a blurred line between FGC and genital cosmetic surgery that gynaecologists must think about in their daily practices with legal and economic implications. For instance, if it is considered to be a corrective therapeutic surgery, the procedure is most likely to be covered in many Western healthcare systems, but if it is defined as cosmetic, then it is likely not be covered or reimbursed. It is unlikely that a surgeon would classify the symmetrisation of the labia as “FGM”. Yet as we have seen, if something goes wrong and the patient is unhappy with the outcome, the surgeon could be sued under the anti-FGM law.
Reaching Consistency: Is Individual Consent a False Solution?
Another important aspect that was debated extensively at the symposium was the issue of consent. Speakers and participants discussed whether individual consent could be a solution to reaching consistency. If we reject the concept of zero-tolerance because of the double standard relating to genital cosmetic surgery, under what circumstances might genital modifications be justified? For instance, should it be permissible to allow genital modifications such as pricking, labiaplasty and re-infibulation above the age of 18 if consent is obtained? On the surface it seems like introducing a policy linked to consent might resolve the controversial aspects of the zero-tolerance stance. This solution might be able to grant both—bodily integrity (the right to say no) and bodily autonomy [having the freedom to say yes or no].
However, the concept of individual informed consent is a Western notion that would not apply to many contexts where autonomy is not necessarily obtained at a particular age but through initiation, for instance, as the second speaker Brian Earp pointed out. Adriana Kaplan illustrated this with examples from Casamance, southern Senegal. She said that during her NGO’s investigations, they realized that people did not want to drop circumcision and excision ceremonies because they felt that it empowered them and granted individuals status within their community. Anthropologist Bettina Shell-Duncan argued that the concept of informed consent is based on individual rights within a context where autonomous personhood is taken for granted. Yet, in many rural communities in Africa, decisions are not taken by individuals alone, but in a relational way with the interests of the larger community in mind. Bettina Shell-Duncan and Sarah O’Neill noted that when decisions regarding the body are made, it is not a question of individual free choice, but rather a question of group identity and belonging influenced by customary ties of solidarity which are linked to a sense of honour and reputation. As a result of this relational personhood—drawing one’s sense of identity from belonging to a particular group—people may not want to make decisions that greatly differ from their identity group, Shell-Duncan argued.
Particularly in rural places where governmental infrastructure, healthcare and social services are weak or non-existent, people rely on each other as a safety net. It is thus not merely a question of cultural identity and belonging but also of safety and survival. The risk of taking a decision alone may mean losing one’s community support and slipping through the safety net. An important question to ask is what would consent even look like in this context and how to conceptually move away from relational personhood in autonomous decision making.
Conclusions
It is important to reaffirm, that we, the authors, all personally reject FGC and also strive professionally for action. However, our aim here is to point out that the zero-tolerance policy puts professionals in various disciplines in challenging situations. Fifty years after the first feminist activists rose awareness among the scientific community and international policy makers that the customary genital modification on girls commonly referred to as “female circumcision” were in fact a “mutilation” that violates women’s human rights and physical integrity, it seems that concerns about the definition of FGM has re-emerged due to inconsistencies of the zero-tolerance policy. There is lack of clarity about what kinds of female genital modifications constitute an aesthetic enhancement, a meaningful ritual within a traditional or religious context, or a “mutilation” and violation of rights.
Our concerns are not about the moral “rightness” of banning and trying to stop invasive forms of FGC. Quite to the contrary. If we want to put an end to these practices worldwide, we need to address, both conceptually and empirically, the real-life consequences of the inconsistencies of policies that justify certain genital modifications to the exclusion of others based on gender, race and ethnicity.
Before the thriving success of genital cosmetic surgery, the Western imperialism tag of the FGM campaign was rebuffed with the argument that the concern was the bodily integrity and human rights of all women. Yet, the inconsistencies and empirical challenges mentioned in this paper suggest that unfortunately race and ethnicity are benchmarks within the zero-tolerance policy for determining whether a bodily practice is a “mutilation” or a cosmetic procedure. Earp and Johnsdotter [56] recently wrote “the WHO appears to be engaged in highly selective condemnation of only non-Western, female-only genital cutting, irrespective of harm, consent, or the comparability of the cutting to other medically unnecessary practices”.
The condemnation of some genital modification practices and the acceptance, or even legitimation, of others lead to the question: what could be an acceptable baseline for determining the (in)tolerance towards bodily practices: consent, age, health consequences, or gender? To this question, a consortium of 91 scholars from various disciplines and countriesFootnote 14—known as the Brussels Collaboration on Bodily Integrity [57] since the idea emerged during the symposium—responded that the respect for the bodily integrity of all children can be a non-discriminatory basis to avoid medically unnecessary genital modification practices on minors. What this collaboration further demonstrates is that a large group of experts with different scientific interests—whether specialists in FGC, genital cosmetic surgery, male circumcision or intersex surgeries—are able to collaborate in order to try to reach consensus. This interdisciplinary collaboration thus set an encouraging step towards building bridges between stakeholders and academics.
This introductory chapter and the overall discussion in this special issue shows that what might have been perceived as mere “academic pursuits” and “philosophical thoughts” about the double standard in FGC and other genital modification practices are also the reflection of concrete dilemmas for professionals in the field that need to be addressed and researched.
Notes
The term female circumcision is commonly used by women who cherish the practice as a significant cultural or religious tradition. The connotations of the term are that it is equivalent to male circumcision. Yet on an anatomical level, it corresponds only to the FGM/C type Ia and is, therefore, not representative of all the different types
We refer to FGM when discussing the global abolitionist strategy and FGC to designate customary forms of genital modification
Source: https://www.csmonitor.com/World/2016/0225/Are-ritual-nicks-a-humane-alternative-to-FGM-Doctors-debate (accessed 15 August 2020); https://www.newsweek.com/fgm-compromise-nick-western-countries-429250 (accessed 15 August 2020)
For example, the United Kingdom (1985), the United States (1996), Ivory Coast (1998), Spain (2003), Ethiopia (2004), Italy (2006), Eritrea (2007), Egypt (2008), Somalia and Switzerland (2012) [2].
Source: https://www.abc.net.au/news/2019-10-16/high-court-rules-female-genital-mutilation-illegal-in-all-forms/11606396 (Accessed 7 August 2020)
Source: https://www.abc.net.au/news/2018-08-11/genital-mutilation-convictions-overturned/10108106 (Accessed 2 December 2019)
Source: https://www.mediquality.net/fr/web/MediQuality/-/kenyan-doctor-goes-to-court-to-legalize-female-genital-mutilation(Accessed January 28, 2018).
Source: https://edition.cnn.com/2019/10/25/africa/kenya-doctor-fgm-petition-intl/index.html(Accessed January 6, 2020).
Source: https://copfgm.org/2019/11/25/type-iv-contributions-des-membres (Accessed December 2, 2019)
Including ethicists, public health professionals, legal scholars, social scientists, and feminists from Africa, Asia, Australasia, Europe, the Middle East and the Americas.
References
WHO. Care of girls and women living with female genital mutilation. A clinical handbook. Geneva: World Health Organization; 2018.
UNICEF. Female genital mutilation/cutting: a statistical overview and exploration of the dynamics of change. New York: UNICEF; 2013.
Agboli A, Botbol M, O’Neill S, Richard F, Aujoulat I. Transforming vulnerability into power: exploring empowerment among women with female genital mutilation/cutting (FGM/C) in the context of migration in Belgium. J Human Dev Capabil. 2019;21(1):49–62. https://doi.org/10.1080/19452829.2019.1661981.
Johansen RE. Undoing female genital cutting: perceptions and experiences of infibulation, defibulation and virginity among Somali and Sudanese migrants in Norway. Cult Health Sex. 2017;19(4):528–42. https://doi.org/10.1080/13691058.2016.1239838.
Johnsdotter S, Essén B. Cultural change after migration: circumcision of girls in Western migrant communities. Best Pract Res Clin Obstet Gynaecol. 2016;32(Supplement C):15–25. https://doi.org/10.1016/j.bpobgyn.2015.10.012.
Johnsdotter S, Mestre i Mestre RM. ‘Female genital mutilation’ in Europe: public discourse versus empirical evidence. Int J Law Crime Justice. 2017;51:14–23. https://doi.org/10.1016/j.ijlcj.2017.04.005.
Kahn S. “You see, one day they cut”: the evolution, expression, and consequences of resistance for women who oppose female genital cutting. J Hum Behav Soc Environ. 2016;26(7–8):622–35. https://doi.org/10.1080/10911359.2016.1238805.
Villani M, Bodenmann P. FGM in Switzerland: between legality and loyalty in the transmission of a traditional practice. Health Sociol Rev. 2017;26(2):160–74. https://doi.org/10.1080/14461242.2016.1254058.
Vloeberghs E, van der Kwaak A, Knipscheer J, van den Muijsenbergh M. Coping and chronic psychosocial consequences of female genital mutilation in the Netherlands. Ethn Health. 2012;17(6):677–95. https://doi.org/10.1080/13557858.2013.771148.
Ahmadu F. Ain’t I a woman too? challenging myths of sexual dysfunction in circumcised women. In: Shell-Duncan B, Hernlund Y, editors. Transcultural bodies: Female genital cutting in global context. London: Rutgers University Press; 2007. p. 278–310.
Ahmadu F. Rites and wrongs: an insider/outsider reflects on power and excision. In: Shell-Duncan B, Hernlund Y, editors. Female “circumcision” in Africa: Culture, controversy, and change: Lynne Rienner Publishers; 2000. p. 283–312.
Boddy J. Wombs and alien spirits: women, men, and the Zar cult in northern Sudan: University of Wisconsin Press; 1989.
Gruenbaum E. The female circumcision controversy: an anthropological perspective. Philadelphia: University of Pennsylvania Press; 2001.
Johnson M. Becoming a Muslim, becoming a person: female “circumcision”, religious identity and personhood in Guinea-Bissau. In: Shell-Duncan B, Hernlund Y, editors. Female “circumcision” in Africa: culture, controversy, and change: Lynne Rienner Publishers; 2000. p. 215–34.
Lambelet CD. The Seattle compromise: multicultural sensitivity and Americanization. Duke Law J. 1997;47:717–83.
Catania L, Abdulcadir O. Ferite per sempre. Le mutilazioni genitali femminili e la proposta del rito simbolico alternativo. Derive Approdi; 2005.
Arora KS, Jacobs AJ. Female genital alteration: a compromise solution. J Med Ethics. 2016;00:1–7.
Committee on Bioethics. Policy statement—ritual genital cutting of female minors. Pediatrics. 2010;125(5):1088–1093. https://doi.org/10.1542/peds.2010-0187.
UNFPA. Implementation of the international and regional human rights framework for the elimination of female genital mutilation: UNFPA; 2014.
Shreeves R. Zero tolerance for female genital mutilation. At a Glance. European Parliament; 2015.
Askew I, Chaiban T, Kalasa B, Sen P. A repeat call for complete abandonment of FGM. J Med Ethics. 2016;42(9):619–20.
Bader D. Nationalisme sexuel: le cas de l'excision et de la chirurgie esthétique génitale dans les discours d'experts en Suisse. Swiss J Sociol. 2016;42(3):574–98. https://doi.org/10.1515/sjs-2016-0025.
Earp B. Why was the U.S. ban on female genital mutilation ruled unconstitutional, and what does this have to do with male circumcision? Ethics Med Public Health. 2020;15. https://doi.org/10.1016/j.jemep.2020.100533.
American College of Obstetricians and Gynecologists. Breast and Labial Surgery in Adolescents. Committee Opinion No. 686. Obstet Gynecol. 2017;129:e17–9.
Royal College of Obstetricians & Gynaecologists. RCOG/BritSPAG statement on BBC report of under 18s seeking labiaplasty. Royal College of Obstetricians & Gynaecologists; 2017.
British Society for Paediatric & Adolescent Gynaecology. Labial Reduction Surgery (Labiaplasty) on Adolescents. Position Statement. 2013.
Forster K. Labiaplasty: vaginal surgery “world’s fastest-growing cosmetic procedure”, say plastic surgeons. Independent. 2017;12:2017.
International Society of Aesthetic Plastic Surgery. The international study on aesthetic/cosmetic procedures performed in 2016. International Society of Aesthetic Plastic Surgery; 2016.
International Society of Aesthetic Plastic Surgery. The international study on aesthetic/cosmetic procedures performed in 2017. International Society of Aesthetic Plastic Surgery; 2017.
Boddy J. Civilizing women. British Crusades in Colonial Sudan. Princeton University Press; 2007.
Thomas L. Politics of the womb: women, reproduction, and the state in Kenya. Berkeley: University of California Press; 2003.
Abu-Sahlieh SAA. Circoncision masculine, circoncision féminine. Débat religieux, médical, social et juridique. Paris: L'Harmattan; 2001.
O’Neill S. Defying the law, negotiating change. The Futanke’s opposition to the national ban on FGM in Senegal London: Goldsmiths. University of London; 2013.
Hosken FP. The Hosken report: genital and sexual mutilation of females. Women’s International Network News: Lexington; 1979.
UNICEF. Changing a harmful social convention: female genital mutilation/cutting. Florence: Innocenti Research Center; 2008.
WHO, UNICEF, UNFPA. Female genital mutilation: a joint WHO/UNICEF/UNFPA statement. Geneva: World Health Organization; 1997.
UNICEF. Legislative reform to support the abandonment of female genital mutilation/cutting: UNICEF; 2010.
Nedim U. ‘Any extent’ of injury can amount to female genital mutilation. Lexology: High Court finds; 2019.
Court of Criminal Appeal. A2 v R; Magennis v R; Vaziri v R [2018] NSWCCA 174 (10 August 2018). New South Wales: Supreme Court; 2018.
Bader D, Mottier V. Femonationalism and Populist Politics: The Case of the Swiss Ban on Female Genital Mutilation: Nations and Nationalism. 2020.
Hausammann C. Condamnation pour mutilations génitales féminines commises à l’étranger. Centre suisse de compétence pour les droits humains: Berne; 2019.
Hausammann C, Bader D. Norme pénale spéciale contre les mutilations sexuelles féminines. Newsletter n°2. Centre suisse de compétence pour les droits humains: Berne; 2011.
Essén B, Johnsdotter S. Female genital mutilation in the west: traditional circumcision versus genital cosmetic surgery. Acta Obstet Gynecol Scand. 2004;83(7):611–3.
Bibbings L, Alldridge P. Sexual expression, body alteration, and the defence of consent. J Law Soc. 1993;20(3):356–70.
Sheldon S, Wilkinson S. Female genital mutilation and cosmetic surgery: regulating non-therapeutic body modification. Bioethics. 1998;12(4):263–85.
Bibbings L. Touch: socio-cultural attitudes and legal responses to body alteration. In: Bentley L, Flynn L, editors. Law and the sense. London: Pluto; 1996. p. 176–98.
Johnsdotter S, Essén B. Genitals and ethnicity: the politics of genital modifications. Reprod Health Matters. 2010;18(35):29–37.
Berer M. Cosmetic genitoplasty: it’s female genital mutilation and should be prosecuted. Br Med J. 2007;334(7608):1335.
Dustin M. Female genital mutilation/cutting in the UK: challenging the inconsistencies. Eur J Women's Stud. 2010;17(1):7–23. https://doi.org/10.1177/1350506809350857.
Shahvisi A, Why UK. Doctors should be troubled by female genital mutilation legislation. Clin Ethics. 2017;12(2):102–8. https://doi.org/10.1177/1477750916682671.
Bennett T. Beauty and the beast: analogising between cosmetic surgery and female genital mutilation. Flinders Law J. 2012;14(1):49–68.
Veale D, Daniels J. Cosmetic clitoridectomy in a 33-year-old woman. Arch Sex Behav. 2011;41(3):725–30. https://doi.org/10.1007/s10508-011-9831-4.
Bader D. Excision et nymphoplastie: les deux faces d'un même miroir sociologique. Profession Sage-Femme. 2014;203:30–2.
Asefaw F. Weibliche Genitalbeschneidung: Hintergründe, gesundheitliche Folgen und nachhaltige Prävention: Boox-Verlag; 2017.
Boddy Janice. The normal and the aberrant in female genital cutting: Shifting paradigms. Hau J Ethnogr Theory. 2016;6(2):41–69.
Earp B, Johnsdotter S. Current critiques of the WHO policy on female genital mutilation. Int J Impot Res. 2020:1–14.
Earp B, Kraus C, Bader D, Alexander S, O'Neill S, Abdulcadir J. The Brussels collaboration on bodily integrity. Medically unnecessary genital cutting and the rights of the child: moving toward consensus. Guest editorial. Am J Bioeth. 2019;19(10):17–28. https://doi.org/10.1080/15265161.2019.1643945.
Acknowledgements
The authors would like to thank Asuncion Frezsnoza-Flot for helping to fund the symposium. The symposium was funded as part of a partnership between the Université Libre de Bruxelles and the University of Lausanne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sociocultural Issues and Epidemiology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
O’Neill, S., Bader, D., Kraus, C. et al. Rethinking the Anti-FGM Zero-Tolerance Policy: from Intellectual Concerns to Empirical Challenges. Curr Sex Health Rep 12, 266–275 (2020). https://doi.org/10.1007/s11930-020-00299-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11930-020-00299-9