Abstract
Purpose of Review
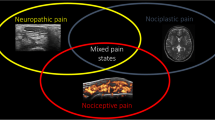
Chronic pain in osteoarthritis (OA) is characterized by pain sensitization, which involves both peripheral and central mechanisms. Studies suggest synovial macrophage and spinal microglia are implicated in pain sensitization in OA. We, therefore, reviewed the evidence of whether synovial macrophage and spinal microglia facilitated pain sensitization at diverse levels and how this event occurred in OA.
Recent Findings
Peripherally, joint inflammation is now believed to be a source of OA-related pain. Synovial macrophages accumulate in OA inflamed synovium and display a pro-inflammatory phenotype. Abundant macrophage-derived pro-inflammatory cytokines and other pain-causing substance facilitate hyperexcitation of primary sensory neuron in OA-related pain. Thus, activated synovial macrophage was considered a predictor for phenotyping of OA pain clinically. In response to affected joint-derived strong nociception, aberrant neuronal excitability is often associated with the hyperactivity of microglia in the spinal dorsal horn, thereby leading to central sensitization.
Summary
Hyperactivity of synovial macrophage and spinal microglia underlies the mechanisms of pain sensitization at the peripheral and central level in OA. This concept provides not only a clinically relevant strategy for identifying the phenotype of OA-related pain but also has the potential to develop individualized interventions for OA, particularly in those patients with hyperactivity of macrophage and microglia.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pan F, Jones G. Clinical perspective on pain and pain phenotypes in osteoarthritis. Curr Rheumatol Rep. 2018;20(12):79. https://doi.org/10.1007/s11926-018-0796-3.
Thomas E, Peat G, Croft P. Defining and mapping the person with osteoarthritis for population studies and public health. Rheumatology (Oxford). 2014;53(2):338–45. https://doi.org/10.1093/rheumatology/ket346.
Yu SPC, Hunter DJ. Emerging drugs for the treatment of knee osteoarthritis. Expert Opin Emerg Dr. 2015;20(3):361–78. https://doi.org/10.1517/14728214.2015.1037275.
Cohen E, Lee YC. A mechanism-based approach to the management of osteoarthritis pain. Curr Osteoporos Rep. 2015;13(6):399–406. https://doi.org/10.1007/s11914-015-0291-y.
Malfait AM, Schnitzer TJ. Towards a mechanism-based approach to pain management in osteoarthritis. Nat Rev Rheumatol. 2013;9(11):654–64. https://doi.org/10.1038/nrrheum.2013.138.
Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr Cartil. 2013;21(1):16–21. https://doi.org/10.1016/j.joca.2012.11.012.
Cardoso JS, Riley JL 3rd, Glover T, Sibille KT, Bartley EJ, Goodin BR, et al. Experimental pain phenotyping in community-dwelling individuals with knee osteoarthritis. Pain. 2016;157(9):2104–14. https://doi.org/10.1097/j.pain.0000000000000625.
Frey-Law LA, Bohr NL, Sluka KA, Herr K, Clark CR, Noiseux NO, et al. Pain sensitivity profiles in patients with advanced knee osteoarthritis. Pain. 2016;157(9):1988–99. https://doi.org/10.1097/j.pain.0000000000000603.
Osgood E, Trudeau JJ, Eaton TA, Jensen MP, Gammaitoni A, Simon LS, et al. Development of a bedside pain assessment kit for the classification of patients with osteoarthritis. Rheumatol Int. 2015;35(6):1005–13. https://doi.org/10.1007/s00296-014-3191-z.
Miller RJ, Malfait AM, Miller RE. The innate immune response as a mediator of osteoarthritis pain. Osteoarthr Cartil. 2020;28(5):562–71. https://doi.org/10.1016/j.joca.2019.11.006.
Zhang Y, Nevitt M, Niu J, Lewis C, Torner J, Guermazi A, et al. Fluctuation of knee pain and changes in bone marrow lesions, effusions, and synovitis on magnetic resonance imaging. Arthritis Rheum. 2011;63(3):691–9. https://doi.org/10.1002/art.30148.
Neogi T, Guermazi A, Roemer F, Nevitt MC, Scholz J, Arendt-Nielsen L, et al. Association of joint inflammation with pain sensitization in knee osteoarthritis: the multicenter osteoarthritis study. Arthritis Rheumatol. 2016;68(3):654–61. https://doi.org/10.1002/art.39488.
Kraus VB, McDaniel G, Huebner JL, Stabler TV, Pieper CF, Shipes SW, et al. Direct in vivo evidence of activated macrophages in human osteoarthritis. Osteoarthr Cartil. 2016;24(9):1613–21. https://doi.org/10.1016/j.joca.2016.04.010.
Haraden CA, Huebner JL, Hsueh MF, Li YJ, Kraus VB. Synovial fluid biomarkers associated with osteoarthritis severity reflect macrophage and neutrophil related inflammation. Arthritis Res Ther. 2019;21(1):146. https://doi.org/10.1186/s13075-019-1923-x.
Griffin TM, Scanzello CR. Innate inflammation and synovial macrophages in osteoarthritis pathophysiology. Clin Exp Rheumatol. 2019;37(Suppl 120(5)):57–63.
Zhang H, Lin C, Zeng C, Wang Z, Wang H, Lu J, et al. Synovial macrophage M1 polarisation exacerbates experimental osteoarthritis partially through R-spondin-2. Ann Rheum Dis. 2018;77(10):1524–34. https://doi.org/10.1136/annrheumdis-2018-213450.
Ji RR, Berta T, Nedergaard M. Glia and pain: is chronic pain a gliopathy? Pain. 2013;154(Suppl 1):S10–28. https://doi.org/10.1016/j.pain.2013.06.022.
Tran PB, Miller RE, Ishihara S, Miller RJ, Malfait AM. Spinal microglial activation in a murine surgical model of knee osteoarthritis. Osteoarthr Cartil. 2017;25(5):718–26. https://doi.org/10.1016/j.joca.2016.09.007.
Yang JL, Xu B, Li SS, Zhang WS, Xu H, Deng XM, et al. Gabapentin reduces CX3CL1 signaling and blocks spinal microglial activation in monoarthritic rats. Mol Brain. 2012;5:18. https://doi.org/10.1186/1756-6606-5-18.
Yusup A, Kaneko H, Liu L, Ning L, Sadatsuki R, Hada S, et al. Bone marrow lesions, subchondral bone cysts and subchondral bone attrition are associated with histological synovitis in patients with end-stage knee osteoarthritis: a cross-sectional study. Osteoarthr Cartil. 2015;23(11):1858–64. https://doi.org/10.1016/j.joca.2015.05.017.
Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. The Lancet. 2005;365(9463):965–73. https://doi.org/10.1016/s0140-6736(05)71086-2.
Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. https://doi.org/10.1186/1471-2474-9-116.
Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27(6):1513–7.
Neogi T, Frey-Law L, Scholz J, Niu J, Arendt-Nielsen L, Woolf C, et al. Sensitivity and sensitisation in relation to pain severity in knee osteoarthritis: trait or state? Ann Rheum Dis. 2015;74(4):682–8. https://doi.org/10.1136/annrheumdis-2013-204191.
Misra D, Fielding RA, Felson DT, Niu J, Brown C, Nevitt M, et al. Risk of knee osteoarthritis with obesity, sarcopenic obesity, and sarcopenia. Arthritis Rheumatol. 2019;71(2):232–7. https://doi.org/10.1002/art.40692.
Syx D, Tran PB, Miller RE, Malfait AM. Peripheral mechanisms contributing to osteoarthritis pain. Curr Rheumatol Rep. 2018;20(2):9. https://doi.org/10.1007/s11926-018-0716-6.
Zhang H, Cai D, Bai X. Macrophages regulate the progression of osteoarthritis. Osteoarthr Cartil. 2020;28(5):555–61. https://doi.org/10.1016/j.joca.2020.01.007.
Blom AB, van Lent PL, Libregts S, Holthuysen AE, van der Kraan PM, van Rooijen N, et al. Crucial role of macrophages in matrix metalloproteinase-mediated cartilage destruction during experimental osteoarthritis: involvement of matrix metalloproteinase 3. Arthritis Rheum. 2007;56(1):147–57. https://doi.org/10.1002/art.22337.
. Sakurai Y, Fujita M, Kawasaki S, Sanaki T, Yoshioka T, Higashino K, et al. Contribution of synovial macrophages to rat advanced osteoarthritis pain resistant to cyclooxygenase inhibitors. Pain. 2019;160(4):895–907. https://doi.org/10.1097/j.pain.0000000000001466This study confirms a key role of synovial macrophage in pain of OA murine models.
Bondeson J, Wainwright SD, Lauder S, Amos N, Hughes CE. The role of synovial macrophages and macrophage-produced cytokines in driving aggrecanases, matrix metalloproteinases, and other destructive and inflammatory responses in osteoarthritis. Arthritis Res Ther. 2006;8(6):R187. https://doi.org/10.1186/ar2099.
Sambamurthy N, Zhou C, Nguyen V, Smalley R, Hankenson KD, Dodge GR, et al. Deficiency of the pattern-recognition receptor CD14 protects against joint pathology and functional decline in a murine model of osteoarthritis. PLoS One. 2018;13(11):e0206217. https://doi.org/10.1371/journal.pone.0206217.
Blom AB, van Lent PL, Holthuysen AE, van der Kraan PM, Roth J, van Rooijen N, et al. Synovial lining macrophages mediate osteophyte formation during experimental osteoarthritis. Osteoarthr Cartil. 2004;12(8):627–35. https://doi.org/10.1016/j.joca.2004.03.003.
Daghestani HN, Pieper CF, Kraus VB. Soluble macrophage biomarkers indicate inflammatory phenotypes in patients with knee osteoarthritis. Arthritis Rheumatol. 2015;67(4):956–65. https://doi.org/10.1002/art.39006.
. Culemann S, Gruneboom A, Nicolas-Avila JA, Weidner D, Lammle KF, Rothe T, et al. Locally renewing resident synovial macrophages provide a protective barrier for the joint. Nature. 2019;572(7771):670–5. https://doi.org/10.1038/s41586-019-1471-1This study provides a critical description of synovial macrophages are a mixed population, consisting of different origins and function phenotypes.
Utomo L, van Osch GJ, Bayon Y, Verhaar JA, Bastiaansen-Jenniskens YM. Guiding synovial inflammation by macrophage phenotype modulation: an in vitro study towards a therapy for osteoarthritis. Osteoarthr Cartil. 2016;24(9):1629–38. https://doi.org/10.1016/j.joca.2016.04.013.
Tsuneyoshi Y, Tanaka M, Nagai T, Sunahara N, Matsuda T, Sonoda T, et al. Functional folate receptor beta-expressing macrophages in osteoarthritis synovium and their M1/M2 expression profiles. Scand J Rheumatol. 2012;41(2):132–40. https://doi.org/10.3109/03009742.2011.605391.
Utomo L, Bastiaansen-Jenniskens YM, Verhaar JA, van Osch GJ. Cartilage inflammation and degeneration is enhanced by pro-inflammatory (M1) macrophages in vitro, but not inhibited directly by anti-inflammatory (M2) macrophages. Osteoarthr Cartil. 2016;24(12):2162–70. https://doi.org/10.1016/j.joca.2016.07.018.
Fahy N, de Vries-van Melle ML, Lehmann J, Wei W, Grotenhuis N, Farrell E, et al. Human osteoarthritic synovium impacts chondrogenic differentiation of mesenchymal stem cells via macrophage polarisation state. Osteoarthr Cartil. 2014;22(8):1167–75. https://doi.org/10.1016/j.joca.2014.05.021.
Hu Y, Gui Z, Zhou Y, Xia L, Lin K, Xu Y. Quercetin alleviates rat osteoarthritis by inhibiting inflammation and apoptosis of chondrocytes, modulating synovial macrophages polarization to M2 macrophages. Free Radic Biol Med. 2019;145:146–60. https://doi.org/10.1016/j.freeradbiomed.2019.09.024.
Tu J, Hong W, Guo Y, Zhang P, Fang Y, Wang X, et al. Ontogeny of synovial macrophages and the roles of synovial macrophages from different origins in arthritis. Front Immunol. 2019;10:1146. https://doi.org/10.3389/fimmu.2019.01146.
He XH, Zang Y, Chen X, Pang RP, Xu JT, Zhou X, et al. TNF-alpha contributes to up-regulation of Nav1.3 and Nav1.8 in DRG neurons following motor fiber injury. Pain. 2010;151(2):266–79. https://doi.org/10.1016/j.pain.2010.06.005.
Ji RR, Xu ZZ, Gao YJ. Emerging targets in neuroinflammation-driven chronic pain. Nat Rev Drug Discov. 2014;13(7):533–48. https://doi.org/10.1038/nrd4334.
Inglis JJ, Nissim A, Lees DM, Hunt SP, Chernajovsky Y, Kidd BL. The differential contribution of tumour necrosis factor to thermal and mechanical hyperalgesia during chronic inflammation. Arthritis Res Ther. 2005;7(4):R807–16. https://doi.org/10.1186/ar1743.
Segond von Banchet G, Boettger MK, Fischer N, Gajda M, Brauer R, Schaible HG. Experimental arthritis causes tumor necrosis factor-alpha-dependent infiltration of macrophages into rat dorsal root ganglia which correlates with pain-related behavior. Pain. 2009;145(1-2):151–9. https://doi.org/10.1016/j.pain.2009.06.002.
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7(1):33–42. https://doi.org/10.1038/nrrheum.2010.196.
Attur M, Belitskaya-Levy I, Oh C, Krasnokutsky S, Greenberg J, Samuels J, et al. Increased interleukin-1beta gene expression in peripheral blood leukocytes is associated with increased pain and predicts risk for progression of symptomatic knee osteoarthritis. Arthritis Rheum. 2011;63(7):1908–17. https://doi.org/10.1002/art.30360.
Obreja O, Rathee PK, Lips KS, Distler C, Kress M. IL-1 beta potentiates heat-activated currents in rat sensory neurons: involvement of IL-1RI, tyrosine kinase, and protein kinase C. FASEB J. 2002;16(12):1497–503. https://doi.org/10.1096/fj.02-0101com.
Binshtok AM, Wang H, Zimmermann K, Amaya F, Vardeh D, Shi L, et al. Nociceptors are interleukin-1beta sensors. J Neurosci. 2008;28(52):14062–73. https://doi.org/10.1523/JNEUROSCI.3795-08.2008.
Miller RE, Tran PB, Das R, Ghoreishi-Haack N, Ren D, Miller RJ, et al. CCR2 chemokine receptor signaling mediates pain in experimental osteoarthritis. Proc Natl Acad Sci U S A. 2012;109(50):20602–7. https://doi.org/10.1073/pnas.1209294110.
Belkouch M, Dansereau MA, Reaux-Le Goazigo A, Van Steenwinckel J, Beaudet N, Chraibi A, et al. The chemokine CCL2 increases Nav1.8 sodium channel activity in primary sensory neurons through a Gbetagamma-dependent mechanism. J Neurosci. 2011;31(50):18381–90. https://doi.org/10.1523/JNEUROSCI.3386-11.2011.
Kao DJ, Li AH, Chen JC, Luo RS, Chen YL, Lu JC, et al. CC chemokine ligand 2 upregulates the current density and expression of TRPV1 channels and Nav1.8 sodium channels in dorsal root ganglion neurons. J Neuroinflammation. 2012;9:189. https://doi.org/10.1186/1742-2094-9-189.
. Soni A, Wanigasekera V, Mezue M, Cooper C, Javaid MK, Price AJ, et al. Central sensitization in knee osteoarthritis: relating presurgical brainstem neuroimaging and PainDETECT-based patient stratification to arthroplasty outcome. Arthritis Rheumatol. 2019;71(4):550–60. https://doi.org/10.1002/art.40749This study provides strong evidence of centrally mediated pain mechanisms in OA patients by MRI neuroimaging as well as neuropathic-like pain symptoms.
Reckziegel D, Raschke F, Cottam WJ, Auer DP. Cingulate GABA levels inversely correlate with the intensity of ongoing chronic knee osteoarthritis pain. Mol Pain. 2016;12:174480691665069. https://doi.org/10.1177/1744806916650690.
Liu J, Chen L, Tu Y, Chen X, Hu K, Tu Y, et al. Different exercise modalities relieve pain syndrome in patients with knee osteoarthritis and modulate the dorsolateral prefrontal cortex: a multiple mode MRI study. Brain Behav Immun. 2019;82:253–63. https://doi.org/10.1016/j.bbi.2019.08.193.
Chen G, Zhang YQ, Qadri YJ, Serhan CN, Ji RR. Microglia in pain: detrimental and protective roles in pathogenesis and resolution of pain. Neuron. 2018;100(6):1292–311. https://doi.org/10.1016/j.neuron.2018.11.009.
Sagar DR, Burston JJ, Hathway GJ, Woodhams SG, Pearson RG, Bennett AJ, et al. The contribution of spinal glial cells to chronic pain behaviour in the monosodium iodoacetate model of osteoarthritic pain. Mol Pain. 2011;7:88. https://doi.org/10.1186/1744-8069-7-88.
Ogbonna AC, Clark AK, Gentry C, Hobbs C, Malcangio M. Pain-like behaviour and spinal changes in the monosodium iodoacetate model of osteoarthritis in C57Bl/6 mice. Eur J Pain. 2013;17(4):514–26. https://doi.org/10.1002/j.1532-2149.2012.00223.x.
Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology. 2018;129(2):343–66. https://doi.org/10.1097/ALN.0000000000002130.
Ji RR, Donnelly CR, Nedergaard M. Astrocytes in chronic pain and itch. Nat Rev Neurosci. 2019;20(11):667–85. https://doi.org/10.1038/s41583-019-0218-1.
Nieto FR, Clark AK, Grist J, Hathway GJ, Chapman V, Malcangio M. Neuron-immune mechanisms contribute to pain in early stages of arthritis. J Neuroinflammation. 2016;13(1):96. https://doi.org/10.1186/s12974-016-0556-0.
Fernandez-Zafra T, Gao T, Jurczak A, Sandor K, Hore Z, Agalave NM, et al. Exploring the transcriptome of resident spinal microglia after collagen antibody-induced arthritis. Pain. 2019;160(1):224–36. https://doi.org/10.1097/j.pain.0000000000001394.
Inoue K, Tsuda M. Microglia in neuropathic pain: cellular and molecular mechanisms and therapeutic potential. Nat Rev Neurosci. 2018;19(3):138–52. https://doi.org/10.1038/nrn.2018.2.
Upadhyay J, Baker SJ, Rajagovindan R, Hart M, Chandran P, Hooker BA, et al. Pharmacological modulation of brain activity in a preclinical model of osteoarthritis. Neuroimage. 2013;64:341–55. https://doi.org/10.1016/j.neuroimage.2012.08.084.
Taylor AM, Castonguay A, Taylor AJ, Murphy NP, Ghogha A, Cook C, et al. Microglia disrupt mesolimbic reward circuitry in chronic pain. J Neurosci. 2015;35(22):8442–50. https://doi.org/10.1523/JNEUROSCI.4036-14.2015.
Ni HD, Yao M, Huang B, Xu LS, Zheng Y, Chu YX, et al. Glial activation in the periaqueductal gray promotes descending facilitation of neuropathic pain through the p38 MAPK signaling pathway. J Neurosci Res. 2016;94(1):50–61. https://doi.org/10.1002/jnr.23672.
Clark AK, Yip PK, Grist J, Gentry C, Staniland AA, Marchand F, et al. Inhibition of spinal microglial cathepsin S for the reversal of neuropathic pain. Proc Natl Acad Sci U S A. 2007;104(25):10655–60. https://doi.org/10.1073/pnas.0610811104.
Clark AK, Yip PK, Malcangio M. The liberation of fractalkine in the dorsal horn requires microglial cathepsin S. J Neurosci. 2009;29(21):6945–54. https://doi.org/10.1523/JNEUROSCI.0828-09.2009.
Taves S, Berta T, Chen G, Ji RR. Microglia and spinal cord synaptic plasticity in persistent pain. Neural Plast. 2013;2013:753656–10. https://doi.org/10.1155/2013/753656.
Berta T, Qadri YJ, Chen G, Ji RR. Microglial signaling in chronic pain with a special focus on caspase 6, p38 MAP kinase, and sex dependence. J Dent Res. 2016;95(10):1124–31. https://doi.org/10.1177/0022034516653604.
Kawasaki Y, Zhang L, Cheng JK, Ji RR. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci. 2008;28(20):5189–94. https://doi.org/10.1523/JNEUROSCI.3338-07.2008.
Funding
This study was supported by Natural Science Foundation of China (No. 81703524).
Author information
Authors and Affiliations
Contributions
TP and DW wrote this paper. FP, SH, and WG gave some critical comments and reviewed this paper. SH drew the figure.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Chronic Pain
Rights and permissions
About this article
Cite this article
Pan, Tt., Pan, F., Gao, W. et al. Involvement of Macrophages and Spinal Microglia in Osteoarthritis Pain. Curr Rheumatol Rep 23, 29 (2021). https://doi.org/10.1007/s11926-021-00997-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s11926-021-00997-w